Thyroid and Parathyroid Disease
Nicholas P.W. Coe
Thyroid Disease
Patricia Arnold is a 35-year-old woman with an asymptomatic neck mass, which she first noticed 3 weeks ago. Her history is unremarkable except for childhood tonsillectomy and adenoidectomy. She is taking birth control pills and has no known drug allergies. A family history reveals that a maternal aunt had Graves’ disease; no other members had thyroid disease. The patient has a 20-pack-year smoking history and has one to two alcoholic drinks per week. A review of various other systems does not reveal any significant findings.
The physical examination reveals a healthy-looking woman in no acute distress. Her vital signs are normal: temperature, 36.5°C; blood pressure, 135/70 mm Hg, pulse rate 80 beats per minute; and respiratory rate, 18 breaths per minute. The head and neck examination reveals no exophthalmos, lid lag, or intraoral lesions; the neck mass is not associated with any cervical adenopathy. The lungs are clear to auscultation; the heart rate and rhythm are regular and without murmurs; and the abdominal examination is normal. Neurologic function is intact, and findings are nonfocal.
What is the differential diagnosis for a neck mass?
View Answer
Approximately 50% of neck masses that persist beyond 3 to 4 weeks originate from the thyroid gland. Inflammatory lesions, nonthyroidal malignant lesions, and congenital lesions account for the remaining 50%. Malignant lesions, such as lymphoma, carcinoma of the thyroid, and metastatic tumor from another head and neck site, are most common in adults, whereas inflammatory lesions are most common in children. Congenital lesions, such as thyroglossal duct and branchial cleft cysts, are also very common in children.
The 3-cm mass, which appears to be originating from the right thyroid lobe, is firm and not tender. There is no associated fever, chills, pressure, or symptoms of thyrotoxicity.
What are the symptoms of thyrotoxicity?
View Answer
Heat intolerance, weight loss with increased appetite, tachycardia (sleeping pulse rate faster than 80 beats per minute), atrial arrhythmias, congestive heart failure (especially in the elderly), hyperkinetic behavior, emotional instability, insomnia, fatigue, muscle weakness, amenorrhea, and diarrhea are all symptoms of thyrotoxicity.
What does thyroid mean and where is the thyroid gland?
View Answer
The word thyroid is derived from the Greek thyreos, or shield. The thyroid gland originates from two sites. The tuberculum impar at the base of the vallate papillae of the tongue forms the foramen cecum. The thyroid tissue descends into the neck along the line of the thyroglossal duct. The lateral component, which contributes the calcitonin-producing C cells, is derived from the fourth pharyngeal pouch.
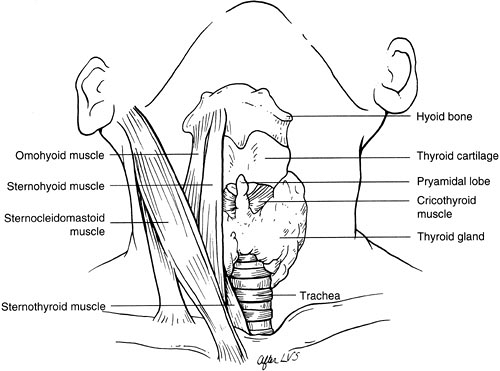
The mature thyroid gland, which weighs about 20 g, drapes over the anterolateral aspect of the upper trachea just below the cricoid cartilage. The two lobes, connected by the isthmus, lie along the sides of the larynx and trachea, extending up to the level of the middle of the thyroid cartilage. The pyramidal lobe is a diverticulum extending upward from the isthmus. These lobes are between the trachea medially and the carotid sheaths and sternocleidomastoid muscles laterally; the strap muscles lie anterior to the thyroid lobes. The parathyroid glands and the recurrent laryngeal nerves are on the posterior surface of the lateral lobes of the thyroid gland. The nerves are typically found in the tracheoesophageal groove. A thin, fibrous capsule surrounds the thyroid gland.
What are the risk factors for thyroid malignancy?
View Answer
A careful personal and family history helps determine whether a patient has any special risk factors for thyroid malignancy. Low-dose radiation exposure (300 to 1000 cGy) is associated with well-differentiated thyroid cancer (1). More than 90% of thyroid carcinomas in patients with a history of irradiation are papillary. Low doses of radiation were commonly used between 1945 and 1955 to treat an enlarged thymus. Radiation was also used from the 1930s to the 1960s to treat diseases such as ringworm, keloids, capillary hemangiomata, and tubercular lymphadenopathy. In more recent times, exposure to radiation from the Chernobyl nuclear accident in April 1986 placed residents of the Ukraine, the Gomel region of Belorussia, and possibly other widespread areas of central Europe at high risk for developing thyroid malignancy. Immigrants from these areas now live in many parts of the Unites States.
A higher incidence of malignancy is also found in patients with a thyroid mass who are younger than 20 years, patients older than 60 years, and men than in the general population. A family history of thyroid disease is often present, especially in female relatives; this has little bearing on the treatment of the patient, but the possibility of the familial form of thyroid carcinoma should always be kept in mind.
Significant findings on physical examination include a hard mass with poorly defined borders, cervical adenopathy adjacent to the thyroid or in the posterior triangle, fixation of the gland, and vocal cord paralysis.
How should a thyroid mass be evaluated?
View Answer
The main features that have to be determined are (a) whether the mass is malignant and (b) whether it is hyperfunctioning. The patient should also be questioned about symptoms of compression such as difficulty swallowing or a choking sensation.
If a patient has no symptoms or signs of thyrotoxicosis, the simplest and most economical way to begin the workup is to determine the thyroid-stimulating hormone (TSH) level and obtain a fine-needle aspirate (FNA) of the thyroid with a 21- to 25-gauge needle. If the TSH level is normal, the patient is not likely to be thyrotoxic; if there is any doubt, determine thyroxine (T4) and triiodothyronine (T3) levels. Ultrasonography may be helpful in a patient whose neck is difficult to examine, but ultrasonography has largely been superseded by FNA for distinguishing between cystic and solid lesions. Radioactive scanning with iodine 123 (123I) or technetium 99m (99mTc)-labeled compounds can differentiate among cold lesions (those with low or no radioisotope uptake), warm lesions (those that take up the radioisotope but show no evidence of thyrotoxicosis), and hot lesions (those that concentrate the isotope to a greater degree than the remaining thyroid). Cold lesions raise suspicion of malignancy and are always evaluated with FNA. Warm and hot lesions are only rarely malignant and do not require FNA.
What are the advantages and disadvantages of needle biopsy in the evaluation of a thyroid nodule?
View Answer
FNA biopsy is safe, fast, sensitive, and cost effective, and it can be performed on an outpatient basis. Papillary, medullary, and anaplastic carcinomas can be diagnosed with this method. Certain elements, such as atypia and a microfollicular pattern, suggest malignancy, whereas a macrofollicular pattern or abundant colloid is more consistent with a benign lesion. However, this technique does not allow differentiation between malignant and benign follicular tumors because that distinction is made on the basis of vascular and/or capsular invasion, features that cannot be determined from an FNA.
What is the therapeutic approach if the FNA indicates that the lesion is benign?
View Answer
If an experienced thyroid cytopathologist considers the aspirate to be benign, the patient is offered the option of treatment with suppressive doses of L-thyroxine, and the biopsy is repeated in 3 to 6 months.
What is the mechanism of thyroxine suppression?
View Answer
The activity of the thyroid gland is regulated by the central nervous system (CNS) and by the serum level of iodine. The hypothalamus secretes thyrotropin-releasing hormone, which stimulates the anterior pituitary gland to release TSH. TSH stimulates the production and release of thyroid hormone and induces hyperplasia (TSH is also known as thyrotropin) and vascularity of the thyroid gland.
Secretion of TSH is inhibited by the negative feedback effect of endogenous or exogenous thyroid hormone. Thyroid suppression may be given in doses of L-thyroxine sufficient to suppress TSH to barely detectable levels. This decrease in TSH may shrink the lesion by inhibiting the hyperplastic effect of TSH. There is, however, a significant association with increased osteoporosis and the onset of atrial fibrillation in these patients. Some endocrinologists will use exogenous thyroid hormone to suppress TSH only to low levels of normal or just below normal because of this major concern. The thyroid tumors do not usually shrink but the patient should be given the option to try this treatment modality.
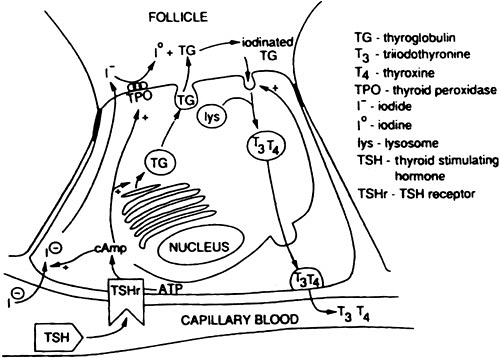
How is thyroid hormone formed?
View Answer
The principal function of the thyroid gland is to produce thyroid hormone, which regulates cellular metabolism. The production of thyroid hormone depends on dietary iodine, which is actively transported from the plasma into the thyroid where it is oxidized and rapidly incorporated into a macromolecule, thyroglobulin. Tyrosine molecules are iodinated at one (monoiodotyrosine) or two (diiodotyrosine) sites, and these are subsequently coupled to form T3 and T4.
Hydrolysis of thyroglobulin releases T3 and T4 into the circulation, but thyroglobulin is not released except in disease states (Fig. 4.1). The active thyroid hormones attach to a plasma protein, thyroxine-binding globulin. In the plasma, the T4-T3 ratio ranges from 10:1 to 20:1. In the periphery, T4 is converted to T3, which enters the tissues quickly because of its lower affinity for protein and is three to four times as active as T4. The half-life of T4 (7 to 8 days) is longer than that of T3 (3 days). The metabolic functions of thyroid hormone include increased calorigenesis, increased protein synthesis, and altered carbohydrate and lipid metabolism.
What are the indications for surgery in thyroid disease?
View Answer
Surgical treatment of thyroid disease should be considered for the following conditions:
Malignancy
Carcinoma proved with FNA
A lesion suspicious for carcinoma on FNA
As prophylaxis for patients with familial thyroid cancer
Nonmalignant thyroid mass
Toxic multinodular goiter
Solitary toxic nodule
Graves’ disease
Compression symptoms from a thyroid mass
Ms. Arnold’s ultrasound examination reveals a solid nodule. A 123I scan reveals a cold nodule, and FNA reveals cells suggestive of papillary carcinoma.
What are the pathologic types of thyroid cancers?
View Answer
Four main types of thyroid cancers can be distinguished according to their pathology: papillary, follicular, medullary, and anaplastic. More than 90% of all thyroid cancers are papillary and follicular (well-differentiated) carcinomas.
Papillary carcinomas are well-differentiated lesions. The peak incidence is in the third to fourth decades, and women are affected three times as often as men. Papillary carcinomas contain concentric layers of calcium called psammoma bodies. Papillary cancers are the slowest-growing thyroid cancers, and they spread through the lymphatic system. When thyroid tissue is found in the posterior triangle of the neck, the condition has been referred to as lateral aberrant thyroid. This actually represents a papillary cancer that has metastasized to a lymph node. Accessory thyroid tissue, separate from the thyroid, can be found in the central compartment of the neck. Usually this does not represent metastatic thyroid cancer but rather an embryonic rest of thyroid tissue. The multicentricity rate of papillary thyroid cancer is 80% on microscopic examination, but probably less than 5% have a clinical effect. Papillary metastases usually concentrate iodine and can be treated with radioiodine. Some papillary thyroid cancers show features of follicular cancer and are known as follicular variants of papillary cancer. They behave in the same way as papillary cancers.
Follicular carcinomas are generally also well-differentiated tumors. Pure follicular cancers, as distinct from follicular variants of papillary cancer, differ from papillary tumors in that they exhibit less multicentricity and are more likely to spread hematogenously to bone, lung, and liver. Follicular metastases may concentrate iodine, but to a lesser degree than papillary lesions. When iodine uptake is demonstrated, they can be treated with radioiodine.
Medullary carcinomas are less common tumors, comprising 3% to 5% of thyroid cancers. They are calcitonin-producing tumors that originate from the C cells; amyloid deposits in the stroma of the tumor are diagnostic. Bilateral multicentricity is more commonly found in familial cases but is still common in the sporadic variety. Medullary cancers occur in families as components of both multiple endocrine neoplasia (MEN) type II and the familial medullary carcinoma syndrome (see Chapter 23). MEN type IIA, or Sipple’s syndrome, also includes pheochromocytomas and hyperparathyroidism (HPT). MEN type IIB is a less common form that includes mucosal neuromas, ganglioneuroma of the bowel, and a marfanoid appearance; HPT is rare. An elevated serum calcitonin level is diagnostic of medullary carcinoma and is also a useful screening tool for familial transmission and to monitor recurrence. Evaluation of point mutations in the Ret protooncogene is part of the workup of these patients and their families (2).
Anaplastic carcinomas account for less than 5% of thyroid cancers and occur later in life than the other types. These cancers are characterized by extremely rapid and widespread growth. Patients present with a sometimes painful and enlarged thyroid gland. These tumors are highly aggressive and are associated with a very short life expectancy.
What is the treatment for a patient with a presentation such as Ms. Arnold’s if the FNA indicates papillary carcinoma?
View Answer
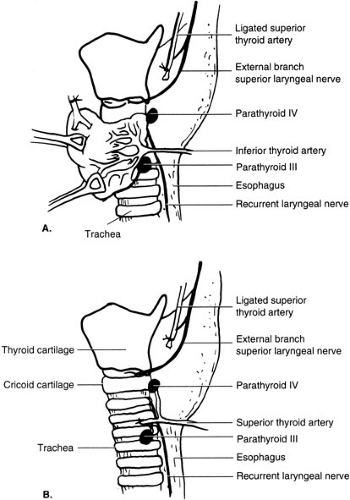
The lesion must be excised, but the extent of resection—thyroid lobectomy alone versus total thyroidectomy (Fig. 4.2)—has been debated extensively (3,4). Lobectomy is advocated by some because it minimizes the operative risks of nerve and parathyroid injury; multicentric disease rarely becomes a clinical problem; and thyroid cancers in general are not very aggressive. More extensive surgical ablation (total thyroidectomy) is promoted because it allows postoperative scanning with 131I for metastatic disease because no normal thyroid tissue (which concentrates iodine more vigorously than papillary or follicular metastases) remains in the neck; it facilitates follow-up with thyroglobulin levels; and it eliminates recurrence caused by multicentricity. One large study has shown a survival benefit for total thyroidectomy over lobectomy (5). A majority of endocrine surgeons favor total thyroidectomy for lesions larger than 2 to 3 cm.
After total thyroidectomy, L-thyroxine is given for life in doses sufficient to maintain normal levels of TSH. Radioiodine is used to ablate any residual functional thyroid tissue in the neck after thyroidectomy and to destroy widespread metastases. Improved survival was demonstrated after treatment with total thyroidectomy, radioiodine ablation, and TSH suppression for life in a study of 1355 patients who were followed for 40 years (5,6).
What is the treatment if the FNA shows atypical follicular cells?
View Answer
The treatment decision in this instance continues to be difficult. The question is whether this tumor is a follicular adenoma, follicular hyperplasia, follicular carcinoma, or a follicular variant of papillary carcinoma. In addition, malignancy cannot be determined from intraoperative frozen sections (7), which adds to the uncertainty of the diagnosis. When the pathologic interpretation is that the lesion is a follicular carcinoma, the debate over the extent of operative resection is similar to that for papillary carcinoma. Advocates of total thyroidectomy for well-differentiated thyroid carcinoma recommend this procedure for lesions that cytology suggests are malignant and for lesions larger than 3 cm. If the cytology is indeterminate, generally a lobectomy is performed followed later by completion thyroidectomy if the permanent sections show malignancy. The surgeon and patient must balance the risk of a total thyroidectomy for possibly benign disease against the risk of further anesthesia and another procedure.
What are Hürthle cell carcinomas?
View Answer
Hürthle cell carcinomas are aggressive variants of follicular cell origin. As with follicular carcinomas, capsular or vascular invasion by the tumor indicates malignancy, but some Hürthle cell tumors behave in a malignant fashion even without these pathologic features. Size appears to be an important criterion. As a general rule, lesions less than 3 cm in diameter behave benignly, whereas those larger than 6 cm have tendency to behave as a malignancy (8).
How are medullary carcinomas treated?
View Answer
Medullary carcinomas are aggressive lesions that are markedly multicentric and that commonly metastasize to the lymph nodes. Total thyroidectomy with a central node dissection is performed for disease limited to the thyroid (9). A unilateral or bilateral modified radical neck dissection is indicated when metastatic disease is suspected because of elevated calcitonin levels and nodes that are either palpable or demonstrated by ultrasound and FNA studies to contain metastatic disease. Development of medullary thyroid cancer in patients with MEN II is virtually 100% and prophylactic total thyroidectomy at an early age is recommended in all these patients.
How are anaplastic carcinomas treated?
View Answer
Anaplastic carcinomas are characterized by extremely rapid growth and a very poor prognosis. Thyroidectomy does not improve the prognosis and is performed only to prevent airway compression. Chemotherapy and radiation therapy may offer some benefit as palliation (10).
Ms. Arnold is scheduled for neck exploration and thyroid resection for a papillary carcinoma.
What are the main steps in a thyroidectomy?
View Answer
General endotracheal anesthesia is induced, and the neck is extended. A curvilinear transverse incision is made in the line of a natural skin crease just below the cricoid cartilage over the thyroid isthmus. The incision is carried through the skin, subcutaneous tissue, platysma (innervated by the facial nerve), and cervical fascia overlying the pretracheal muscles and anterior jugular veins. After the subplatysmal flaps are developed, the cervical fascia is opened in the midline. The strap muscles (sternohyoid and sternothyroid) are separated. They are only divided for very large lesions. If the tumor infiltrates the sternothyroid muscle, the muscle should be resected en bloc with the thyroid (Fig. 4.3).
What are the characteristics of the blood supply to the thyroid gland?
View Answer
The thyroid has an abundant arterial blood supply from the superior thyroid arteries, which arise as the first branch of the external carotid arteries, and the inferior thyroid arteries, which arise from the thyrocervical trunks of the subclavian artery. There is no middle thyroid artery. Although the thyroid ima, an inferior artery that is said to arise from the arch of the aorta, is mentioned in many texts, it is rarely if ever found. The venous drainage consists of paired superior, inferior, and middle thyroid veins (Fig. 4.2).
The patient undergoes total thyroidectomy for treatment of a papillary carcinoma.
What are the complications of thyroidectomy?
How can that happen?
View Answer
With an experienced thyroid surgeon and the use of magnification (loupes), this complication is infrequent. The nerve is most vulnerable at the level of the two upper tracheal rings, where the middle portion of the thyroid lobe is attached to the tracheal cartilage by the suspensory ligament of Berry. The nerve is usually posterior to this ligament; however, variations in position occur and the nerve may be displaced by the thyroid mass.
What happens if the recurrent laryngeal nerve is injured?
View Answer
The recurrent laryngeal nerve is motor to all the muscles of the larynx except the cricothyroid. Therefore, injury results in vocal cord paralysis, and the affected vocal cord assumes a paramedian position. In most cases, nerve injury is an indirect result of adjacent dissection leading to neuropraxia or axonotmesis and function returns within a few days to 3 months. Division of the nerve (neurotmesis) results in permanent loss of function and repair attempts have a very poor track record. Unilateral injury causes various levels of hoarseness. Bilateral nerve injury may lead to the inability to protect the airway and usually the need for a tracheostomy.
What other nerves may be injured during thyroidectomy?
View Answer
The external branch of the superior laryngeal nerve may be damaged during the mobilization of the superior pole of the thyroid. This is the motor nerve of the inferior pharyngeal constrictor and cricothyroid muscles, and injury is manifested by limitation of the force of voice projection and lowering of the pitch. This function usually improves during the first 3 months after thyroidectomy but may persist if the nerve is divided.
What are the signs and symptoms of hypoparathyroidism, and how would you treat it?
View Answer
The parathyroids are very delicate and despite meticulous dissection, clinically significant hypoparathyroidism after thyroid resection is usually a temporary problem. The signs and symptoms of hypoparathyroidism occur within the first few days after surgery. The early symptoms are perioral numbness, tingling of the fingers, and in extreme cases, carpopedal spasm. The threshold of muscular excitability is lowered, and involuntary spasms occur. The following are classic signs of hypo-parathyroidism:
Chvostek’s sign: ipsilateral facial muscles contract when the facial nerve is tapped against the bone just anterior to the ear.
Trousseau’s sign: carpal spasm occurs after the brachial artery is occluded for 3 minutes with an inflated sphygmomanometer cuff.
Spontaneous carpopedal spasm: hands and feet contract spontaneously. This is called tetany.
The calcium level is measured postoperatively in any patient undergoing total thyroidectomy. It is probably unnecessary to perform this study when only one side has been explored. If the patient is symptomatic or if the calcium level falls to less than 7.5 to 8 mg/dL, oral calcium replacements are given (500 mg of elemental calcium in the form of 1250 mg of calcium carbonate (Os-Cal) or 600 mg. of calcium as 1500 mg. of calcium citrate (Caltrate) every 6 hours). Most postoperative hypoparathyroidism resolves over the first few days or weeks. If the hypocalcemia is unresponsive to oral calcium supplementation, oral vitamin D (calcitriol 0.25 to 0.5 µg daily) may be given.
How is postoperative hemorrhage managed?
View Answer
This potentially serious complication is fortunately uncommon. Accumulation of blood or formation of a clot in the closed space around the trachea can lead to airway constriction. The treatment is to open the wound and evacuate the clot at the bedside and obtain hemostasis in the operating room. Tracheostomy is contraindicated if the clot is evacuated. If airway control is needed, the patient can be intubated orally.
After the thyroidectomy, Ms. Arnold’s voice appears to be unchanged from the preoperative period, and she has no complications. She is discharged from the hospital.
What is the prognosis for the different types of thyroid cancers?
View Answer
Several prognostic scoring systems have been developed for well-differentiated thyroid cancer. Two such systems are the AGES system (age of patient; grade, extent, and size of tumor) (11) and the AMES system (age, metastatic disease, and extent and size of tumor) (12). Papillary carcinoma has the most favorable prognosis, with approximately 95% survival at 10 and 20 years. The prognosis for follicular and medullary carcinomas is less favorable, with 80% of patients surviving at 10 years and 71% at 20 years (13). Anaplastic carcinomas have a poor prognosis: fewer than 10% of patients survive 1 year (14).
What is the recommended follow-up for the different types of carcinomas?
View Answer
The follow-up for well-differentiated carcinomas consists of physical examination, thyroglobulin measurements, ultrasonography, chest radiography, and 131I nuclear scanning. For patients with medullary carcinoma, the follow-up is similar, but it also includes calcitonin measurement and molecular analysis of the Ret protooncogene. This is important for family members for evaluation of familial carcinoma.
Ms. Arnold is prescribed L-thyroxine supplements. At the first postoperative clinic visit, her wound appears to be well healed, and she reports feeling well.
Barbara Morin has had a thyroid nodule for a few years and has been referred by her primary care physician. She has been told that the nodule is not cancer.
What are the common causes of thyroid nodules besides carcinoma?
View Answer
Other causes are multinodular goiter or follicular hyperplasia, Hashimoto’s disease (lymphocytic thyroiditis), and follicular adenoma.
What does goiter mean, and what causes it?
View Answer
Goiter is benign enlargement of the thyroid gland. The term is derived from the Latin guttur, which means throat. The pathogenesis of multinodular goiter in most cases is unknown; the involvement of growth factors is being investigated (15). TSH clearly plays a role in iodine deficiency states, but iodine deficiency is rare in the United States today.
What are the clinicopathologic manifestations of goiter, and what is the recommended therapy?
View Answer
The thyroid gland may have nodules of variable size and number or be smooth and diffusely enlarged. Patients with goiter may be asymptomatic, although they more commonly complain of a neck mass or an increase in neck size, sometimes with pressure symptoms. On physical examination there will usually be a palpable mass that moves on swallowing. If the goiter extends retrosternally, the patient’s face becomes suffused with blood when the arms are raised above the head because the goitrous mass obstructs venous return from the head (Pemberton’s sign). Thyrotoxicosis can also develop in patients with a long-standing history of multinodular goiter (toxic multinodular goiter).
A multinodular goiter that produces no symptoms may not require treatment. Indications for surgery are pressure, cosmetic deformity, persistent growth of the goiter, and a nodule suspicious for cancer.
What is Hashimoto’s thyroiditis?
View Answer




Hashimoto’s thyroiditis, or chronic lymphocytic thyroiditis, is the most common form of chronic thyroiditis. It is an autoimmune disease in which antibodies to thyroglobulin are formed. The thyroid may be diffusely enlarged and firm or it may be reduced in size or even difficult to palpate at all. The presence of nodules may cause this condition to be confused with a multinodular goiter or carcinoma. Hashimoto’s thyroiditis is seen predominantly in women, with a mean age of 50 years. Common complaints are neck enlargement and associated pain and tenderness. Most patients are euthyroid or, most commonly, hypothyroid. Occasionally, Hashimoto’s thyroiditis can result in hyperthyroidism.
A high serum titer of thyroid antibodies is diagnostic of this disease. Needle aspiration and cytologic examination may be indicated to rule out carcinoma.
The treatment of Hashimoto’s disease depends on severity. In some patients, no therapy is indicated, whereas other patients require thyroid replacement therapy to relieve hypothyroidism. Surgery is indicated for pressure, for suspected carcinoma, and for cosmetic reasons. After surgery, most patients will need to take replacement doses of thyroid hormone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree