Preoperative Anesthetic Assessment of the Surgical Patient
Thomas McNiff
Cornelius Dyke
Mrs. Barr is a 65-year-old woman whom the anesthesiologist is called to see before surgery. She presented to the emergency department with abdominal pain and bilious emesis of 2 days’ duration. After evaluation by the general surgery service, she is scheduled for an exploratory laparotomy for a presumed small bowel obstruction. Further medical history reveals hypertension, non-insulin-dependent diabetes mellitus, and severe degenerative joint disease, which limits her ability to walk. She has not seen her primary physician for 2 years. She has a 30-pack-year history of smoking.
Mrs. Barr’s surgical history includes an aortofemoral bypass graft 8 years ago and a right femoropopliteal bypass graft 3 years ago. She takes a beta-blocker and a diuretic for hypertension, a nonsteroidal anti-inflammatory for joint pain, and metformin (Glucophage) for diabetes. She has no medical allergies.
Why is an anesthetic assessment needed?
View Answer
An anesthetic assessment includes taking a pertinent history, performing a physical examination, assigning American Society of Anesthesiologists (ASA) physical status (Table 1.1), and performing appropriate laboratory tests. The anesthetic evaluation is designed to ensure proper preparation of the patient for surgery and to allow risk stratification. Multiple studies and closed claim analyses have indicated that inadequate preoperative planning and errors in patient preparation are the most common causes of anesthetic complications. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) standards emphasize the importance of the anesthetic assessment by requiring that in any accredited facility all patients undergoing sedation or regional or general anesthesia have a standardized preoperative assessment.
TABLE 1.1. American Society of Anesthesiologists (ASA) Status | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
What is Mrs. Barr’s NPO status?
View Answer
NPO (nil per os; nothing by mouth) status is used to assess the patient’s likelihood of having a full stomach and thus having increased risk of aspiration. Patients with normal gastric motility require more than 4 hours to empty the stomach of solid matter (1). However, patients with decreased gastric motility are always considered to have full stomachs and to be at increased risk for aspiration. Decreased motility can occur in patients with intestinal obstruction, trauma patients, obese patients, gravid women, and patients with diabetes mellitus.
What is rapid-sequence intubation?
View Answer
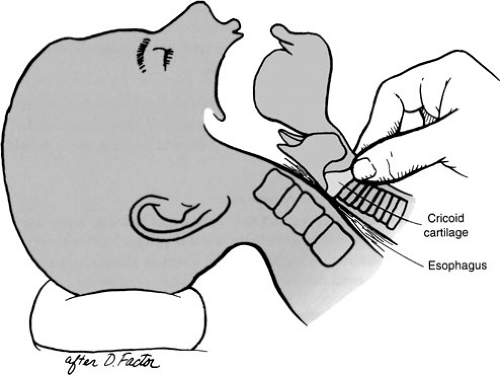
Rapid-sequence intubation is a technique used for patients at risk for aspiration. The patient is preoxygenated with 100% oxygen and an intravenous (IV) anesthetic agent is administered, followed rapidly by IV succinylcholine. Cricoid pressure is applied to occlude the esophagus in the event of passive regurgitation (Fig. 1.1) and is maintained until tracheal intubation is confirmed by measuring end-tidal carbon dioxide, documenting bilateral breath sounds, and noting inflation of the endotracheal tube cuff has occluded the trachea.
Mrs. Barr has been NPO for 2 days. What else does this imply?
View Answer
Any NPO period creates a fluid deficit. Fluid deficits contribute to hemodynamic instability and risk of cardiac and renal complications. Correction of fluid deficit is based on calculation of maintenance fluid and third-space volume requirements.
Maintenance IV fluids are calculated according to body weight for both children and adults. The initial 10 kg of a person’s body weight is allotted at 4 mL per kg; the second 10 kg is allotted at 2 mL per kg; and any remaining weight is allotted at 1 mL per kg.
Calculation of the patient’s fluid deficit is based on maintenance volume and the number of hours he or she has been NPO. Half of this fluid is replaced during the first hour of surgery, and 25% of the volume is replaced during each of the subsequent 2 hours.
Additional intraoperative fluid requirements are calculated according to third-space fluid losses anticipated in the operating room, which are also based on the patient’s weight. Operations without much fluid loss, such as eye surgery, have third-space losses of 2 mL per kg per hour. Operations with moderate fluid losses, such as ventral hernia repair, are replaced at 6 mL per kg per hour. Large operations with much exposed viscera, such as abdominal aorta resection or exploratory laparotomy, have large fluid shifts and patients are given an additional 10 to 15 mL per kg per hour. The overall determinant of adequate fluid resuscitation is urine output, which should be at least 0.5 mL per kg per hour.
Why is a patient’s anesthetic history important?
View Answer
History repeats. If old charts are available, review them to determine ease of laryngoscopy and intubation, type of anesthetic used, and any complications associated with anesthesia. If old charts are not available, ask the patient what types of anesthetics he or she has had (e.g., regional versus general). Seek details of the previous anesthetics: ask the patient whether he or she has ever been told that the anesthesiologist had difficulty placing a breathing tube, and ask whether he or she required prolonged postoperative ventilation.
Why is a family history of problems with anesthetics important?
View Answer
A family history of problems with anesthetics may indicate inherited risks (e.g., malignant hyperthermia). Many patients have not had prior surgery, but the family history might help the anesthesiologist become aware of inherited conditions that may threaten life.
Mrs. Barr states that she had general anesthesia for her aortobifemoral bypass graft and had no problems. However, her sister almost died of an intraoperative “fever.”
What is malignant hyperthermia?
View Answer
Malignant hyperthermia is an autosomal dominant trait that causes severe fevers and massive catabolism. It is triggered by administration of some anesthetic agents. Initially, it manifests as tachycardia and cardiac dysrhythmia, which can result in complete cardiac collapse. Malignant hyperthermia may not manifest until 24 hours after exposure. The physiologic mechanism is believed to be an excessive release of calcium from the sarcoplasmic reticulum in skeletal muscle, which results in severe muscle contractures. Anesthetic agents known to trigger malignant hyperthermia are the volatile anesthetics (e.g., halothane, desflurane, isoflurane), succinylcholine, and decamethonium (2). Total IV anesthesia and regional anesthesia are generally considered safe for these patients. Malignant hyperthermia is associated with other disorders, such as Duchenne’s muscular dystrophy and King-Denborough syndrome (3).
After obtaining a complete history, perform a thorough physical examination, paying particular attention to the airway and cardiovascular, pulmonary, and neurologic systems. Also assess other pertinent organ systems.
Why is an examination of the airway important?
View Answer
Examination of the airway allows the anesthesiologist to assess how easy it will be to intubate the patient and to anticipate any difficulty with the airway. Considerations during examination include the Mallampati classification, extent of mouth opening, hyomental distance, and neck range of motion.
What is the Mallampati classification?
View Answer
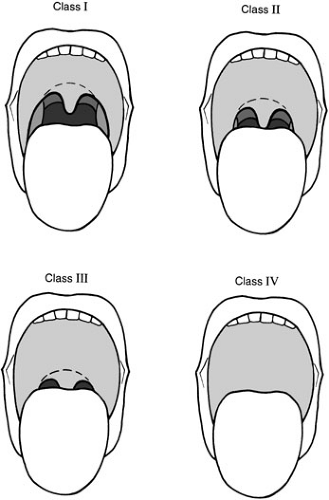
The Mallampati classification system assesses the size of the tongue relative to the oropharyngeal cavity (Fig. 1.2). It is performed with the patient sitting upright and the head in a neutral position. The patient maximally opens his or her mouth and maximally protrudes his or her tongue. The patient should not phonate because this falsely raises the soft palate and gives an erroneous classification. The airway is classified by what structures are visualized:
Class I: the soft palate, fauces, uvula, and anterior and posterior tonsillar pillars
Class II: the soft palate, fauces, and uvula
Class III: the soft palate and base of the uvula
Class IV: the soft palate not visible
There is a correlation between Mallampati class and ease of laryngoscopy. Class I patients are expected to be relatively easy to intubate, whereas class IV patients are expected to be difficult to intubate. This score combined with range of motion of cervical vertebrae and presence or absence of dentition allows relatively accurate prediction as to the difficulty of intubation.
Why does the anesthesiologist want to know the patient’s height and weight?
View Answer
The dosage of most drugs used in the operating room is determined by body weight (milligrams per kilogram). Spinal and epidural anesthesia dosing is based on height. Also, in the event that a pulmonary artery catheter is placed, body surface area (BSA) is used for such calculations as cardiac index and systemic vascular resistance index.
How is BSA calculated?