Obesity Surgery
Mohammad K. Jamal
Eric J. DeMaria
Mrs. Greene is a 43-year-old white woman referred by her primary care physician for evaluation for a bariatric procedure. She has tried several weight loss programs and diet pills without much success.
She has significant comorbidities, including non-insulin-dependant diabetes mellitus, hypertension, degenerative joint disease, and chronic venous insufficiency. She also has sleep apnea for which she uses continuous positive airway pressure at night. She takes several medications including glipizide (Glucotrol), hydrochlorothiazide, and non-steroidal anti-inflammatory drugs (NSAIDs). Her psychiatrist recently diagnosed her with clinical depression and started her on paroxetine HCl (Paxil).
Mrs. Greene’s surgical history is significant for a total abdominal hysterectomy and appendectomy. She has had several right knee arthroscopies for evaluation of a torn meniscus as well as back surgery for a herniated disc.
Mrs. Greene is an obese female in no apparent distress with normal vital signs on examination. She weighs 326 pounds and is 5 feet 4 inches tall, giving her a body mass index (BMI) of 56 kg/m2. Examination of her respiratory and cardiovascular system is unremarkable. Her abdominal examination reveals well-healed scars from prior surgeries as well as a small, easily reducible umbilical hernia. Her rectal examination is normal, and the stool is guaiac negative. Her lower extremities show changes of chronic venous disease. A preliminary diagnosis of morbid obesity-related comorbidities is made on the basis of history and physical examination findings.
What is the genetic basis of obesity?
View Answer
Obesity is a complex disease influenced by the interaction of several genetic, endocrine, metabolic, and environmental factors. One of the major breakthroughs in obesity research was the identification of the mutated ob gene in mice. The protein encoded by this gene is leptin, which is a glycoprotein secreted primarily from adipose tissue that is thought to be a primary regulator of metabolism. Leptin functions in several ways. It acts as a satiety signaler by suppressing neuropeptide Y expression from the hypothalamus, impairs insulin-mediated glucose uptake in skeletal muscle, stimulates lipogenic enzymes in adipocytes, and alters hypothalamic-pituitary-adrenal balance, all of which contribute to obesity.
Although leptin trials in humans have been disappointing, the findings described have generated tremendous interest in the link between genetic factors and obesity. Elevated leptin blood levels in humans are associated with an increased percentage of body fat, a higher BMI, insulin resistance characterized by high blood pressure, low levels of high-density lipoprotein cholesterol, and elevated fasting insulin levels. Elevated leptin levels may be directly related to increased risk of heart disease.
The human obesity gene and the leptin receptor genes have been cloned, and several members of families with a mutation in the coding sequence of the leptin receptor gene have been identified. Other genetic mutations that may play some role in the development of obesity in humans include those of the glucocorticoid receptor gene responsible for glucocorticoid promotion of visceral fat accumulation, the beta-adrenergic receptor responsible for catecholamine effect on energy metabolism, and the sulfonylurea receptor gene responsible for glucose-stimulated insulin secretion.
How is obesity defined according to the National Institutes of Health (NIH) Consensus Panel on Gastric Surgery for Severe Obesity?
View Answer
The most accurate way to define the relationship between body weight and frame size is to use the BMI, which is calculated by dividing the patient’s weight in kilograms by the patient’s height in meters squared. Obesity is defined as a BMI of greater than 30 kg per m2. The 1991 NIH Consensus Panel on Gastric Surgery for Severe Obesity defined morbid obesity as a BMI of 35 kg per m2 or greater with severe obesity-related comorbidities or as a BMI of 40 kg per m2 or greater without comorbidities. Super-obese patients are defined as having a BMI of 50 kg per m2 or greater. Other definitions of morbid obesity include patients who weigh at least 200% of their ideal body weight (IBW).
What is the prevalence of morbid obesity in the United States?
View Answer
Obesity is a serious health problem in the United States; nearly 20% of the adult population is obese. An estimated 32.6 million Americans are overweight and 11.5 million are morbidly obese.
What are some of the obesity-related comorbidities and their impact on health care?
View Answer
Significant obesity-related illnesses include adult-onset diabetes mellitus, hypertension, hypercholesterolemia, obesity hypoventilation and sleep apnea syndrome, cholelithiasis, cardiovascular disease, renal disease, and osteoarthritis. Others include necrotizing panniculitis, hypercoagulable states, and psychosocial problems as well as an increased risk of uterine, colon, and breast cancer. Several obesity-related illnesses may cause significant physical and emotional disability, including overflow incontinence, pseudotumor cerebri, sex-hormone imbalance, and gastroesophageal reflux. Overall, obesity-related illnesses consume nearly 5% of the total health care costs in the United States, a staggering $100 billion.
Does dietary treatment have a long-term success rate in the treatment of obesity?
View Answer
No dietary approach has achieved long-term success in the treatment of morbid obesity. Two diet pills (phentermine and phenformin) were associated with an unacceptably high incidence of cardiac valvular disease and pulmonary hypertension and were removed from the market by the Food and Drug Administration (FDA). Currently available sibutramine (Meridia) and orlistat (Xenical) are associated with only a 10% weight loss in most studies. Surgery has been the only method proven to maintain long-term weight loss, and current options include restrictive procedures, malabsorptive procedures, or a combination of both.
What are the current surgical options, their associated complications, and the outcome data for the treatment of morbid obesity?
View Answer
Surgical options for the treatment of morbid obesity can be divided into a combination of both restrictive and malabsorptive procedures or purely restrictive procedures. An example of the former is the Roux-en-Y gastric bypass, whereas vertical band gastroplasty, horizontal gastroplasty, and gastric banding are purely restrictive gastric procedures.
Roux-en-Y Gastric Bypass
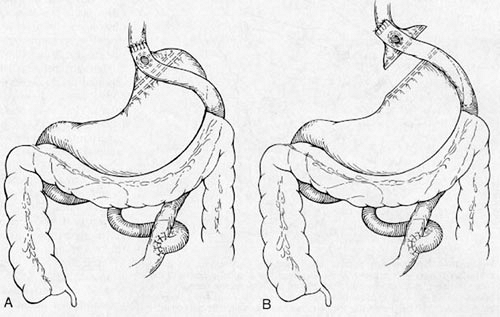
This is currently the gold standard procedure. It developed based on the observation that patients who underwent partial gastrectomy for peptic ulcer disease tended to remain underweight. The proximal gastric bypass procedure uses a 30-mL pouch, a gastroenterostomy stoma of 1 cm, and a 45-cm long Roux-en-Y limb. The long-limb gastric bypass procedure for super-obese patients (BMI ≥50) involves a 150-cm long Roux limb (Fig. 9.1).
The gastric bypass works both by restricting the amount of food eaten and by intentionally inducing a dumping syndrome that pertains to high-fat, high-carbohydrate liquids. This procedure has been highly successful with several large series of patients over a long period who have demonstrated superior excess weight loss (EWL) when compared with patients who underwent gastric restrictive procedures. Long-lasting weight loss is typically 66% EWL at 2 years, 60% EWL at 5 years, and 50% EWL at 10 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree