Location
Morphology
Number of quadrants involved
Degree of fixation
Mobility
Extrarectal growths
Direct continuity with other structures (vagina)
DRE alone is considered inadequate in the staging of rectal cancer.
Rectal Ultrasound
Endorectal ultrasound (EUS) is an outpatient procedure requiring only enema preparation and often no sedation.
The accuracy of ERUS is user dependent and variable (Fig. 42.1).
The Minnesota series, one of the largest series published in 2002 by Garcia-Aguilar et al., describes 1,184 patients with rectal carcinoma or villous adenoma that underwent ERUS. Histopathologic correlation was available for the 545 patients who had no prior radiotherapy.
The accuracy of ERUS in assessing the level of penetration was only 69 %, with 18 % overstaged and 13 % understaged.
For nodal involvement, the accuracy in the 238 patients who had radical surgery was poor, 64 % with 25 % overstaged and 11 % understaged.
Limitations to ERUS:
A significant learning curve associated with the interpretation of the endorectal ultrasound image.
Rafalesen et al. reported that the reader experience had a significant effect on the assessment of penetration of the bowel wall by tumor. When comparing more experienced with less experienced radiologists, the accuracy for bowel wall penetration was 90 % vs. 66 %, respectively.
Overstaging of a tumor is common because of the inability of ultrasound to differentiate perirectal inflammation from tumor infiltration in the perirectal fat.
ERUS is difficult to perform in near obstructing lesions and those higher up in the rectum.
Magnetic Resonance Imaging
MRI use in staging rectal cancer was originally described in 1986.
Fig. 42.1
The main concept in the use of MRI to stage rectal cancer is to obtain high-resolution images within small field-of-view thin sections with fast/turbo spin echo (FSE/TSE) T2-weighted axial and coronal views of the rectum. (a) EUS demonstrating the five layers of the rectum, (b) Standard EUS of a rectal tumor
Kim et al. compared the histopathologic staging with the preoperative staging in 217 rectal cancer patients. The accuracy for the depth of invasion was 81 % and for regional lymph node metastasis was 63 %.
MRI T staging has been defined (Table 42.2).
Table 42.2
MRI T staging as proposed by Brown et al.
MRI T stage
T1: Low signal in the submucosal layer or replacement of the submucosal layer by abnormal signal not extending into circular muscle layer
T2: Intermediate signal intensity within muscularis propria. Outer muscle coat replaced by tumor of intermediate signal intensity that does not extend beyond the outer rectal muscle into perirectal fat
T3: Broad-based bulge or nodular projection (not fine speculation) of intermediate signal intensity projecting beyond outer muscle coat
T4: Extension of abnormal signal into adjacent organ, extension of tumor signal through the peritoneal reflection
MRI identification of metastatic lymph node involvement has not been standardized.
Criteria that are most predictable for determining lymph node metastasis are signal heterogeneity and an irregular border. Size criteria are not adequate. It is important to remember that in patients with rectal cancer, approximately 15 % of lymph nodes smaller than 5 mm are positive for metastasis.
With the use of ultrasmall superparamagnetic iron oxide (USPIO)-enhanced MRI, recent advances have been made in the evaluation of lymph nodes. The iron oxide nanoparticle is given intravenously and is transported to the lymphatic system where it is picked by macrophages. The nanoparticle causes a decrease in signal intensity, and therefore, inflammatory lymph nodes exhibit less signal intensity.
Initial results using this technique demonstrate up to 93 % sensitivity and 96 % specificity for perirectal lymph node metastasis. However, larger prospective trials are needed.
In recent years, tumor involvement of the circumferential resection margin (CRM) has been identified as an important predictor of locoregional recurrence in rectal cancer patients undergoing a radical proctectomy with total mesorectal excision (TME).
The preoperative assessment of the relationship of the tumor with the fascia propria of the rectum, the CRM in patients treated with TME, has become of upmost importance in selecting neoadjuvant therapy and planning the surgical resection.
The fascia propria of the rectum is well visualized by phased-array coil MRI, and several studies have suggested that MRI can predict with high degree of accuracy the distance of the tumor to the fascia propria of the rectum (Fig. 42.2).
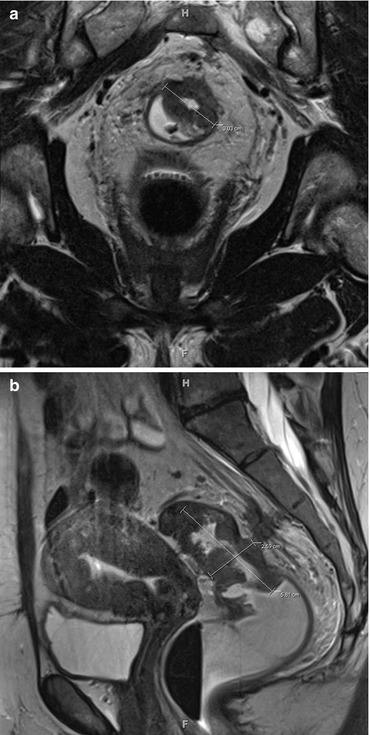
Fig. 42.2
(a and b). The main concept in the use of MRI to stage rectal cancer is to obtain high-resolution images within small field-of-view thin sections with fast/turbo spin echo (FSE/TSE) T-2-weighted axial and coronal views of the rectum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






