Fig. 50.1
Transanal procedure. (a) Exposure and placing traction sutures. (b) Start full thickness rectal dissection above pectinate line. (c) Pulling rectosigmoid down
Full-thickness biopsies are taken to determine the place where the normoganglionic portion of the colon is reached.
A primary procedure, without a protective colostomy, requires the presence of an experienced clinical pathologist, familiar with the interpretation of frozen sections, to identify the normoganglionic portion of the colon.
In the absence of an experienced pathologist, the surgeon must create a colostomy proximal to the transition zone, in the right transverse colon or with an ileostomy.
A Swenson operation consists of a resection of the aganglionic segment (transabdominal or transanal), including a part of the normoganglionic dilated colon, and pull-through of a normoganglionic bowel, with a coloanal anastomosis of the normoganglionic bowel to the rectum, above the pectinate line.
A Duhamel operation preserves the aganglionic rectum, dividing the colon at the peritoneal reflection. The normoganglionic colon is then pulled through a presacral space, created by blunt dissection and anastomosed to the rectal wall above the pectinate line.
A Soave procedure consists of an endorectal (submucosal) dissection of the aganglionic colon down to the pectinate line, leaving a seromuscular cuff. The normally innervated colon is passed through the muscular cuff and anastomosed to the rectum.
A transanal approach can be performed provided the transition zone is in the sigmoid. If not, laparoscopy can be added for splenic flexure mobilization.
Complications
An algorithm to the approach to post-pull-through Hirschsprung’s patients with problems is shown in Fig. 50.2.
Fig. 50.2
Algorithm for post-pull-through Hirschsprung’s disease patient who is not doing well
To avoid incontinence, preservation of the dentate line and not overstretching the sphincters are crucial.
Enterocolitis is a complication without a known etiology, unless there is an anatomic explanation, such as a stricture causing stasis, but is felt to be due to fecal stasis.
Postoperative constipation can be avoided by resecting not only the aganglionic segment but also the dilated portion of the colon.
Swenson operation may be associated with higher rates of nerve damage that may provoke urinary and sexual disturbances.
The Duhamel procedure is commonly followed by severe problems of constipation and dilatation of the aganglionic piece of colon left in place.
In the Soave operation, patients may suffer from fecal incontinence, as well as perianal fistulas and abscesses due to the presence of islets of mucosa left behind during the endorectal dissection.
Surgical Management of Total Colonic Aganglionosis
An ileostomy is performed in a newborn and then at age 1–3 years resection of the entire aganglionic colon and pull-through of the normal ganglionic terminal ileum that is anastomosed just above the anal canal.
They suffer from multiple stools and treatment is with loperamide, pectin, and a constipating diet.
Ultrashort-Segment Hirschsprung’s
Both the existence and treatment of the ultrashort-segment aganglionosis are controversial as normal individuals have variable length of aganglionosis above the pectinate line.
Typically, Hirschsprung’s in adults is of the short-segment variety.
Many actually have idiopathic constipation that responds to laxative therapy.
Some surgeons propose a myectomy, consisting of a resection of a strip of smooth muscle from the anal verge up to the area where ganglion cells are found.
Neuronal Intestinal Dysplasia (NID)
Neuronal intestinal dysplasia refers to a histological condition that includes hypertrophy of ganglion cells, immature ganglia, hypoganglionosis, hyperplasia of the submucosal and myenteric plexus, and giant ganglion cells as well as hypoplasia or aplasia of the sympathetic innervations of the myenteric plexus.
Most cases of NID are likely sampled areas of colon that are actually transition zone bowel in a Hirschsprung’s patient.
Anorectal Malformations (Imperforate Anus)
Anorectal malformations represent a spectrum of defects characterized by the absence of an external anal orifice, occurring in about 1 in every 5,000 newborns.
The majority have an abnormal communication between the rectum and the perineum (perineal fistula), the vestibule (vestibular fistula), or the vagina (vaginal fistula), in the female.
In some female patients, the rectum, vagina, and urethra are fused together forming a common channel (cloacal malformation) and open into a single external orifice.
In the male, the communication is with the urethra (rectourethral fistula) or the bladder (rectobladder neck fistula).
The most common type of defects seen in boys is a rectourethral fistula and the most common type in girls is vestibular fistula (Table 50.1).
Table 50.1
Current classification of anorectal malformations
Male
Perineal fistula
Rectourethral fistula
Bulbar
Prostatic
Rectobladder neck fistula
Imperforate anus without fistula
Rectal atresia and stenosis
Female
Perineal fistula
Vestibular fistula
Imperforate anus without fistula
Rectal atresia and stenosis
Cloaca
Complex malformations
Associated Anomalies
Urogenital abnormalities occur in about 50 % of all patients with anorectal malformations.
Unilateral renal agenesis is the most common urologic anomaly, followed by vesicoureteral reflux.
Other important abnormalities include cryptorchidism, hypospadias, renal ectopia, and hydronephrosis.
Sacral and spinal abnormalities are also very common (agenesis, hypoplasia, hemivertebrae, scoliosis).
A tethered cord occurs in 25 % of patients, where the spine grows faster than the cord, producing traction on the nerve fibers that may produce functional disturbances in the motion of the lower extremities and may contribute to sphincter problems particularly impacting bladder emptying.
An anorectal malformation with hemisacrum and a presacral mass (dermoid, teratoma, lipoma, anterior meningocele) is known as the Currarino triad.
Approximately 8 % have esophageal atresia.
Approximately 30 % have an associated cardiovascular anomaly (PDA, ASD, VSD, tetralogy of Fallot).
The higher the malformation, the worse the functional prognosis will be.
The higher the anorectal defect, the higher the rate of fecal incontinence and the lower the rate of constipation.
The lower the malformation, the higher the incidence of constipation, but the lower the incidence of fecal incontinence.
Specific Defects
Males
Perineal Fistula
The rectum opens anterior to the center of the sphincter mechanism in the perineum.
The end of the rectum often lies immediately below a very thin layer of epithelium with an external opening located at the base of the scrotum or sometimes at the base of the penis.
The overwhelming majority of these patients have a normal sacrum; less than 10 % of them have associated defects.
Treatment consists of moving the anal orifice back to the center of the sphincter, creating a normal-sized anus.
Rectourethral Fistula
In this group of malformations, the rectum connects to the urethra, most commonly into the lower part of the posterior urethra known as the bulbar urethra, (rectourethral bulbar fistula; Fig. 50.3a). Most (~85 %) achieved bowel control after treatment and 30 % have associated defects.
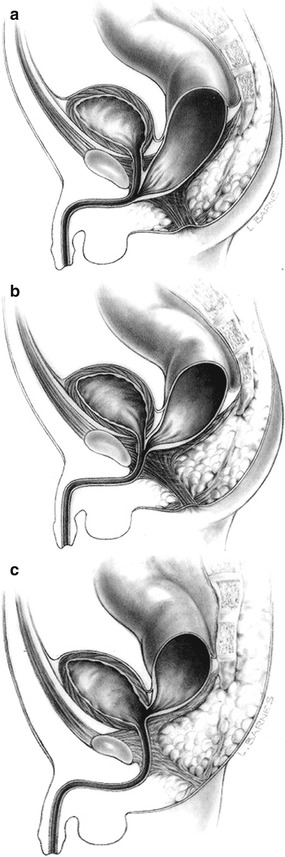
Fig. 50.3
(a) Bulbar fistula (b) Prostatic fistula (c) Bladder neck fistula (Reprinted from Pena, A (1989) Atlas of surgical management of anorectal malformations with permission from Springer)
In the second subtype, the rectum opens into the upper part of the posterior urethra (rectoprostatic fistula; Fig. 50.3b). Only 60 % of these patients achieve bowel control later in life, and 60 % have significant associated defects.
Most of these patients (rectourethral fistula) require a colostomy at birth, and subsequently (usually 1–2 months later) they receive the definitive repair of the malformation.
The higher the malformation, the more likely the patient will have a flat bottom, meaning that the natural midline groove is absent and there is no distinguishable anal dimple. The lower the malformation, the more prominent the midline groove and the anal dimple.
Rectobladder Neck Fistula
This is the highest of all defects in male patients (Fig. 50.3c), where the rectum is connected to the bladder neck.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






