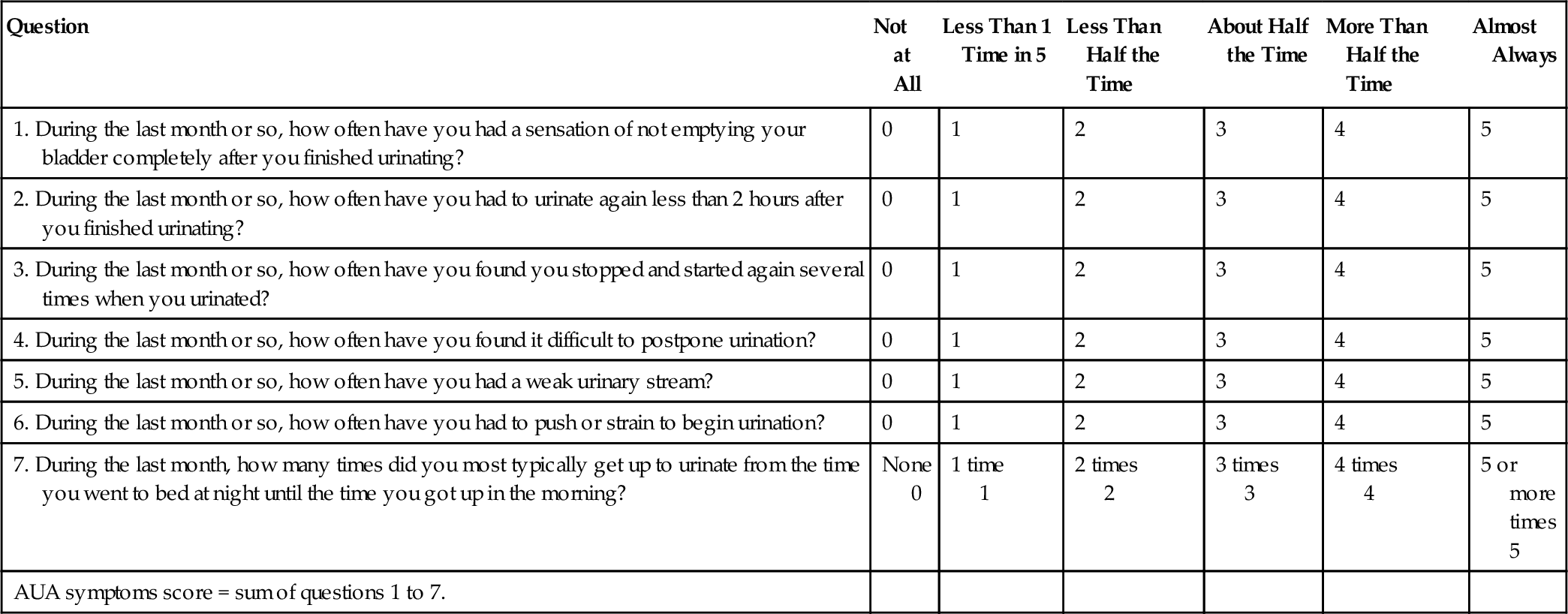
Chapter 1 Urology is a surgical specialty devoted to the study and treatment of disorders of the genitourinary tract of the male and the urinary tract of the female. The urologist surgically corrects acquired and congenital abnormalities and diagnoses and treats many medical disorders of the genitourinary tract. 2. There is a wide overlap with other specialties, and urologists have frequent interaction with other physicians, including family practitioners, internists, pediatricians, geriatricians, endocrinologists, nephrologists, neurologists, obstetricians and gynecologists, and general, vascular, and trauma surgeons. 3. It is important that all physicians be aware of the specific diagnostic and therapeutic measures that are available within this specialty. The most obvious manifestations of urologic disease are those signs and symptoms that are directly related to the urinary tract of the male and female or to the genitalia of the male. Hematuria and scrotal swelling are examples in this category. a. A stone in the kidney or upper ureter may produce ipsilateral testicular pain. b. This same stone may be associated with symptoms of nausea and vomiting. c. The gastrointestinal (GI) tract is probably the most common site to manifest symptoms from primary urologic problems. This is most probably due to the common innervation of these systems and the close direct relationship between the various component organs. 2. Primary urologic disorders may also be manifest in different organ systems and by seemingly unrelated signs and symptoms. Bone pain and pathologic fractures secondary to metastatic carcinoma arising in the genitourinary tract are examples. 3. Similarly, primary disease in other organ systems may result in secondary urologic signs and symptoms that initially lead the patient to the urologist. Diabetes may be detected by finding glucosuria in a patient presenting with frequency and nocturia. Other signs and symptoms mimicking urologic disease are related to inflammatory or neoplastic processes arising in the: b. GI tract c. Female internal genitalia Fever, weight loss, and malaise can be nonspecific systemic manifestations of acute and chronic inflammatory disorders, renal failure, and genitourinary carcinoma with or without metastases. Localized or extensive disease may exist within the genitourinary tract without any signs or symptoms being manifest. 2. Sixty percent of prostate cancers are detected secondary to prostate-specific antigen (PSA) elevations only without palpable abnormalities of the prostate. 3. Far-advanced renal deterioration may occur prior to the detection of silent reflux or obstruction. b. The character, onset, duration, and progression of the symptom are carefully defined. It is important to note what factors exacerbate or ameliorate the problem. 2. Urologic symptoms are generally related to: b. Alterations of micturition c. Changes in the gross appearance of the urine d. Abnormal appearance and/or function of the external genitalia 2. Renal pain b. The etiology of renal pain may be due either to capsular distention or inflammation or to distention of the renal collecting system. c. Renal pain can be a dull, aching sensation felt primarily in the area of the costovertebral angle or pain of a sharp, colicky nature felt in the area of the flank, with radiation around the abdomen into the groin and ipsilateral testicle or labium. The latter is due to the common innervation. d. The nature of the primary disease process within the kidney often determines the type of sensation that is experienced and depends on the degree and rapidity of capsular and/or collecting system distention. 3. Ureteral pain b. The lower ureter, however, sends sensory fibers to the cord through ganglia subserving the major pelvic organs. Therefore pain derived from the lower ureter is generally felt in the suprapubic area, bladder, penis, or urethra. c. The most common etiologic mechanism for ureteral pain is sudden obstruction and ureteral distention. d. Acute renal and ureteral colic are among the most severe types of pain known to humankind. 4. Bladder pain b. The pain of overdistention is generally felt within the suprapubic area, resulting in severe local discomfort. c. The pain due to bladder inflammation is generally felt as a sharp, burning pain that is often referred to the tip of the penile urethra in males and the entire urethra in females. 5. Prostate pain a. Sensory fibers from the prostate mostly enter the sacral aspect of the spinal cord. b. Prostate pain is most commonly due to acute inflammation and is generally perceived as discomfort in the lower back, rectum, and perineum. c. Irritative symptoms arising from the bladder may overshadow the purely prostate symptoms. 6. Penile pain a. Penile and urethral pain are generally directly related to a site of inflammation. 7. Scrotal pain a. Pain within the scrotum generally arises from disorders of the testis and/or epididymis. b. The most common etiologic factors include trauma, torsion of the spermatic cord, torsion of the appendix testis or appendix epididymis, and acute inflammation, particularly epididymitis. The pain in these cases is generally of rapid onset, if not sudden, and severe in nature. c. Hydroceles, varicoceles, and testicular tumors can also be associated with scrotal discomfort but are generally of a more insidious nature and less severe in most cases. b. It must be emphasized that a variety of disease processes can result in similar symptoms at the level of the lower urinary tract, and although these terms are used to describe specific symptoms in this area, they do not necessarily pertain to specific etiologies. 2. Changes in urine volume b. Polyuria refers to an increase in the volume of urine excreted on a daily basis. The etiologic mechanisms include increased fluid intake, exogenous or endogenous diuretics, and abnormal states of central or peripheral osmoregulation. 3. Irritative symptoms b. Strangury is a subtype of dysuria in which intense discomfort accompanies frequent voiding of small amounts of urine. c. Frequency refers to the increased number of times one feels the need to urinate. This can be secondary to a true decrease in bladder capacity from a loss of elasticity or edema due to inflammation, or it can be secondary to a decrease in the effective bladder capacity due to a failure of the bladder to empty completely with persistence of a large amount of residual urine. d. Nocturia is essentially the nighttime equivalent of urinary frequency, that is, a decreased real or effective bladder capacity forces the patient to arise at night to urinate. e. Nycturia refers to the excretion of larger volumes of urine at night than during the day and is secondary to mobilization of dependent fluid that accumulated when the patient was in the upright position. Nycturia can result in nocturia even in the presence of a normal bladder capacity if large quantities of fluid are mobilized. f. Urgency refers to the sudden, severe urge to void that may or may not be controllable. g. The irritative symptoms noted previously are most commonly associated with inflammation of the lower urinary tract, that is, bladder and prostate. Acute bacterial infections probably represent the most common etiologic mechanism. It should be noted, however, that the irritative symptoms may be secondary to the presence of a foreign body, nonspecific inflammation, radiation therapy or chemotherapy, neoplasms, and neurogenic bladder dysfunction. h. The term overactive bladder refers to the symptoms of frequency and urgency, with or without urge or reflex incontinence, in the absence of local pathologic or metabolic factors that would account for these symptoms. The urodynamic-based definition of overactive bladder requires the demonstration of involuntary bladder contractions. 4. Bladder outlet obstructive symptoms a. Hesitancy refers to the prolonged interval necessary to voluntarily initiate the urinary stream. b. Straining refers to the need to increase intraabdominal pressure to initiate voiding. c. Decreased force and caliber of the urinary stream refer to the physical changes of the urinary stream that may be noted due to increased urethral resistance. d. Terminal dribbling refers to the prolonged dribbling of urine from the meatus after the completion of micturition. e. Sense of residual urine is the complaint of a sensation of incomplete emptying of the bladder that the patient recognizes after micturition. f. Prostatism. All of the previous symptoms may be noted with any type of bladder outlet obstruction, that is, secondary to benign prostatic hypertrophy (BPH), prostate carcinoma, or urethral stricture disease. The most common cause of these symptoms, however, is benign prostatic enlargement, and hence this complex of symptoms has often been referred to as prostatism. g. Urinary retention. Acute urinary retention may be associated with severe suprapubic discomfort. Alternatively, the chronic retention of urine within the bladder may occur on a gradual basis due to progressive obstruction and bladder decompensation, and large amounts of urine may be retained with minor changes in symptomatology. h. Interruption of the urinary stream. Sudden painful interruption of the urinary stream can be secondary to the presence of a bladder calculus that ball valves into the bladder neck, causing abrupt blockage of the urinary flow. i. Bifurcation of the urinary stream. The symptom of a double stream or spraying of the urinary stream can be secondary to urethral stricture disease or can occur intermittently without any obvious pathology. 5. Incontinence b. False or overflow incontinence is seen with total bladder decompensation in which the bladder acts as a fixed reservoir and the only outflow of urine is an overflow phenomenon with constant dribbling through the bladder outlet. c. Urgency incontinence results when the sensation of urgency becomes so severe that involuntary bladder emptying occurs. This is commonly secondary to severe inflammation of the urinary bladder. This type of incontinence can also be due to involuntary bladder contractions without inflammation (see definition of overactive bladder on Page 6). d. Stress incontinence is secondary to distortion of the normal anatomic relationship between the bladder and the urethra such that sudden increases in intraabdominal pressure (laughing, straining) are transmitted unequally to the bladder and the urethra, resulting in elevated bladder pressure without a concomitant rise in urethral pressure. Most commonly, this is related to laxity of the pelvic floor, particularly following childbirth, but it may also be noted in women who have not had children. It is also a frequent sequel of radical prostatectomy surgery for prostate cancer. e. It is important to differentiate the various types of incontinence because each is treated differently. Historical factors are very important in separating these different entities. 6. Enuresis refers to involuntary urination and bed-wetting that occurs during sleep. 7. Quantification of voiding symptoms a. The AUA Symptom Index (internationally known as the IPSS) is a self-administered questionnaire consisting of seven questions relating to symptoms of lower urinary tract voiding dysfunction (Table 1-1). The IPSS includes a quality-of-life question to assess the degree of bother experienced by the patient. b. Symptoms are classified as mild (0-7), moderate (8-19), or severe (20-35). c. The symptom score is an integral part of the clinical practice guidelines for treatment planning and follow-up for BPH management. d. The symptom score is not specific for or diagnostic of BPH. It can be used in men and women for general assessment of voiding symptoms. b. Pyuria refers to the finding of large quantities of white blood cells that cause urine to have a cloudy appearance. Microscopic examination of the urine sample will demonstrate the inflammatory nature that is usually secondary to an infection. c. Chyluria refers to the presence of lymph fluid mixed with the urine. It is an unusual cause of cloudy urine. 2. Pneumaturia refers to the passage of gas along with urine while voiding. There may be associated pyuria or frank fecal contamination of the urine, as this phenomenon is almost exclusively due to the presence of a fistula between the GI and urinary tracts. On occasion, the presence of a gas-forming infection within the urinary tract can produce similar symptoms, although this is very unusual. 3. Hematuria a. The passage of bloody urine is always alarming, and generally the patient makes a prompt visit to the physician. Investigation is always warranted, including a properly performed urinalysis to be certain that the red discoloration of the urine is indeed secondary to the presence of blood. For a differential diagnosis of the causes of red urine, see Page 12. b. Although hematuria is always a danger signal, a clue to its significance may lie in whether there is associated pain or whether the bleeding is essentially painless. Pain that occurs in association with cystitis or passage of a urinary tract calculus may indicate that the bleeding is in fact benign in nature. Painless hematuria, however, is always believed to be secondary to a urinary tract neoplasm until proven otherwise. This differentiation is not infallible, and therefore all urinary tract bleeding warrants investigation to be certain that there is not an associated neoplasm in addition to the more obvious cause for painful bleeding. c. The probable site of bleeding within the urinary tract may be ascertained by determining whether the bleeding is initial (at the beginning of the stream only), terminal (at the end of the stream only), or total (throughout the entire stream). Initial hematuria generally indicates some type of anterior urethral bleeding that is flushed out by the initial passage of the bladder urine through the urethra. Terminal hematuria is often secondary to posterior urethral, bladder neck, or trigone bleeding and is noted when the bladder finally compresses these areas at the end of micturition. Total hematuria indicates that the bleeding occurs at the level of the bladder or above, such that all of the urine is mixed with blood and is therefore bloody throughout the entire stream. 4. Colored urine may result from a variety of foods, medications, and medical disorders. The colors may range from almost clear to black, with all other colors of the spectrum noted in between. (See Table 1-2 for common causes of colorful urine.) Table 1-2 Common Causes of Colorful Urine
Signs and Symptoms
The Initial Examination
Background
Definition
Importance to other branches of medicine
Urologic manifestations of disease
Direct
Referred manifestations
Systemic
Asymptomatic
History
Symptoms
Pain
Alterations of micturition
Changes in the gross appearance of the urine
Colorless
Very dilute urine
Overhydration
Cloudy/milky
Phosphaturia
Pyuria
Chyluria
Red
Hematuria
Hemoglobin/myoglobinuria
Anthocyanin in beets and blackberries
Chronic lead and mercury poisoning
Phenolphthalein (in bowel evacuants)
Phenothiazines (Compazine, etc.)
Rifampin
Orange
Dehydration
Phenazopyridine (Pyridium)
Sulfasalazine (Azulfidine)
Yellow
Normal
Phenacetin
Riboflavin
Green-blue
Biliverdin
Indicanuria (tryptophan indole metabolites)
Amitriptyline (Elavil)
Indigo carmine
Methylene blue
Phenols (IV cimetidine [Tagamet], IV promethazine [Phenergan], etc.)
Resorcinol
Triamterene (Dyrenium)
Brown
Urobilinogen
Porphyria
Aloe, fava beans, and rhubarb
Chloroquine and primaquine
Furazolidone (Furoxone)
Metronidazole (Flagyl)
Nitrofurantoin (Furadantin)
Brown-black
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access