Niraj J. Gusani
DEFINITION
■ A segmental hepatectomy consists of surgical resection of one or more functional anatomic segments of the liver, as originally classified by Couinaud (FIG 1). Nomenclature for liver resections was standardized in the Brisbane conference.1
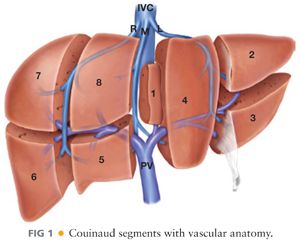
■ The most common anatomic segmental resections are (1) right posterior sectionectomy (segments 6 and 7), (2) left lateral sectionectomy (segments 2 and 3), and (3) caudate lobe resection (segment 1).
■ Smaller resections of a single segment or nonanatomic subsegmental resections will not be covered in this chapter. Usually, these involve simple excisions without formal inflow or outflow occlusion or delineation of the segmental vascular or biliary anatomy.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ Patients should be good medical candidates for major surgery.
■ Preoperative planning requires a thorough history of previous abdominal surgeries.
■ If performing a metastasectomy, there should be a thorough evaluation of extrahepatic disease. The presence of extrahepatic disease should be considered in conjunction with the tumor type and extent of resection to determine if the patient will benefit from surgical intervention involving the liver or extrahepatic sites.
■ Episodes of jaundice, hepatitis exposure, alcohol, illicit drug abuse, and treatment with chemotherapy should be elicited to ascertain the health of the liver parenchyma.
■ A complete viral hepatitis panel should be obtained as part of screening surgical candidates.
■ Liver function can be assessed by the Child-Pugh classification and/or the Model for End-Stage Liver Disease (MELD). Neither metric has been definitively shown to be superior in determining a patient’s ability to tolerate surgery.2
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Multiphase, contrast-enhanced cross-sectional imaging with either computed tomography (CT) or magnetic resonance imaging (MRI) is necessary for planning surgery. Both imaging modalities are of similar sensitivity and may often be used interchangeably or in combination to better define certain pathologic processes.
■ In a normal, healthy liver, a future (postresection) hepatic remnant composed of at least two contiguous segments with adequate inflow and outflow and measuring 25% of the complete liver volume is sufficient functional liver to allow for full hepatic recovery. However, in a damaged or cirrhotic liver, a remnant of greater than 40% is often recommended, although the percentage of viable remnant liver may need to be greater, depending on the amount of damage/dysfunction of the liver. Segmental hepatic resections rarely induce hepatic insufficiency unless the remnant liver is severely diseased.
■ Concern for significant hepatic dysfunction should be investigated by objective testing of the liver. Transjugular measurement of the portal pressure gradient (normal <5 to 8 mmHg), routine serum liver function tests, and biopsy (to evaluate steatosis or cirrhosis) are the most common modalities to evaluate the extent of hepatic disease.
■ In Asia, indocyanine green clearance testing is often performed to quantify liver health. This is rarely performed in the United States.
■ In patients with evidence of decompensated cirrhosis (Child’s B and C) and pathologic conditions that have demonstrated benefit from transplantation (hepatocellular cancer, neuroendocrine malignancies, and some hilar cholangiocarcinomas), surgeons should consider a referral for transplantation.
SURGICAL MANAGEMENT
■ The indications for hepatectomy include diagnostic uncertainty, symptomatic benign lesions, and malignancy (Table 1).
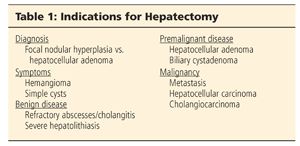
■ The strongest evidence for hepatic metastasectomy shows that R0 resection prolongs survival and is potentially curative for colorectal carcinomas and neuroendocrine tumors.
Preoperative Planning
■ Ideally, preoperative cross-sectional imaging should be discussed with skilled radiologists before surgery and be available throughout the procedure.
■ Vascular, particularly hilar, arterial anomalies are common. Inadvertent injury at surgery may be prevented by thorough multiplanar analysis of preoperative imaging.
■ 3-D reconstruction is not mandatory, but understanding of all the lesions and their relation to hepatic and portal venous structures is imperative. This should be combined with intraoperative ultrasound.
■ For postoperative pain control, we employ epidural catheters, administered by a dedicated pain service, placed preoperatively.
■ Low central venous pressure (CVP) anesthesia is a cornerstone in reducing blood loss in hepatic surgeries. To maintain low CVP (5 to 8 mmHg), good communication with the preoperative nursing and anesthesia teams is critical.
■ Patients receive appropriate prophylactic antibiotics due to transection of the biliary tree (clean-contaminated surgery). We consider cases with an indwelling biliary device as contaminated procedures secondary to colonization of the biliary tract.
■ Most patients undergoing hepatectomy are at high risk for venous thromboembolic (VTE) disease due to age, presence of malignancy, and complex and long major abdominal surgery. Unfractionated heparin is given subcutaneously prior to induction and redosed every 8 hours as needed. Patients undergoing hepatectomy for malignant diagnoses are usually sent home on a 30-day course of low-molecular-weight heparin for VTE prophylaxis.
Positioning
■ Supine with arms abducted. Laparoscopic resections may be facilitated by use of the modified lithotomy position or of a split-leg table. For extreme lateral right liver lesions, full lateral positioning may be used.
TECHNIQUES
RIGHT POSTERIOR SECTIONECTOMY (SEGMENTS 6 AND 7)
Exposure
■ A subcostal, chevron, or midline incision can be used. It is our preference to operate through a midline incision.
■ A fixed traction system is employed. Retraction of the costal margin is critical.
Mobilization
■ The round ligament is ligated but kept long to allow its use for countertraction and exposure. The falciform ligament is divided close to the liver, thus minimizing interference from this structure during intraoperative ultrasonography (IOUS).
■ Dissection of the apex of the right triangular ligament proceeds from medial to lateral. The peritoneum and areolar tissue surrounding the anterior and lateral aspects of the right hepatic vein (RHV) is cleared. To continue laterally and inferiorly, the liver can be retracted medially and compressed posteriorly.
■ If caval compression induces hypotension, temporary release of retraction may be all that is required. Alternatively, raising the inferolateral edge of the right liver will expose the final attachments of the right triangular ligament.
■ Complete mobilization of the right liver requires extensive exposure of the lateral and anterior surface of the inferior vena cava (IVC). Medial retraction and cephalad rotation of the inferolateral edge raises the liver off the IVC.
■ A variable number of short hepatic vein branches drain the right hepatic lobe directly into the IVC. These should be carefully ligated using 4-0 ties and clips. We avoid use of clips on the hepatic side of these small vessels as they may interfere with parenchymal transection and reserve their use for the branches on the caval side.
■ At the proximal and lateral aspect of the IVC, there is a ligamentous band/parenchymal bridge, which extends from segment 7 to the retroperitoneal tissue behind the IVC. Release of this band is critical in the exposure and safe dissection of the RHV. This band can be vascular and transection should be performed by ligation, stapling, or use of bipolar transection of this tissue.
Hilar Dissection and Vascular Control
■ Anterior and cranial fixation of the falciform ligament exposes the hilum.
■ Antegrade cholecystectomy is performed to expose the right lateral hilar plate.
■ IOUS should be used routinely to examine the hepatic parenchyma for known and occult lesions. IOUS confirms vascular anatomy, identifies major vascular branches, and maps the proximity of hepatic and portal vein branches near the lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








