■ PNETs appear as hypervascular lesions on thin-slice CT or MRI scans. Somatostatin receptor scintigraphy (SRS) has a high sensitivity for most PNETs, with the exception of insulinomas. EUS may further characterize lesions near the pancreatic head, which typically have a hypoechoic appearance compared to normal pancreatic parenchyma. FNA or core needle biopsy sampling can confirm the presence of PNETs with immunohistochemical staining of cell block or tissue for chromogranin. Functional tumors are diagnosed on a biochemical basis.
■ MCAs are typically seen in younger women and may contain loculated lesions with multiple septae. More commonly, however, these lesions are seen as larger unilocular cysts. EUS and FNA reveal viscous, mucinous fluid with high carcinoembryonic antigen (CEA) levels and low amylase.
■ SCAs may contain a “starburst” or honeycomb pattern of central scarring on CT imaging. EUS reveals a characteristic thin-walled capsule with thin septae. If FNA is performed, it often yields serous fluid with low amounts of CEA and mucin.
■ SPTs present in young females (mean age 25 to 30 years) typically as a large mass in the body or tail. These lesions contain hypodense areas representing sloughed, necrotic papillary stalks with internal calcifications. FNA with immunostaining may reveal neuron-specific enolase, vimentin, and α1-antitrypsinase expression. Aggressive surgical resection is warranted even in the presence of local invasion or metastatic disease.3,4
■ IPMNs are diagnosed with CT or MRCP. EUS with FNA reveals high amylase and CEA levels. Additionally, K-ras mutation and loss of heterozygosity are malignant characteristics. Endoscopic retrograde cholangiopancreatography (ERCP) will show continuity with the main pancreatic duct.
SURGICAL MANAGEMENT
Preoperative Planning
■ A complete history and physical of any patient undergoing central pancreatectomy is essential, paying close attention to signs of malignancy including weight loss or new-onset diabetes. A prior history of jaundice or pancreatitis should also be solicited. Basic blood chemistries should be obtained as well as a hepatic function panel, complete blood count, and coagulation studies. Serum tumor markers, including CEA, carbohydrate antigen (CA 19-9), and α-chromogranin should be obtained. When indicated, additional studies to characterize functional PNETs are warranted.
■ Central pancreatectomy may be considered for lesions less than 3 cm located deep within the pancreatic neck or proximal body or situated near the main pancreatic duct; such lesions are not amenable for enucleation. The length of remnant distal pancreas should maximize functional endocrine tissue. To this effect, recommendations from Iacono et al.5 include a minimum length of 5 cm for the distal pancreatic stump.
■ Contraindications to resection include evidence of invasive malignancy and chronic or focal pancreatitis not involving the pancreatic neck or body. Importantly, central pancreatectomy is contraindicated when the tail of the pancreas receives its only blood supply from the transverse pancreatic artery, as this will be ligated during the operation.5
POSITIONING
■ The patient is placed in supine position, with the table placed into slight reverse Trendelenburg. Two large-bore peripheral intravenous (IV) lines should be established and, if the patient has cardiovascular comorbidities, arterial blood pressure monitoring is advisable.
TECHNIQUES
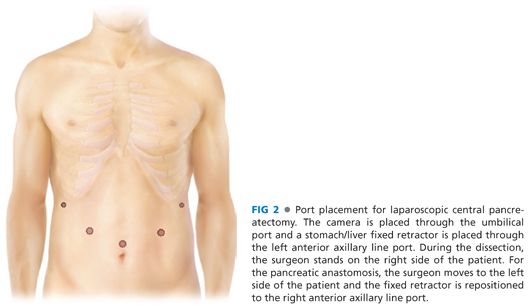
■ Laparoscopic central pancreatectomy has been reported by experienced surgeons to be feasible and safe. Port site placement for a minimally invasive approach is shown in FIG 2. The minimally invasive operation proceeds in the order described in the following text.
EXPOSURE OF THE PANCREAS
■ Obtain adequate exposure to the upper abdomen through a midline celiotomy or, alternatively, a bilateral subcostal incision. Thoroughly explore the abdomen to exclude metastatic or other disease.
■ Divide the gastrocolic ligament to enter the lesser space. Preserve the gastroepiploic vasculature; this will lead you to the insertion of the right gastroepiploic artery into the superior mesenteric vein. Divide any congenital adhesions between the gastric antrum and the body of the pancreas. Continue this dissection working left to right until you reach the level of the gastroepiploic vein.
■ Mobilize the proximal transverse mesocolon to fully expose the head of the pancreas (HOP) and the second and third portions of the duodenum. Then, establish the plane between the gastroepiploic vascular pedicle and the transverse mesocolon to expose the pancreatic neck and superior mesenteric vein (FIG 3).

■ Dissect the superior border of the pancreas. Divide the hepatoduodenal ligament to expose the common hepatic artery (CHA) and the associated lymphatics. Sharply dissect down to the anterior adventitia of the CHA. Continue the dissection distally, establishing a plane between the CHA and the cephalad aspect of the pancreatic body and neck. The gastroduodenal artery is your landmark for the distal extent of the dissection. Beyond this landmark, pancreatic transaction risks injury to the intrapancreatic bile duct.
PREPARING FOR RESECTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








