■ Our discussion here is limited solely to choledochojejunostomy.
DIFFERENTIAL DIAGNOSIS
■ Choledochal cyst excision (type I, II, or III)
■ Repair of CBD strictures
■ Repair after traumatic or iatrogenic injury of the CBD
■ Diversion of biliary flow in the presence of distal obstruction or pending obstruction for palliation
■ Orthotopic liver transplantation
■ Reestablishing biliary continuity after resection of benign or malignant disease, including biliary, ampullary, duodenal, or pancreatic head neoplasms
PATIENT HISTORY AND PHYSICAL FINDINGS
■ A thorough medical history and physical exam is important in determining the possible etiology causing the need for reestablishing biliary continuity. The overall health of the patient must be considered in determining whether the patient is a surgical candidate. Past surgical history is essential to identifying those patients at risk of iatrogenic strictures.
■ Symptoms of easy bruising, pruritus, acholic stools, nausea, vomiting, right upper quadrant pain, fevers, chills, mental status changes, and weight loss are important indicators of hepatic dysfunction and biliary obstruction.
■ Physical exam findings of abdominal mass, abdominal pain, abdominal surgical scars, jaundice, and scleral icterus should be sought. Additionally, indicators of cholangitis should be identified and rapidly treated: Charcot’s triad (right upper quadrant abdominal pain, jaundice, and fever) or Reynolds’ pentad (Charcot’s triad findings plus mental confusion and septic shock) indicate the need for preoperative biliary drainage.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Hilar anatomy must be evaluated prior to surgery, identifying any aberrant biliary or arterial anatomy and elucidating the possible etiology, site of injury, extent of obstruction, and planned surgical approach needed.
■ Contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) should be used to properly identify the anatomy and assess for potential vascular involvement in neoplastic processes or injury in iatrogenic biliary injuries. Magnetic resonance cholangiopancreatography (MRCP) is particularly useful to elucidate the biliary and pancreatic ductal anatomy and adjacent structures (FIG 2). Imaging is useful and often helpful in predicting the etiology of benign or malignant neoplasms. Image-guided percutaneous approaches with ultrasound or CT guidance may enable tissue biopsy of suspicious lesions.

■ Evaluation with endoscopic ultrasound (EUS) or with endoscopic retrograde cholangiopancreatography (ERCP) offers another method to assess the anatomy and for tissue biopsy (FIG 3).

■ In cases of cholangitis or biliary obstruction, biliary decompression by ERCP or percutaneous transhepatic cholangiography (PTC) may be warranted prior to surgical repair. It should be noted that biliary stenting in the face of asymptomatic mild to moderate hyperbilirubinemia, prior to elective surgery, may increase the postoperative risk of infection.1
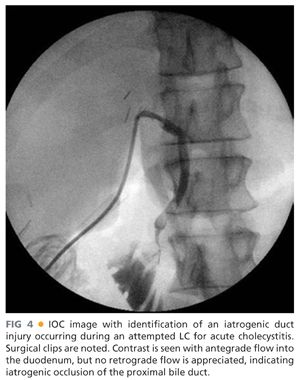
■ A previously obtained intraoperative cholangiogram (IOC) may be available and prove beneficial. Many cases of iatrogenic injuries occurring during laparoscopic cholecystectomy (LC) are identified by this technique (FIG 4).
SURGICAL MANAGEMENT
■ Indications include:
■ Bypass of distal or ampullary strictures.
■ Reconstruction after traumatic or iatrogenic injuries.
■ Reconstruction following Choledochal cyst excision (type I, II, or III).
■ Benign or malignant disease: biliary, ampullary, duodenal, or pancreatic head neoplasms. It can be included for palliative diversion or following resection.
■ Reconstruction during Orthotopic Liver transplantation.
Preoperative Planning
■ Standard optimization of comorbidities should be managed as permitted; for example, diabetes, hypertension, and cardiopulmonary status.
■ Coagulation disorders, if present, should be corrected with vitamin K as required.
■ In the appropriately selected jaundiced patient, preoperative stenting via ERCP and/or PTC may be necessary.
■ Cholangitis, if present, should be treated with appropriate drainage and antibiotics. Common biliary pathogens include Escherichia coli, Klebsiella spp, Enterococcus spp, streptococci, Enterobacter spp, and Pseudomonas aeruginosa.
■ In the absence of cholangitis, preoperative antibiotics should be given, and expanded in the presence of biliary stenting due to the increased risk of biliary contamination, even in asymptomatic patients.
■ In malnourished patients, nutritional support may be considered preoperatively and continued into the postoperative period to minimize postoperative complications. Adequate nutrient absorption may be hindered preoperatively due to biliary blockage or diversion.
■ In the face of malignant disease, preoperative workup should also be tailored to the assessment of the type and extent of disease present. Surgical resectability is of primary concern in malignant processes; however, choledochojejunostomy may be undertaken as a palliative biliary diversion in unresectable malignancies.
Positioning
■ Patient is placed in supine position with both arms at 90 degrees, ensuring pressure points are protected and padded (FIG 5).

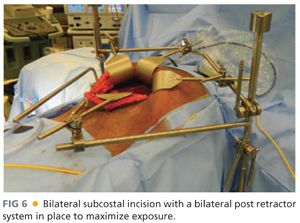
■ We use a bilateral post, framed retractor system (FIG 6) to maximize exposure via a bilateral subcostal incision.
TECHNIQUES
PLACEMENT OF INCISION AND OPERATIVE EXPOSURE
■ A bilateral subcostal incision provides optimal exposure. Once the peritoneum is entered, adhesions are cleared if present, and the falciform ligament is divided between ties or with an energy device. This further exposes the operative field and permits retractor placement (FIG 6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








