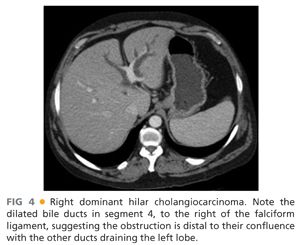
■ The resection may also include the caudate lobe and all the biliary ducts to the right of the umbilical fissure. This is most frequently indicated in hilar cholangiocarcinoma patients.
DIFFERENTIAL DIAGNOSIS
■ Cholangiocarcinoma
■ Metastatic carcinoma
■ Hepatocellular carcinoma
■ Gallbladder cancer
■ Liver trauma
PATIENT HISTORY AND PHYSICAL FINDINGS
■ Attention must be given to the potential for underlying liver disease. The intended hepatic remnant following right trisegmentectomy is inadequate.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Triphasic, contrast-enhanced abdominal computed tomography (CT) scan
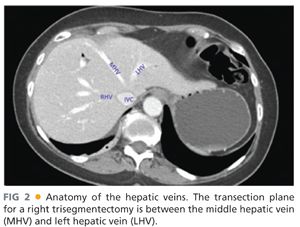
■ Its main value is to identify the vascular structures involved, anatomic variations in the hilar vasculature, and margins to be preserved at the time of surgery (FIG 2).
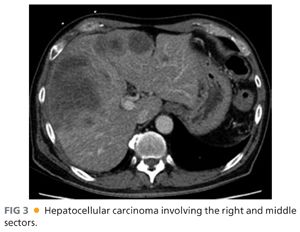
■ Examples of CT scans from patients with hepatocellular carcinoma involving the right side and middle segments (FIG 3) and a right dominant hilar cholangiocarcinoma are shown (FIG 4).
■ Abdominal magnetic resonance imaging (MRI) with contrast and delayed liver phase
■ Equivalent to a contrast CT scan; slightly better at defining parenchyma abnormalities and in differential diagnosis
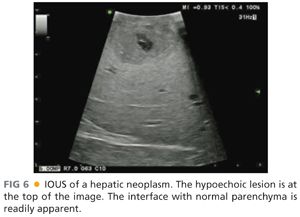
■ Intraoperative ultrasound (IOUS)
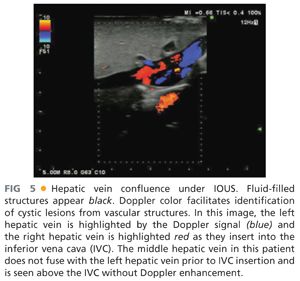
■ Essential tool and skill needed during liver surgery. IOUS helps define margins, identify smaller lesions (<1 cm), and visualize the portal pedicles and hepatic veins (FIGS 5 and 6).
SURGICAL MANAGEMENT
Preoperative Planning
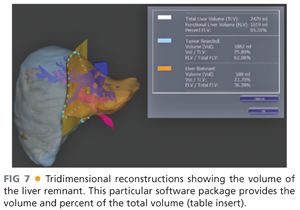
■ The volume of the intended remnant liver should to be calculated with preoperative imaging and considered against the patient body weight. The author favors 3-D reconstruction of a CT scan with software rendition of the remnant volume (FIG 7).
■ The functional capacity of the remnant liver should be estimated.
■ Portal vein (PV) embolization of the right lobe (and occasionally segment 4) is often indicated.
■ If PV embolization is performed, CT scan volumetrics are repeated 3 to 4 weeks postembolization to assess for adequate hypertrophy of the planned liver remnant.
■ Low-volume intraoperative resuscitation reduces blood loss. This approach requires preoperative communication with the preoperative nursing staff and anesthesiologist.
■ Regional anesthesia approaches, such as epidural catheters, reduce pain scores and respiratory complications.
■ Preoperative steroid (100 mg intravenous [IV] methylprednisolone) is associated with reduced peaks of liver injury test values but not improved outcomes.
Positioning
■ The patient is placed in a supine position. Tucking the right arm is optional, depending on the retractor to be used.
■ The patient is prepped from the nipples to the pubis on both sides.
■ The authors routinely place an arterial line and central venous line.
TECHNIQUES
INCISION
■ A number of options are possible (FIG 8) for appropriate exposure to perform a right trisegmentectomy.
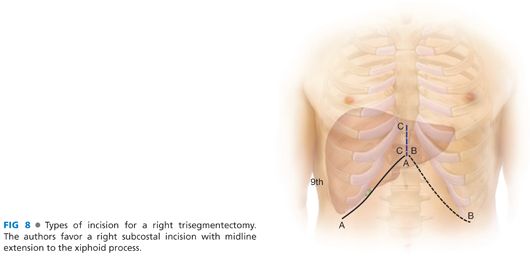
■ Bilateral, subcostal incision with upper midline extension (A + B + C)
■ A right-sided, hockey stick–type incision (A + C)
■ In children, a flat bilateral incision can be used (A + B).
■ Removal of the xiphoid process is optional in order to get a better exposure of the suprahepatic abdominal vena cava.
EXPOSURE
■ A Thompson retractor facilitates the application of adequate tension of the costal margin to provide exposure to the hepatic veins and suprahepatic vena cava.
HILAR PALPATION
■ Bimanual palpation of the hilar structures through the foramen of Winslow quickly defines the arterial anatomy (FIG 9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








