Christopher R. Chapple, MD, FRCS (Urol), FEBU
Stress incontinence is a symptom, a sign, and a clinical diagnosis; the clinical symptom is that of involuntary loss of urine associated with increased intra-abdominal pressure, such as occurs during coughing and sneezing. The International Continence Society (ICS) defines urodynamic stress incontinence as the involuntary loss of urine during increased intra-abdominal pressure during filling cystometry, in the absence of detrusor (bladder wall muscle) contraction (Abrams et al, 2002). Thus, urodynamic evaluation is a prerequisite for the diagnosis of urodynamic stress incontinence. Therefore, in discussing stress incontinence, this review refers to women with stress urinary incontinence (SUI) diagnosed on the basis of symptoms alone or urodynamically proven, so-called urodynamic stress incontinence.
Treatment options for SUI include conservative techniques and both pharmacologic and surgical interventions. Surgical procedures to treat SUI generally aim to improve the support to the urethrovesical junction and to correct deficient urethral closure. There is a contemporary lack of consensus, however, regarding the precise mechanism by which continence is achieved in the “normal asymptomatic female” and therefore not surprisingly in how “normality” is restored by surgical manipulation. Anti-incontinence surgery is generally used to address the failure of normal anatomic support of the bladder neck and proximal urethra and intrinsic sphincter deficiency. Anti-incontinence surgery does not necessarily work by restoring the same mechanism of continence that was present before the onset of incontinence. Rather, it works by a compensatory approach, creating a new mechanism of continence (Jarvis, 1994a).
Therapeutic Options
The surgeon’s preference, coexisting problems, and anatomic features of the patient and her general health condition influence the choice of procedure. Numerous surgical methods have been described, but they essentially fall into seven categories (Table 71–1).
This wide variety of treatment options for stress incontinence indicates the lack of a clear consensus as to which procedure is the most effective. Several groups have reviewed the literature, often using systematic and methodical analyses of well-designed randomized controlled trials (Jarvis, 1994b; Black and Downs, 1996; Fantl et al, 1996; Leach et al, 1997; Moehrer et al, 2002, 2003; Lapitan et al, 2003). Most of these reviews, however, are hampered by the quality of the existing evidence base, and these reviews are based on studies of mixed quality with little standardization of the points in Table 71-2.
Table 71–2 Standardization Needed for Studies
A review of existing literature on confounding variables affecting outcome of therapy (Smith et al, 2005) concluded the following:
Choice of Surgical Technique
Differentiating Relative Contributions of Hypermobility and Intrinsic Sphincter Deficiency
The influence of urethral function defined by leak point pressure or maximum urethral closure pressure (MUCP) is difficult to define on account of the large variation in outcome measures employed. Furthermore, other variables such as urethral mobility are often not controlled. Intrinsic sphincteric deficiency (ISD) is usually defined as a leak point pressure of less than 60 or MUCP of less than 20. A standardized test is not available to differentiate the relative contributions of intrinsic sphincter deficiency and hypermobility; therefore few studies have been able to accurately separate their individual contributions to the development of incontinence (Chapple et al, 2005). Retropubic procedures act to restore the bladder neck and proximal urethra to a fixed, retropubic position and are used when hypermobility is believed to be an important factor in the development of that woman’s stress incontinence. This may facilitate the function of a marginally compromised intrinsic urethral sphincter mechanism, but if significant intrinsic sphincter deficiency is present it is likely that SUI will persist despite efficient surgical repositioning of the bladder neck and proximal urethra; at present this hypothesis remains unproven. In such circumstances then a sling procedure (particularly a “snug” fascial sling) or an artificial sphincter is most likely to be the therapy of choice.
In the normal continent woman, the bladder neck and proximal urethra are supported in a retropubic position, with the bladder base being dependent. Increases in intra-abdominal pressure are transmitted to both the bladder and the proximal urethra such that the pressure difference between the two is unchanged, promoting continence (Einhorning, 1961). A valvular effect at the bladder neck created by the transmission of abdominal pressure to the dependent bladder base may also be operative here (Penson and Raz, 1996). Furthermore, with proper bladder neck support, reflex contraction of the pelvic floor muscles during Valsalva maneuvers and coughing acts as a backboard for urethral compression (Staskin et al, 1985).
Surgical Procedures
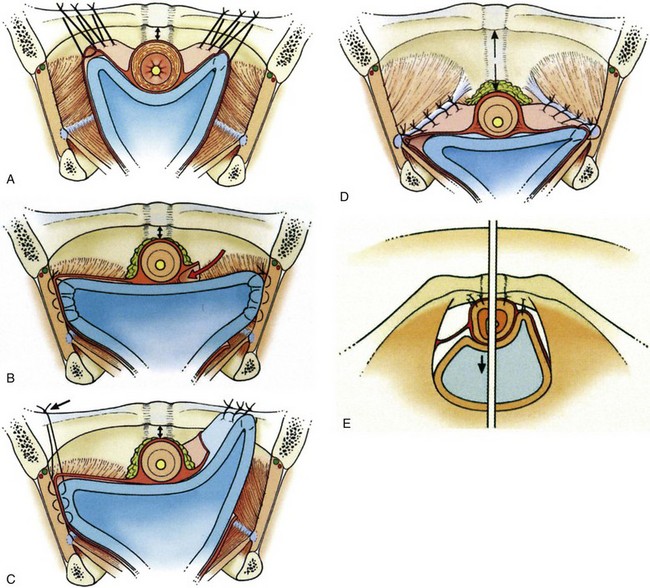
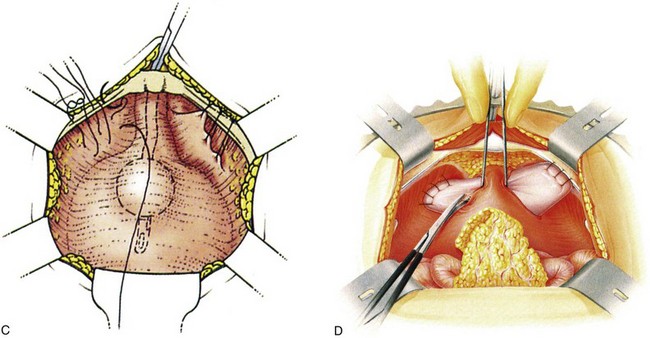
The Burch colposuspension (Fig. 71–1A) is the elevation of the anterior vaginal wall and paravesical tissues toward the iliopectineal line of the pelvic sidewall with use of two to four sutures on either side (Burch, 1961). The VOS repair (see Fig. 71–1B) aims to anchor the vagina to the internal obturator fascia and is a modification of a combination of the Burch and paravaginal defect repair, with placement of the sutures laterally anchored to the internal obturator fascia rather than hitching the vagina up to the iliopectineal line (Turner-Warwick, 1986), although a more recent modification does, where appropriate, insert sutures into both the internal obturator and iliopectineal line (see Fig. 71–1C). The paravaginal defect repair (see Fig. 71–1D) aims to close a presumed fascial weakness laterally at the site of attachment of the pelvic fascia to internal obturator fascia (Richardson et al, 1976). The MMK procedure (see Fig. 71–1E) is the suspension of the vesicourethral junction (bladder neck) toward the periosteum of the symphysis pubis (Marshall et al, 1949) and was thought to act by buttressing the paraurethral area and bringing the vesicourethral junction into a more elevated “intra-abdominal” position.
The Degree of Urethral Elevation
The extent of the urethral elevation achieved by both the Burch (see Fig. 71–1A) and the VOS suspensions (see Fig. 71–1B and C) is higher than the arcus tendineus anchorage of the paravaginal defect repair (see Fig. 71–1D).
The Configuration of the Suspensions
A particular advantage of the horizontal urethral elevation achieved by both the VOS and the paravaginal repair suspensions is the significantly less susceptibility to tension on the urethra and to obstructive problems than with the V-shaped configuration of the Burch suspension (see Fig. 71–1A).
Tissue Approximation
Both the VOS and the paravaginal repair suspensions are anchored by tissue-approximating sutures; thus, unlike the Burch colposuspension, neither the VOS nor the paravaginal repair suspension is suture dependent in the longer term once the initial healing is complete because there is direct tissue adhesion. The VOS anchorage and suspension is significantly more robust than that of the paravaginal defect repair; the elevation it achieves can be further augmented by additionally including the iliopectineal ligament in the upper sutures (see Fig. 71–1C).
Laparoscopic colposuspension is the most popular of the laparoscopic incontinence procedures that were first introduced in the early 1990s (Vancaillie and Schuessler, 1991) with the premise that as minimally invasive procedures they would benefit patients by avoiding the major incision of conventional open surgery and shorten the time for a return to normal activity. As in open colposuspension, sutures are inserted into the paravaginal tissues on either side of the bladder neck and then attached to the iliopectineal ligaments on the same side. There are, however, technical variations in surgery with respect to the laparoscopic approach (transperitoneal into the abdominal cavity or extraperitoneal) and in the number and types of sutures, the site of anchor, and the use of mesh and staples (Jarvis et al, 1999).
Assessing Outcomes of Therapy
Duration of Follow-up
It is recognized that prolonged follow-up is required to assess the true benefit of an incontinence procedure. Short-term follow-up should be considered to have begun in all studies after participants have reached 1 year of follow-up (Abrams et al, 2005). In the short term (2 years), most procedures are successful and success rates between procedures are similar (Leach et al, 1997). However, with longer follow-up (>5 years), failures become manifest and the true benefit of the better procedures is realized. Most studies report outcomes after short-term follow-up, and thus results must be interpreted with caution.
The Issue of Intrinsic Sphincter Deficiency
There is no consistency in the existing literature database to support the likelihood that intrinsic sphincter deficiency can influence either the outcomes or the type of surgical treatment. The main problem is that there is no consensus on the meaning of intrinsic sphincter deficiency and how to diagnose it (Smith et al, 2005, 2009). Nevertheless it is likely in the author’s view (unsubstantiated by any unequivocal evidence) that mild degrees of intrinsic sphincter deficiency coexist with hypermobility in most cases. In a situation in which intrinsic sphincter deficiency is the predominant problem, then a repositioning procedure such as a colposuspension is less likely to be successful than a tight fascial sling or artificial sphincter.
The Definition of Cure
Finally, one must question whether the goal of complete continence is reasonable, given that the condition of SUI is generally a degenerative one and corrective surgery does not replace the defective components. As well, even in normal healthy women, urinary continence is a spectrum of dryness; approximately 40% of nulliparous 30- to 49-year-olds experience some degree of incontinence with exercise (Nygaard et al, 1990). It seems unreasonable to expect surgery for a degenerative condition to achieve results that are better than the nondegenerative state.
The Patient’s versus the Physician’s Perspective
A patient’s satisfaction with treatment is often based on the difference between her expectations and her experiences (Sofaer and Firminger, 2005). Thus, fulfillment of positive expectations is a key element of a patient’s satisfaction (Sitzia and Wood, 1997). Because expectations vary widely, satisfaction is not a standard concept. Consequently, treatment plans must be tailored to meet a nonstandard goal. An integral step in achieving this goal is the development of a patient-physician partnership that promotes the negotiation of realistic expectations.
Logically, agreement of patient and physician with respect to treatment plan and goals should improve outcomes. When a diagnosis has been made, asking patients what they already know about the condition may give clues to expectations for treatment. The “ask-tell-ask” method may be employed to mend the gaps between the physician’s and the patient’s expectations. The physician explains the proposed treatment plan and expectations for the outcome, then encourages the patient to ask questions. The physician provides the information requested and invites questions again, continuing the process until a mutual understanding of treatments and expectations is reached (Barrier et al, 2003). This approach may prevent “surprises” such as unexpected pain of treatment, adverse events of medication, and prolonged recovery time. Elkadry and associates (2003) emphasized this point by demonstrating a significant association between feeling unprepared for surgery and the patient’s dissatisfaction after pelvic reconstruction. The same investigators also reported that achievement of patient-defined goals was more predictive of a patient’s satisfaction than were objective measures of surgical success.
Whereas many, including the author, think that urodynamic studies are helpful in defining the underlying pathophysiologic process in cases with incontinence, they have not been proved to have adequate sensitivity, specificity, or predictive value (Chapple et al, 2005). The ICI meeting concluded that although urodynamic studies, such as frequency-volume charts and pad tests, are useful there is inadequate evidence to justify pressure-flow studies for routine testing as either entry criteria or outcome measures in clinical trials. It was recommended that most large-scale clinical trials enroll subjects by using carefully defined symptom-driven criteria when the treatment will be given on an empirical basis (Abrams et al, 2005).
Indications for Retropubic Repair
The treatment of SUI in women must be tailored to the individual patient. Once evaluation has identified contributing factors, a trial of conservative therapy should be pursued and surgery considered for patients who fail to respond to these conservative measures. Careful assessment of the patient is essential in making an accurate diagnosis (Fig. 71–2).
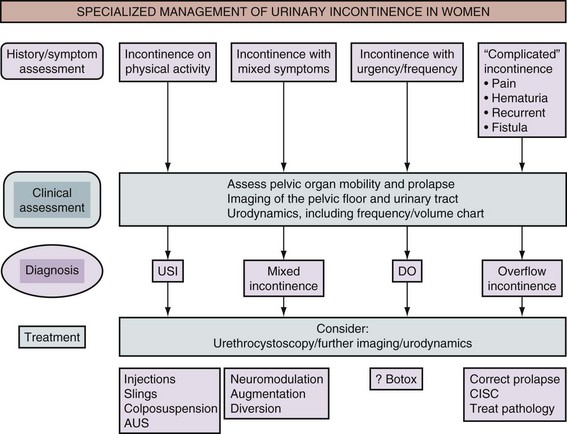
Figure 71–2 Algorithm for the specialized management of stress urinary incontinence (after the Third International Consultation on Incontinence, Monaco [Abrams et al, 2005]). USI, urodynamic stress incontinence; DO, detrusor overactivity; AUS, artificial urinary sphincter; CISC, clean intermittent self-catheterization.
The selection of technique is largely based on the surgeon’s preference and prior experience; bladder base and urethral hypermobility may be surgically corrected by either a vaginal or a retropubic approach. Although it has been suggested that a retropubic colposuspension should be considered in patients who frequently generate high intra-abdominal pressure (e.g., those with chronic cough from obstructive pulmonary disease and women in strenuous occupations) (Appell, 1993), it could also be argued that these patients may be better served by a pubovaginal sling as well.
Potential Contraindications
If there is a history of prior failed incontinence procedures the existence of significant sphincteric deficiency must be suspected, even if hypermobility exists, and consideration given to performing a pubovaginal sling, although retropubic colposuspensions may be successful in this scenario as well (Cardozo et al, 1999; Maher et al, 1999; Nitahara et al, 1999).
In the author’s view, when SUI exists solely due to intrinsic sphincter deficiency (i.e., a fixed, nonfunctional proximal urethra with intrinsic urethral sphincter dysfunction), a retropubic suspension procedure is less likely to be successful because there is no hypermobility to correct and the patient is better served by a pubovaginal sling, collagen injections, or an artificial sphincter (Bergman et al, 1989b). This represents a personal view that is at variance with the ICI’s conclusion statement on the role of urethral occlusive forces, which reads as follows: “It would appear that a low leak point pressure is less predictive of outcome on this data when compared to the presence or absence of urethral hypermobility” (Smith et al, 2009).
A retropubic colposuspension is contraindicated when there is an inadequate vaginal length or mobility of the vaginal tissues, for example, after prior vaginal surgery or radiotherapy or such as that after a prior vaginal incontinence procedure (Appell, 1993). The lysis of retropubic adhesions can be performed adequately and safely by a vaginal approach in conjunction with a needle suspension procedure or pubovaginal sling.
Vaginal versus Retropubic Surgery
From a review of the literature there is clearly a difference in the success rate of vaginal versus retropubic surgery alone with respect to correction of stress incontinence. An anterior colporrhaphy can certainly be efficacious for the correction of prolapse, with a reported efficacy in randomized controlled studies of 42% and 57% in the management of cystoceles (Sand et al, 2001; Weber et al, 2001). For the treatment of both a cystocele and SUI, an anterior colporrhaphy should be combined with a sling procedure. Goldberg and colleagues (2001), in a case-control series, demonstrated that in women with a cystocele and SUI the addition of a pubovaginal sling to an anterior colporrhaphy significantly decreased the recurrence rate from 42% in the control group to 19% in the anterior colporrhaphy group.
Glazener and Cooper (2001) reviewed the literature on randomized or quasi-randomized trials that included anterior vaginal repair for the treatment of urinary incontinence. Nine trials were identified that included 333 women having an anterior vaginal repair and 599 who received comparison interventions. They concluded that anterior vaginal repair was less effective than open abdominal retropubic suspension on the basis of patient-reported cure rates in eight trials both in the medium term (failure rate within 1 to 5 years after anterior repair, 97 of 259 [38%] versus 57 of 327 [17%]; relative risk [RR], 2.29; 95% confidence interval [CI], 1.7 to 3.08) and in the long term (after 5 years, 49 of 128 [38%] versus 31 of 145 [21%]; RR, 2.02; 95% CI, 1.36 to 3.01). There was evidence from three of these trials that this was reflected in a need for more repeated operations for incontinence (25 of 107 [23%] vs. 4 of 164 [2%]; RR, 8.87; 95% CI, 3.28 to 23.94). These findings held irrespective of the coexistence of prolapse (pelvic relaxation), although fewer women had a prolapse after anterior repair (RR, 0.24; 95% CI, 0.12 to 0.47) and later prolapse operation appeared to be equally common after either a vaginal (3%) or an abdominal (4%) operation.
Long-term follow-up beyond the first year is available in only three randomized controlled trials (Bergman et al, 1989a; Liapis et al, 1996; Colombo et al, 2000). There is a low morbidity with vaginal repair, but long-term success rates decrease with time to the extent that a 63% cure rate at 1 year fell to 37% at 5 years of follow-up (Bergman and Elia, 1995).
The recommendation from the ICI committee (Smith et al, 2009) is that anterior colporrhaphy should not be used in the management of SUI alone (grade A).
General Technical Issues
Retropubic Dissection
In open retropubic suspension procedures good access to the retropubic space is crucial. This is best performed with the patient in the supine position with the legs abducted, in either a low or a modified dorsal lithotomy position with the use of stirrups, allowing access to the vagina during the procedure and a perineal-abdominal progression. A urethral Foley catheter is inserted; the catheter balloon is used for subsequent identification of the urethra and bladder neck, and, indeed, it is invaluable in allowing palpation of the edges of the bladder by appropriate manipulation. A Pfannenstiel or lower midline abdominal incision is made, separating the rectus muscles in the midline and sweeping the anterior peritoneal reflection off the bladder. It is essential to optimize the access to the retropubic space, and if a Pfannenstiel skin incision is made it is advisable to use the suprapubic V-shaped modification described by Turner-Warwick and colleagues (1974). Likewise, whatever incision is made, extra valuable access to the retropubic space is obtained by extending the division of the rectus muscles down to the pubic bone and elevating the aponeurotic insertion of the rectus muscle off the upper border of the pubic bone.
The retropubic space is then developed by teasing away the retropubic fat and underlying retropubic veins from the back of the pubic bone. The bladder neck, anterior vaginal wall, and urethra are then easy to identify, often facilitated by the presence of the Foley balloon. In patients who have had previous retropubic surgery, the dissection is performed sharply and it is important to take down all old retropubic adhesions, particularly in the presence of a prior failed repair. If difficulty is encountered in the identification of the bladder neck, the bladder may be partially filled or even opened to identify its limits and an examining finger in the vagina is invaluable in aiding the dissection (Symmonds, 1972; Gleason et al, 1976).
Suture Material
Absorbable sutures were used in the original descriptions of the MMK procedure (chromic catgut), Burch colposuspension (chromic catgut), and VOS procedure (polyglycolic acid or polydioxanone), whereas the original paravaginal repair used nonabsorbable sutures (silicon-coated Dacron). Fibrosis during subsequent healing is likely to be the most important factor in providing continued fixation of the perivaginal fascia to the suspension sites (Tanagho, 1996); nevertheless, some surgeons believe that a nonabsorbable suture material is better because of the risk of suture dissolution before the development of adequate fibrosis (Penson and Raz, 1996). Clearly, the choice of suspension suture material is a personal choice, but erosion of nonabsorbent sutures into the lumen of the bladder is a not uncommon complication and a not uncommon source of medical litigation (Woo et al, 1995).
Bladder Drainage
Some degree of immediate postoperative voiding difficulty can be expected after retropubic suspensions (Lose et al, 1987; Colombo et al, 1996a). Immediately postoperatively, bladder drainage may take the form of a urethral or a suprapubic catheter, generally based on the surgeon’s preference. A voiding trial is usually performed around the fifth day postoperatively. However, there is some evidence that a suprapubic catheter may be advantageous with respect to a lower incidence of asymptomatic and febrile urinary tract infection and earlier resumption of normal bladder function (Andersen et al, 1985; Bergman et al, 1987). In addition, the use of a suprapubic tube is generally more comfortable, allows the patient to participate in catheter management, and avoids the need for clean intermittent self-catheterization. Catheterization can be discontinued when efficient voiding has resumed, which is usually indicated by a postvoid residual urine volume either less than 100 mL or less than 30% of the functional bladder volume.
Marshall-Marchetti-Krantz Procedure
Technique
Marshall, Marchetti, and Krantz in 1949 described a retropubic approach for the elevation and fixation of the anterolateral aspect of the urethra to the posterior aspect of the pubic symphysis and the adjacent periosteum. Technically, the original description of the MMK procedure reported a double suture bite of the paraurethral tissue included with the vaginal wall; this may be generically entitled a cystourethropexy. In 1949, Marshall and coworkers described their retropubic vesicourethral suspension in 50 patients; 38 of the patients had symptoms of SUI, 25 of whom had failed prior gynecologic operations for urinary incontinence. A simple suprapubic procedure was described by which the vesical outlet was suspended to the pubis (Marshall et al, 1949). In the original description, three pairs of sutures (taking double bites of tissue) were placed on each side of the urethra, incorporating full-thickness vaginal wall (excluding mucosa) and lateral urethral wall (excluding mucosa) (Marshall et al, 1949). Marchetti (1949) then modified the procedure to omit the tissue bite through the urethral wall because of concern about urethral injury. Apart from modifications in suture number and material over the years, the procedure remains the same today.
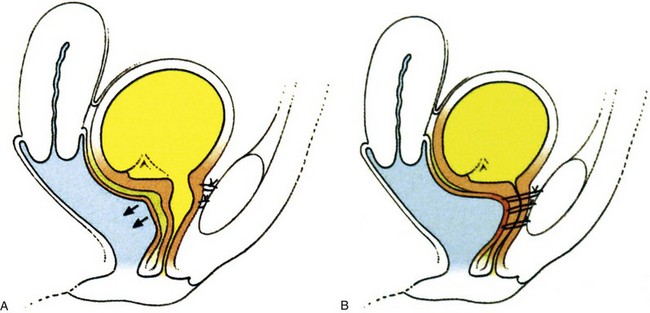
Cystourethropexy was often used as a secondary procedure for the resolution of persistent leaking after an anterior colporrhaphy. A cystourethropexy does not support the posterior wall of the urethra unless the sutures include the paraurethral vaginal wall, nor does it positively reduce an anterior vaginal wall prolapse in the same way that the true retropubic colposuspension procedures do. If there is a significant urinary residual after colporrhaphy with associated laxity of the anterior vagina wall, then with the descent, this applies traction to the posterior aspect of the bladder neck and tends to “tent” it open because the anterior aspect is tethered by sutures to the back of the pubis (see Fig. 71–1E). Sutures are placed on either side of the urethra (avoiding the urethral wall), taking bites through the paraurethral fascia and anterior vaginal wall (excluding mucosa). The most proximal sutures are placed at the level of the bladder neck. Each suture is then passed into an appropriate site in the cartilaginous portion of the symphysis (Fig. 71–3). However, the main technical problem relating to the MMK procedure is the difficulty of obtaining an adequately robust anchorage of the anterior wall of the urethra and the paraurethral fascia to the symphysis and the periosteum of the pubis where the suture bites are relatively insecure. As shown in Figure 71–3 these sutures can potentially either distort the bladder neck and impair sphincter function (see Fig. 71–3A) or obstruct the bladder neck (see Fig. 71–3B). All sutures are inserted; and while an assistant elevates the anterior vaginal wall, each suture is individually tied, starting with the more distal pair. The proximal, or bladder neck, suture frequently needs to be passed through the insertion of the rectus abdominis. Additional sutures may or may not be placed between the anterior bladder wall and the rectus muscles to pull the bladder farther anteriorly.
Results
Krantz described a personal series of 3861 cases with a follow-up of up to 31 years and a 96% subjective cure rate (Smith et al, 2005). Short- and medium-term results with the MMK procedure have been good. Mainprize and Drutz (1988) reviewed 58 articles (predominantly retrospective) published between 1951 and 1988 for treatment outcomes in 3238 cases. The cure rate, mostly based on subjective criteria, was 88%, with an improvement rate of 91%. Jarvis’s meta-analysis of studies in the literature (1994b) noted subjective continence in 88.2% (range, 72% to 100%) of 2460 patients with 1- to 72-month follow-up and objective continence in 89.6% (range, 71% to 100%) of 384 patients with 3- to 12-month follow-up. Whether the procedure was being done primarily or secondarily affected the outcome, with subjective continence in 92% if it was done primarily versus 84.5% if it was done secondarily. Longer-term data are limited in amount. McDuffie (1981) reported 75% success at 15 years. More recently, Clemens and coworkers (1998) noted subjective cure or improvement (SUI and urgency urinary incontinence) in only 41% of patients with a mean follow-up of 17 years, and Czaplicki and colleagues (1998) noted decreasing continence rates from 77% at 1 year to 57% at 5 years to 28% at 10 years, with a mean duration of continence of 78.5 months. There are significant limitations to the data since most series are retrospective, with preoperative assessment based mainly on the history and physical examination and few studies using objective data as outcome measures.
Complications occur in up to 21% of cases (Mainprize and Drutz, 1988), and the placement of sutures through the pubic symphysis incurs the risk of osteitis pubis, a potentially devastating complication of the MMK procedure that has been reported in 0.9% to 3.2% of patients (Lee at al, 1979; Mainprize and Drutz, 1988; Zorzos and Paterson, 1996). Patients usually present 1 to 8 weeks postoperatively with acute pubic pain radiating to the inner thighs, aggravated by moving. Physical examination reveals tenderness over the pubic symphysis, and radiography demonstrates haziness to the borders of the pubic symphysis and possibly lytic changes. Treatment is with bed rest, analgesics, and possibly corticosteroids (Lee at al, 1979). Other specific complications of the MMK procedure have included the occasional erosion of nonabsorbable cystourethropexy sutures into the bladder lumen with stone formation. Also, the positioning of sutures in the endopelvic fascia close to the bladder neck can result in a significant outlet obstruction.
Whereas the MMK procedure produces a cure rate similar to that of colposuspension, the complication of osteitis pubis means that there is little to support its use as an alternative to other colposuspension procedures. Indeed the ICI committee (Smith et al, 2009) concluded that although short-term results indicate comparable cure rates to colposuspension there is limited evidence that the longer-term outcome is poorer after MMK (level 1) and declines further over time (level 3). There is no evidence to support the continued use of MMK over colposuspension.
The recommendation from the ICI committee (Smith et al, 2009) is that the MMK procedure is not advised for the treatment of SUI (grade A).
Burch Colposuspension
Technique
Burch’s original description of the colposuspension in 1961 followed his original procedure, which was essentially a paravaginal repair attaching the paravaginal fascia to the white line of the pelvis, the arcus tendineus. The Burch colposuspension was a novel approach to restore the urethrovesical junction to a retropubic location by approximating the periurethral fascia to the tough bands of fibrous tissue running along the superior aspect of the pubic bone (Cooper [iliopectineal] ligament) with three pairs of sutures. The original Burch retropubic colposuspension is appropriate only if the patient has adequate vaginal mobility and capacity to allow the lateral vaginal fornices to be elevated toward and approximated to the Cooper ligament on either side. This technique has been modified. Tanagho’s modification (1978) approximated the vaginal wall to the lateral pelvic wall, with the sutures holding the anterior vaginal wall to the Cooper ligament, being tied loosely so that two fingers could be placed between the symphysis and urethra. This achieved broad support for the urethra and bladder neck and potentially minimized the risk of postoperative voiding dysfunction. A more recent modification (Shull and Baden, 1989; Turner-Warwick and Chapple, 2002) involves a hybrid approach whereby the vaginal tissues are approximated to the internal obturator fascia with an anchoring bite to the iliopectineal ligament (see VOS repair later).
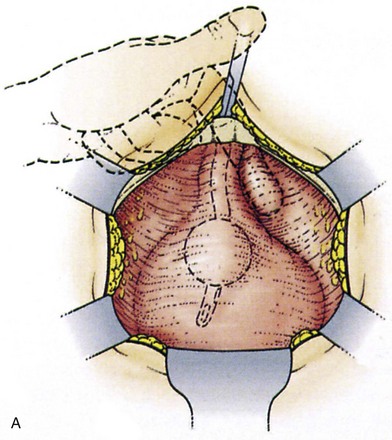
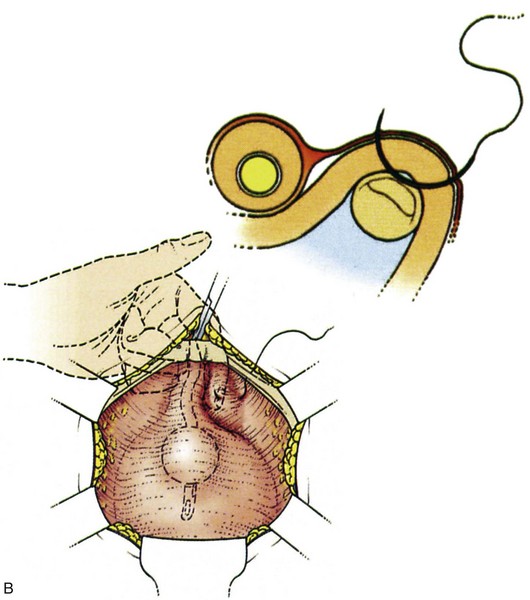
Suture placement is facilitated by the elevation of the dissected anterolateral vaginal wall into the field by the surgeon’s fingers inserted in the vagina (Fig. 71–4). The bladder is retracted to the opposite side with a mounted swab. Two to four sutures are placed on each side, each suture taking a good bite of fascia and vaginal wall, with care taken not to pass through the vaginal mucosa. Some recommend taking double bites of tissue to lessen the risk of suture pull-through (Jarvis, 1994a). The most distal suture is at the level of the bladder neck and placed no closer than 2 cm lateral to it, although some place distal sutures at the midurethral level (Tanagho, 1978). The suspension suture bites of the paraurethral fascia should not be positioned too close to the bladder neck and the urethra, as they are in the cystourethropexy procedures (MMK), because the unwanted effect of lateral traction-tension created by their anchorage to the iliopectineal ligaments may tether the sphincteric occlusive effect on the urethra or create a degree of obstructed voiding. Subsequent sutures are placed proximal to the level of the bladder neck, at about 1-cm intervals. The sutures are then placed into corresponding sites in the Cooper ligament, the emphasis being on a mediolateral direction for the sutures. The exact mechanism of continence of the Burch colposuspension is still unknown. Burch (1968) thought it to be secondary to elevation and stabilization of the bladder neck and urethra. In support of the suggestion regarding suture placement, Digesu and colleagues (2004) reviewed magnetic resonance imaging findings before and 1 year after open Burch colposuspension in 28 women to see if this would explain the mechanism. In the 86% who were cured the distance between the levator ani muscle and bladder neck was significantly shorter than in those whose treatment failed. Their suggestion is that insertion of sutures in a medial-lateral direction as opposed to an anteroposterior direction may better appose the levator ani muscle and bladder neck. The highly vascular vaginal wall may bleed profusely during suture placement, and large vaginal veins often need to be oversewn, but most bleeding ceases once the sutures are tied and the vagina is suspended. To facilitate tying of the sutures, the assistant elevates the appropriate portion of the vaginal wall as each suture is tied, beginning with the more distal pair.
No attempt should be made to tie the sutures tightly. Often, the vaginal wall does not approximate to the Cooper ligaments, and free suture material is seen between the vagina and the ligaments. The principle is to approximate the vaginal wall to the lateral pelvic wall, where it will heal and promote adhesion formation (Tanagho, 1978; Shull and Baden, 1989; Turner-Warwick and Chapple, 2002), thereby creating a broad support for the urethra and bladder neck.