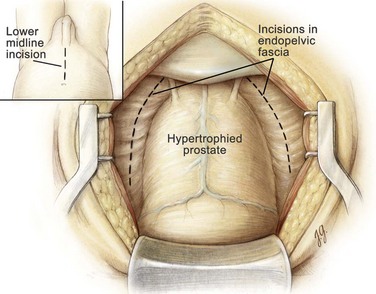
Misop Han, MD, MS, Alan W. Partin, MD, PhD The treatment options for bladder outlet obstruction due to benign prostatic hyperplasia have been expanded dramatically over the past 2 decades with the development of medical and minimally invasive therapies. The current medical therapies for lower urinary tract symptoms (LUTS) include selective long-acting α1-adrenergic antagonists, such as terazosin (Hytrin [Lepor et al, 1992; Roehrborn et al, 1996]), doxazosin (Cardura [Gillenwater et al, 1995]), and tamsulosin (Flomax [Abrams et al, 1995]), and the 5α-reductase blockers, such as finasteride (Proscar [Gormley et al, 1992; Andersen et al, 1995; Lepor et al, 1996]) and dutasteride (Avodart [Roehrborn et al, 2002, 2004]). Minimally invasive procedures include visual laser ablation of the prostate (VLAP [Cowles et al, 1995]), transurethral electrovaporization of the prostate (TVP [Kaplan et al, 1996]), transurethral needle ablation (TUNA [Schulman et al, 1993; Campo et al, 1997]), transurethral microwave thermotherapy (TUMT [Ogden et al, 1993; Javle et al, 1996]), interstitial laser coagulation (ILC [Muschter and Hofstetter, 1995]) and transurethral incision of the prostate (TUIP [Cornford et al, 1997]). However, these approaches are usually reserved for men with moderate symptoms and a small to medium-sized prostate gland (Reich et al, 2006). For larger prostate glands, open prostatectomy has been frequently performed. Lately, holmium laser enucleation of the prostate (HoLEP) with the holmium : yttrium-aluminum-garnet (Ho : YAG) laser has been performed as a minimally invasive alternative to open surgery (Gilling et al, 1998). Most recently, as urologists gain experience in minimally invasive therapy, a simple prostatectomy has been performed using a laparoscopic or robotic approach (Sotelo et al, 2005, 2008; Mariano et al, 2006). For patients with acute urinary retention, persistent or recurrent urinary tract infections, severe hemorrhage from the prostate, bladder calculi, severe symptoms unresponsive to medical therapy, and/or renal insufficiency as a result of chronic bladder outlet obstruction, transurethral resection of the prostate (TURP) or open prostatectomy is indicated. When compared with TURP, open prostatectomy offers the advantages of lower re-treatment rate and more complete removal of the prostatic adenoma under direct vision and avoids the risk of dilutional hyponatremia (the TUR syndrome) that occurs in approximately 2% of patients undergoing TURP (Mebust et al, 1989; Roos et al, 1989). Several contemporary series have demonstrated objective improvement in urinary symptoms after open prostatectomy (Tubaro et al, 2001; Gacci et al, 2003; Varkarakis et al, 2004). The disadvantages of open prostatectomy, as compared with TURP, include the need for a lower midline incision and a resultant longer hospitalization and convalescence period. There also may be an increased potential for perioperative hemorrhage (Serretta et al, 2002). Open prostatectomy can be performed by either the retropubic or the suprapubic approach. In retropubic prostatectomy the enucleation of the hyperplastic prostatic adenoma is achieved through a direct incision of the anterior prostatic capsule. This approach to open prostatectomy was popularized by Terrence Millin, who reported the results of the procedure on 20 patients in Lancet in 1945 (Millin, 1945). The advantages of this procedure over the suprapubic approach are (1) excellent anatomic exposure of the prostate, (2) direct visualization of the prostatic adenoma during enucleation to ensure complete removal, (3) precise transection of the urethra distally to preserve urinary continence, (4) clear and immediate visualization of the prostatic fossa after enucleation to control bleeding, and (5) minimal to no surgical trauma to the urinary bladder. The disadvantage of the retropubic approach, as compared with the suprapubic prostatectomy, is that direct access to the bladder is not achieved. This may be important when one considers excising a concomitant bladder diverticulum or removing bladder calculi. The suprapubic approach also may be the preferred method when the obstructive prostatic enlargement includes a large intravesical median lobe. Suprapubic prostatectomy, or transvesical prostatectomy, consists of the enucleation of the hyperplastic prostatic adenoma through an extraperitoneal incision of the lower anterior bladder wall. This approach to open prostatectomy was first performed by Eugene Fuller in New York in 1894; it was later popularized by Peter Freyer in London, England, who described the procedure in 1900 and later reported the results of his first 1000 patients in 1912 (Freyer, 1912). The major advantage of this suprapubic procedure over the retropubic approach is that it allows direct visualization of the bladder neck and bladder mucosa. As a result, this operation is ideally suited for patients with (1) a large median lobe protruding into the bladder, (2) a clinically significant bladder diverticulum, or (3) large bladder calculi. It also may be preferable for obese men, in whom it is difficult to gain direct access to the prostatic capsule and dorsal vein complex (Culp, 1975). The disadvantage, as compared with the retropubic approach, is that direct visualization of the apical prostatic adenoma is reduced. As a result, the apical enucleation is less precise and this factor may affect postoperative urinary continence. Furthermore, hemostasis may be more difficult because of inadequate visualization of the entire prostatic fossa after enucleation. Open prostatectomy should be considered when the obstructive tissue is estimated to weigh more than 75 g. If sizable bladder diverticula justify removal, suprapubic prostatectomy and diverticulectomy should be performed concurrently. If the prostatectomy is performed without the diverticulectomy, incomplete emptying of the bladder diverticulum and subsequent, persistent infection may occur. Large bladder calculi that are not amenable to easy transurethral fragmentation may also be removed during the open procedure. Open prostatectomy should also be considered when a patient presents with ankylosis of the hip or other orthopedic conditions that prevent proper positioning for TURP. Also, it may be wise to perform an open prostatectomy in men with recurrent or complex urethral conditions, such as urethral stricture or previous hypospadias repair, to avoid the urethral trauma associated with TURP. Finally, the association of an inguinal hernia with an enlarged prostate suggests an open procedure, because the hernia may be repaired via the same lower abdominal incision (Schlegel and Walsh, 1987; Brunocilla et al, 2005). In deciding whether to perform an open prostatectomy for symptomatic obstruction due to benign prostatic hyperplasia, it may be necessary to consider the upper and lower urinary tracts. Usually the patient will have already completed the International Prostate Symptom Score (IPSS) questionnaire and had a peak urinary flow rate determination. The postvoid residual urine volume also may have been verified with abdominal ultrasonography. A cystoscopic examination is not indicated in the routine evaluation of a patient with obstructive voiding symptoms (McConnell et al, 1994). However, cystoscopy should be performed in men with hematuria, suspected urethral stricture, and bladder calculus or diverticulum. It also can be helpful in confirming the presence of a large median lobe or in assessing the length of the prostatic urethra. For this indication it is most ideal to perform the cystoscopic examination with the patient under anesthesia just before surgery, when the pelvic floor musculature is relaxed. Men in urinary retention should have an evaluation of renal function. If the serum creatinine value is elevated, surgery should be delayed until this parameter stabilizes. Urinalysis is performed to rule out a urinary tract infection; and, if an infection is suspected, a urine specimen should be sent for culture and sensitivity. If an infection is present, appropriate antimicrobial therapy must be instituted before surgery to prevent urinary sepsis (Serretta et al, 2002). Historically, 3% to 10% of men undergoing an open prostatectomy will require one or more units of blood in the perioperative period (Serretta et al, 2002; Varkarakis et al, 2004; Zargooshi, 2007). Thus it may be prudent to have one or two units of blood available intraoperatively. Patients who are concerned about infectious processes associated with blood transfusion can donate one to two units of autologous blood before surgery so that it is available at the time of the procedure. The preferred autologous donation schedule is one unit per week, with the last donation 2 weeks before surgery. During this process, the patient should receive oral iron supplementation (ferrous sulfate or ferrous gluconate). The preferred anesthesia is spinal or epidural. Regional anesthesia may reduce intraoperative blood loss and the frequency of postoperative deep vein thrombosis and pulmonary embolus (Peters and Walsh, 1985). General anesthesia is utilized when there is a medical or anatomic contraindication to regional anesthesia or when the patient simply prefers general anesthesia. The suprapubic area is shaved, prepped, and draped in the usual sterile manner. A 22-Fr urethral catheter with a 30-mL balloon is passed into the bladder and connected to a sterile closed drainage system, and the balloon is inflated with 30 mL of saline. A lower midline incision from the umbilicus to the pubic symphysis is made. It is deepened through the subcutaneous tissue. The linea alba is incised, allowing the rectus abdominis muscles to be separated in the midline. The transversalis fascia is incised sharply to expose the space of Retzius. At the superior aspect of the wound the posterior rectus abdominis fascia is incised above the semicircular line to the level of the umbilicus and the peritoneum is mobilized cephalad starting at the pubic symphysis and swept anterolaterally. The pelvis is inspected for any abnormalities, and the inguinal area is examined for hernias. If a hernia is identified, it can be repaired using the preperitoneal approach described by Schlegel and Walsh (1987). A self-retaining Balfour retractor is placed in the incision and widened. A well-padded, malleable blade is connected to the retractor and used to displace the bladder posteriorly and superiorly. Unlike an anatomic radical retropubic prostatectomy, the balloon of the catheter is not positioned beneath the malleable blade. Instead it is allowed to rest at the level of the bladder neck and aids in identifying the prostatovesical junction later in the operation. The anterior surface of the bladder and prostate are exposed. With the use of DeBakey forceps and Metzenbaum scissors, the preprostatic adipose tissue is gently removed to expose the superficial branch of the dorsal vein complex and the puboprostatic ligaments (Fig. 94–1). Before proceeding with enucleation of the prostatic adenoma it is important to achieve complete control of the dorsal vein complex as well as the lateral pedicles at the bladder neck (the main arterial blood supply to the prostate gland) (Walsh and Oesterling, 1990
Indications for Open Prostatectomy
Preoperative Evaluation
Surgical Technique
Anesthesia
Retropubic Prostatectomy
Incision and Exposure of the Prostate
Hemostatic Maneuvers
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Retropubic and Suprapubic Open Prostatectomy