Resection for Hilar Cholangiocarcinoma
Yugi Nimura
 INDICATIONS/CONTRAINDICATIONS
INDICATIONS/CONTRAINDICATIONSThe indication for resection of hilar cholangiocarcinoma should be determined according to the local extension of the disease and surgical risk to the patient; the presence of distant metastases represents a clear contraindication. As local excision of the proximal bile duct can hardly contribute to radical resection of the tumor with free margins, combined liver and bile duct resection has been the standard surgical procedure for most patients with hilar cholangiocarcinoma during the last decade, and the extent of liver resection depends on the extent of the tumor along the intrahepatic sectional and/ or segmental bile ducts.
Although local invasion of the portal bifurcation, main portal vein and/or hepatic arteries had been considered as a sign of unresectable cancer, recent progress in vascular surgical techniques have enabled combined portal vein and hepatic artery resection and reconstruction for locally advanced hilar cholangiocarcinoma (see Chapter 30). Hyperbilirubinemia, cholangitis, and major hepatectomy are considered as risk factors in surgical resection of biliary cancer patients. Functional capacity of the future remnant liver is estimated by CT volumetry and liver function tests, including the indocyanine green clearance (see Chapter 18).
Distant organ metastasis and peritoneal dissemination generally contraindicate resection. However, some value of aggressive paraaortic node dissection for possible lymph node metastasis has been suggested but must be carefully estimated by prospective studies.
 PREOPERATIVE PLANNING
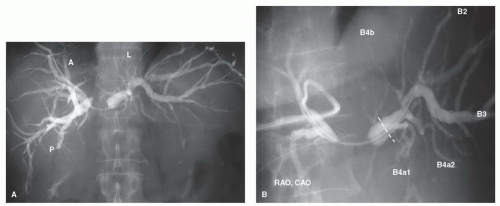
PREOPERATIVE PLANNINGAs most patients with hilar cholangiocarcinoma have obstructive jaundice at the time of diagnosis, ultrasonography followed by multidetector row-CT (MDCT) should be performed for staging of the lesion before biliary drainage. As an expected surgical procedure and future remnant liver can be designed by MDCT, unilateral biliary drainage of the future remnant liver should be carried out with endoscopic nasobiliary drainage (ENBD) or percutaneous transhepatic biliary drainage (PTBD). These external
drainage procedures have another advantage in taking selective cholangiography to make precise diagnoses of progress of cancer along the intrahepatic segmental ducts (Fig. 26.1). Percutaneous transhepatic or peroral cholangioscopy is sometimes useful to define the extension of superficially spreading cholangiocarcinoma. From these findings, resection and reconstruction of the intrahepatic sectional, segmental, and/or subsegmental ducts can be planned prior to surgery. If segmental cholangitis develops prior to surgery, urgent PTBD should be performed to drain the contralateral side of the intrahepatic duct or isolated intrahepatic segmental or subsegmental ducts.
drainage procedures have another advantage in taking selective cholangiography to make precise diagnoses of progress of cancer along the intrahepatic segmental ducts (Fig. 26.1). Percutaneous transhepatic or peroral cholangioscopy is sometimes useful to define the extension of superficially spreading cholangiocarcinoma. From these findings, resection and reconstruction of the intrahepatic sectional, segmental, and/or subsegmental ducts can be planned prior to surgery. If segmental cholangitis develops prior to surgery, urgent PTBD should be performed to drain the contralateral side of the intrahepatic duct or isolated intrahepatic segmental or subsegmental ducts.
In cases of major hepatectomy, particularly right hepatectomy, and right or left trisectionectomy, portal vein embolization (PVE) should be considered to increase the volume and functional capacity of the future remnant liver (see Chapter 18). It is important to note, however, that many patients have atrophy of the ipsilateral lobe, which results in significant hypertrophy of the future liver remnant, thereby obviating the need for PVE. Volumetric assessment is an important preoperative maneuver.
Bile replacement during external biliary drainage should be performed to restore the intestinal barrier function and prevent bacterial translocation. Also synbiotic agents should be administered pre- and postoperatively to prevent perioperative infectious complications.
 SURGICAL TECHNIQUE
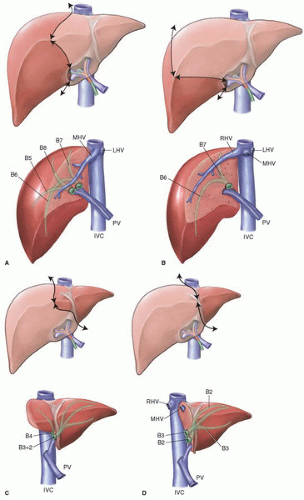
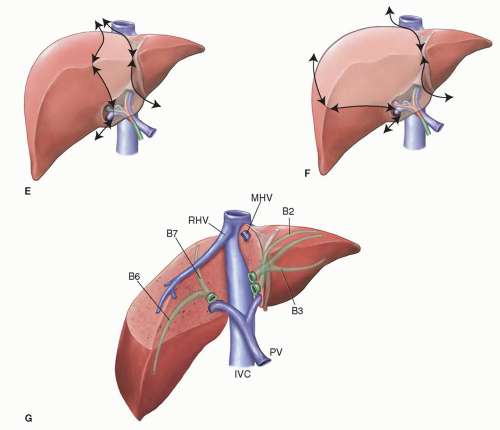
SURGICAL TECHNIQUEAs biliary branches for the caudate lobe are involved in most of the cases of hilar cholangiocarcinoma, which separate the right and left hepatic duct, the caudate lobe resection (see Chapter 22) is usually performed to establish an R0 resection, and the smallest necessary hepatic segmentectomy or sectionectomy with caudate lobectomy was designed to minimize the volume of the impaired cholestatic liver resection during 1980s. After developing preoperative PVE, hemihepatectomy, or trisectionectomy has been performed to increase the resectability of advanced carcinoma and safety of major hepatectomy (Figs. 26.2, 26.3). Advances in vascular surgical techniques in hepatobiliary surgery have allowed combined liver and portal vein and/or hepatic artery resection and reconstruction with acceptable morbidity and mortality rates for locally advanced tumors.
Skin incision
The peritoneal cavity is entered through a right or bilateral subcostal incision with an upper midline extension to widely expose the upper abdominal cavity including the whole liver using bilateral costal retractors (see Figs. 18.7, 19.3 and 21.5).
Intraoperative ultrasonography
Intraoperative ultrasonography (IOUS) is performed to assess the vascular anatomy of the liver, the extent of cancer along the intrahepatic biliary branches, to define the expected resection line of the ducts and to detect unexpected portal vein thrombosis extending beyond the portal bifurcation in case of preoperative PVE (see Chapter 18).
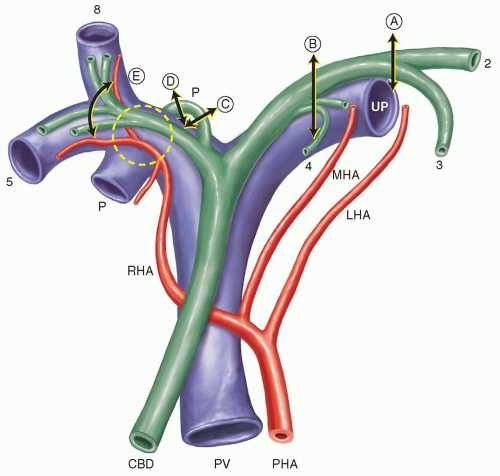
Regional connective tissue and lymph node dissection is carried out to expose and isolate the common hepatic artery (CHA), proper hepatic artery (PHA), right and/ or left hepatic artery (RHA, LHA), portal vein (PV), right portal vein (RPV) and left portal vein (LPV). The common bile duct (CBD) is exposed and divided above or in the pancreatic head with a free margin. Next, dissection of the hilar lymphatic tissue is pursued up to the hepatic hilus and the RHA or LHA is ligated and divided at its origin, and the caudate lobe branches of the portal vein are ligated and divided before dividing the RPV or LPV, resulting in a demarcation along the Cantlie line.
Mobilization of the right and left liver and the caudate lobe.
The right and/or left liver are mobilized in the usual manner, detaching the coronary and triangular ligaments (see Chapter 21, Figs. 21.6 and 21.7). In case of right-sided hepatectomy (see Chapter 19), the posterior liver is further mobilized to be detached from the inferior vena cava (IVC) by ligating and dividing all short hepatic veins (SHV) ((see Figs. 19.5, 19.6, 23.12 and 23.13)). Finally, the right hepatic vein (RHV) is clamped, divided and sutured in a traditional manner or divided with an endosurgical stapler (see Figs. 19.11, 19.12 and 23.18).
In case of the left-sided hepatectomy (see Chapter 20), the caudate lobe is mobilized from the left to the right to be detached from the IVC and all SHVs are ligated and divided, and the distal end of the Arantius canal is ligated and divided close to the left hepatic vein (LHV) or the IVC. Then the posterior surface of the caudate lobe is completely detached from the IVC (see see Chapter 22 and Figs. 22.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree