Recurrent Laparoscopic Hernia Repair
Edward L. Felix
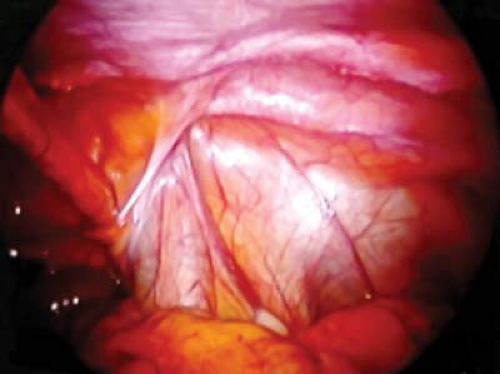
Although most surgeons agree that the laparoscopic approach is ideally suited for the repair of recurrent inguinal hernias, there still is not total agreement on what approach should be used when a laparoscopic repair fails. Whether an open or laparoscopic approach should be utilized must be dictated by the experience of the surgeon. This is because the repair of recurrent laparoscopic inguinal hernias (RLHs) is challenging and requires advanced laparoscopic skills as well as an in-depth understanding of the posterior anatomy (Figs. 21.1 and 21.2). Before undertaking the laparoscopic repair of an RLH, a surgeon must also be totally comfortable utilizing the laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair since it is the safest laparoscopic approach for recurrent laparoscopic hernias. The indications for repair are the same as for any inguinal hernia and other than a lack of experience there is no absolute contraindication to the laparoscopic repair of RLH.
Before starting a laparoscopic repair of a recurrent laparoscopic hernia it is important to know the status of the peritoneal cavity. Since the laparoscopic repair will be transperitoneal, it is essential to know if there is likely to be extensive adhesions or adhesions at the umbilical level which might jeopardize the safety of the repair. The surgeon must have a game plan before beginning the repair. This means that the surgeon must know what is going to be done if confronted by the unexpected. There must be a plan that allows the procedure to be converted to an open anterior repair if needed. Finally, the surgeon must have a plan in place for closing the peritoneum or covering the mesh repair if re-peritonealization is impossible.
Positioning
The patient’s arms are placed at the side of the patient so that the surgeon is free to stand anywhere along the side of the table. The monitor is positioned at the foot of the table and is angled so that the screen is facing the surgeon. In the TAPP repair most surgeons stand on the side of the table of their dominant hand and reach across the patient with the other hand. The assistant surgeon or scrub nurse, if acting as the assistant, stands opposite the surgeon. The scrub table is placed across the legs so that both the surgeon and nurse can reach the instruments.
Patient Prep
Although it has been shown that the routine use of a foley catheter increases the risk of retention, if the surgeon thinks that the procedure will be prolonged a catheter can be placed. Otherwise the patient must void before the induction of anesthesia. The entire abdomen should be prepped so that the position of the trocars can be varied if necessary. The groin on the side of the hernia is shaved and prepped in case the procedure must be converted to open.
Instrumentation
A straight or angled 10 mm scope can be used according to the surgeon’s preference. Instruments should be laparoscopic unipolar scissors, bipolar coagulator, atraumatic graspers, and a laparoscopic needle holder. A suction irrigator, 5 mm clip applier and tacker should be available, but do not need to be opened for every case. A 10 mm Hasson type trocar is used at the umbilicus and 5 mm trocars laterally.