and Andrea Bischoff1
(1)
Pediatric Surgery, Colorectal Center for Children Cincinnati Children’s Hospital, Cincinnati, OH, USA
Electronic supplementary material
Supplementary material is available in the online version of this chapter at 10.1007/978-3-319-14989-9_9.
9.1 Introduction
We define this malformation as a defect in a male in which the rectum is abnormally communicating with the lowest portion of the posterior urethra (Fig. 9.1). Figure 9.2 shows the characteristic image of a distal colostogram performed in a patient with this malformation.
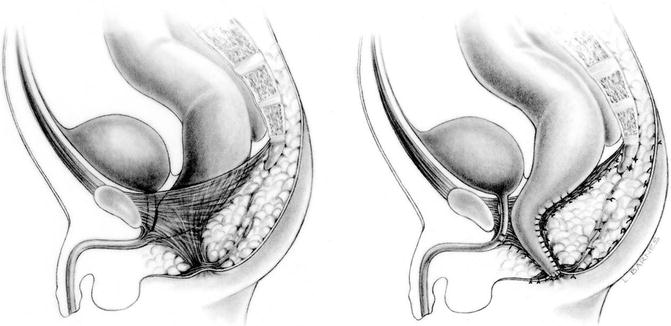

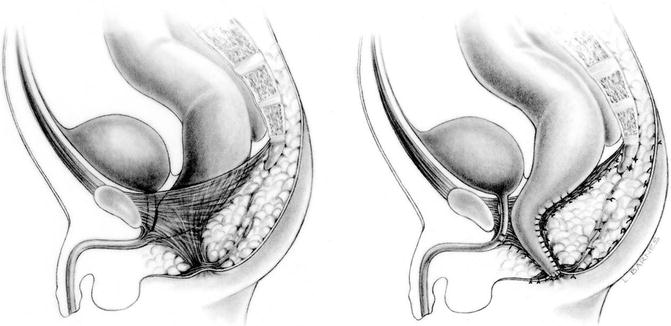
Fig. 9.1
Diagram showing a rectourethral bulbar fistula, preoperatively and postoperatively

Fig. 9.2
Distal colostogram showing a rectourethral bulbar fistula
This is the most common anorectal malformation defect in males in our series. This, of course, should not be interpreted as an accurate reflection of the incidence of this defect in the general population, since ours is a referral center, which means that in general, we tend to receive more complex defects and less of the benign and lower type of malformations.
A literature review revealed very few publications under the name of “rectourethral bulbar fistula” [1–4] in spite of the fact that it is a very common defect. The reason for this, we believe, is that most authors unfortunately are still using the terminology of “high,” “intermediate,” and “low”. Some authors consider this an “intermediate” malformation [1, 5].
Consistent with the concept that dictates that these malformations occur in a spectrum fashion, it is relatively common to see cases in which the fistula is connected even more anteriorly (penile urethra) (Fig. 9.3) [1, 2, 6]. Some authors use the term “ano-penile-urethral fistula” [6].
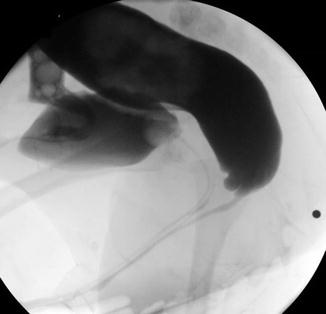
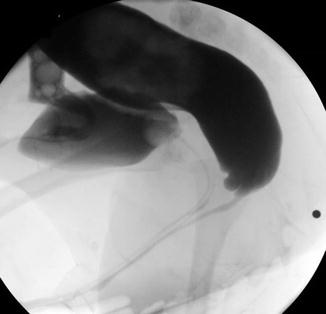
Fig. 9.3
Distal colostogram showing a fistula located at the penile urethra
Until the moment of writing this manuscript, we have had experience with the treatment of 231 cases of rectourethral bulbar fistula. Two hundred and nine of them were primary operations and 22 were reoperations.
As we have mentioned several times, every case represents an anatomic variant. Therefore, one can expect to see cases of rectourethral bulbar fistula in which the rectum opens into the urethra a little higher than the bulbar area. In other words, the rectum connects with the urethra anywhere between the prostatic urethra (middle portion of the posterior urethra) and the bulbar portion of the urethra (the lowest part of the posterior urethra).
9.2 Associated Defects
A significant number of our patients with rectourethral bulbar fistula have some sort of associated defect, mainly urologic. Hypospadias occur in 10 % of the cases, vesicoureteral reflux in about 13 % of the cases, and absent kidney in 10 % of the cases.
The sacrum, in this type of malformation, is usually normal. The average AP sacral ratio in rectourethral bulbar fistula is 0.61. The lateral one is 0.75; 2 % of the cases have sacral hemivertebrae.
Forty-six patients with this malformation were evaluated for the presence of the tethered cord; seven of them had that defect (15 %).
Spinal abnormalities, mainly hemivertebra and butterfly vertebra, have been seen in approximately 7 % of the cases with a rectourethral bulbar fistula.
Esophageal atresia occurs in 4 % of these patients; duodenal atresia in 1 %.
Patent ductus arteriosus occurs in 8 % of the cases, but only one third of them required some sort of therapeutic intervention due to hemodynamic problems. Atrial septum defects occurred in 7 % of the cases, but only one third of them required intervention. Ventricular septum defect occurred in 5 % of the cases, and ¼ of the cases required therapeutic intervention. Tetralogy of Fallot occurred in 1 % of these cases.
There is a small group of male patients born with an anorectal malformation that had communication between the rectum and the urethra in a location more anterior to the bulbar site, meaning somewhere in the spongiosum portion of the penile urethra. In those cases, the rectum follows a narrow fistula tract that runs parallel to the penile urethra and opens at different levels of the urethra (Fig. 9.3).
Those cases are not considered in the classification presented in this book, due to the fact that they are very unusual, but must be kept in mind by the surgeons.
There are also many cases of rectourethral bulbar fistula that, when seen during the newborn period, the rectal pouch seems to be bulging down and located very close to the perineal skin (Fig. 9.4). Using the traditional, old parameters to study the newborn babies, some of those cases were erroneously considered “low” malformations and consequently approached through the perineum. The surgeons found the rectal pouch, pulled it down successfully, and left the patient with a persistent, untouched rectourethral fistula. Soon enough, these patients passed urine through the rectum and stool through the urethra [7]. That is another reason why we do not favor the classification of these malformations into the traditional, old categories of “high,” “intermediate,” and “low.”


Fig. 9.4
Distal colostogram showing the rectal pouch located lower than the fistula
During the neonatal period, these babies are, in general, healthy, due to the fact that the incidence of associated defects is rather low. The perineum in these patients is usually “good looking” (Fig. 9.5), meaning that they have good midline groove and a well-defined anal dimple. Yet, there is no evidence of any kind of perineal fistula or any meconium present in the perineum. During the first 20 h of life, usually they do not pass meconium through the urine, in spite of the presence of the fistula, and we interpret that as a manifestation of a very narrow fistula tract that requires a very significant intraluminal bowel pressure in order to force the meconium through the fistula into the urethra. Therefore, one should not expect meconium in the urine in the first 20 h of life (see Chap. 4 of this book).


Fig. 9.5
Perineum of a patient with a rectourethral bulbar fistula. There is a prominent midline groove and a clear anal dimple
If the baby is born in an institution where the surgeons have a demonstrated interest and experience in the surgical management of neonatal patients, it is conceivable that these patients could be treated posterior sagittally during the newborn period without a colostomy. The fundamental requirement to perform that kind of treatment is that the surgeon could see the image of the rectum located well below the coccyx as delineated by the presence of gas. By seeing that image in a cross-table lateral film, one can be sure that by opening posterior sagittally, the rectum will be found, and therefore, one can avoid damage to the urinary tract.
Most of the patients operated on by us come to our institution with a colostomy already opened at another hospital.
If the surgeon has no experience in the management of neonates with anorectal malformations, it is much safer to open a colostomy (Chap. 5).
A laparoscopic approach is justified and convenient in cases of anorectal malformations that would require a laparotomy; yet, it has been done in these kinds of cases [8–20]. We are definitely opposed to that approach in this particular malformation. A posterior sagittal approach done in these patients is an operation that takes approximately 2 h. The rectum is minimally dissected, just enough to reach the perineum, which is very close. The abdomen is not entered; the results are very good. The patient has mild pain, can eat the same day of the operation, and can be discharged the following day. We do not understand the rationale of attempting the repair of these defects through the abdomen. A consequence of laparoscopic attempts to repair bulbar fistulas is the posterior urethral diverticula (pieces of rectum left attached to the urethra), due to the fact that the surgeon was unable to reach the end of the bowel (which resides well below the peritoneal reflection) through the abdomen, laparoscopically [21] (Animation 9.1). Also, a much more extensive circumferential dissection is done laparoscopically which is unnecessary.
9.3 Posterior Sagittal Anorectoplasty
We perform this operation as early in life as possible, since we try to avoid unpleasant memories related to the operations and rectal dilations in the patient. When the patients are born at our institution, they receive a colostomy at birth, and 2–4 weeks after that operation, assuming that the baby has recovered well, is growing, and developing normally, the baby is ready to undergo this operation. Many times, the patients are referred to us later in life, and that is why not all of our patients have been operated earlyin life.
9.4 Surgical Technique
Under good general anesthesia and endotracheal intubation, the patient is placed first in lithotomy position. We use a baby cystoscope routinely in all of our cases to confirm the diagnosis of rectourethral bulbar fistula. We take advantage of this procedure to learn more about the anatomy of the posterior urethra. We have been learning important anatomic facts from the cystoscopies in male patients with anorectal malformations, including abnormalities in the verumontanum, abnormal locations of the prostatic utricle, and ectopic ureteral openings in the bladder neck and posterior urethra. We also look at the bladder neck as well as the ureteral orifices and the bladder in general. At the end of this procedure, we pass a Foley catheter into the bladder. Sometimes the rectourethral bulbar fistula is a large one, and due to its location, the catheter tends to go into the rectum. This happens in approximately 20 % of the cases. If this happens, we can try to introduce a special catheter with a curved tip, called “coude catheter.” We must try to direct the curve of the catheter anteriorly and cephalad in order to avoid the catheter going into the rectum. This may or may not work. If it does not work, then we can take a regular Foley catheter and introduce a lacrimal probe in its tip (Fig. 9.6) (photograph). By doing that, we can direct the tip of the catheter conveniently into the posterior urethra. If this maneuver does not work, we can pass a wire through a cystoscope, followed by the catheter. Most of the time, we are successful in placing the catheter in the bladder using one of the two described maneuvers. Occasionally, it is impossible to do this and we have to leave the catheter in the rectum. During the operation, when we open the rectum, we have the opportunity to redirect the catheter toward the bladder under direct vision.
Fig. 9.6
Lacrimal probe introduced in the tip of a Foley catheter in order to direct it into the bladder and avoid getting through the fistula into the rectum
With the Foley catheter in place, the patient is placed in prone position with the pelvis elevated. The positioning of the patient is the responsibility of the surgeon. One must be absolutely sure that all of the pressure areas are well cushioned to avoid any potential injuries. The chest should be slightly elevated from the table, with rubber foam (Fig. 9.7) to be sure that the shoulders fall forward to avoid stretching of the brachial plexus. The tips of the toes should not rest on the table. The penis should be free from the rubber foam that is placed in the groin to elevate the pelvis.


Fig. 9.7
Prone position with adequate cushioning
The perineum and perineal area are washed, prepped, and draped in the usual manner. The sterile towels are sutured to the skin to avoid their displacement during the operation (Fig. 9.8). Because of the position of the patient, the towels that surround the operative field tend to fall away, even if taped, and therefore, we have learned to stitch them to the skin.


Fig. 9.8
Sterile towels sutured to the skin to avoid contamination
Animations 9.2 and 9.3 illustrate the basic principles and technical maneuvers required to repair this malformation.
An electrical stimulator is used to determine the limits of the sphincter and also as a guide to be sure that we make the incision dividing the sphincter exactly in the midline, leaving equal amounts of muscle on both sides. A special very fine needle-tip cautery is used to avoid excessive tissue burning. A very sharp needle allows the surgeon to decrease the intensity of the electric current used during the operation by concentrating the energy in the tip of the needle. Not being familiar with the use of this specific type of needle may provoke serious tissue burning. The needle must be used with quick movements touching the tissues only with the very tip of the needle and not with the lateral parts. The field should always be dry, as wetness will diffuse the energy, making the needle ineffective, which may induce the surgeon to increase the intensity, producing tissue burning.
The skin is opened with an incision running from the inferior portion of the sacrum to the anal dimple. When we open the skin, we continue opening the subcutaneous tissue and we usually find a group of fibers that run parallel to the skin and on each side of the midline; therefore, we call them parasagittal fibers (Fig. 9.9). These fibers are divided exactly in the midline. We try to separate rather than to cut them. A Weitlaner retractor is used, trying to place the retractor as superficially as possible to not injure the muscle fibers. Below the parasagittal fibers, we find a fatty tissue that we call ischiorectal fossa (Fig. 9.10). There, it is rather difficult to maintain the midline plane. There is a very thin fascia that can be identified by careful observation of the tissues; that thin fascia allows us to separate one side of the ischiorectal fossa from the other and to avoid the inconvenient herniation of fat into the operative field that may interfere with the exposure. Below the ischiorectal fossa, we find the levator muscle (Fig. 9.11). The levator muscle is divided in the exact midline with needle-tip cautery (Fig. 9.12).

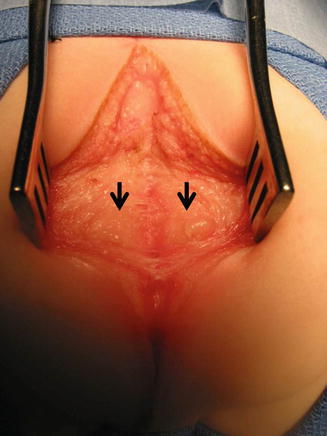
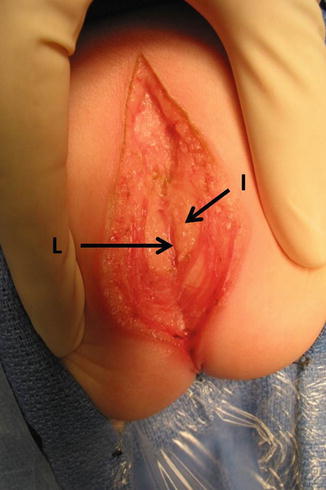
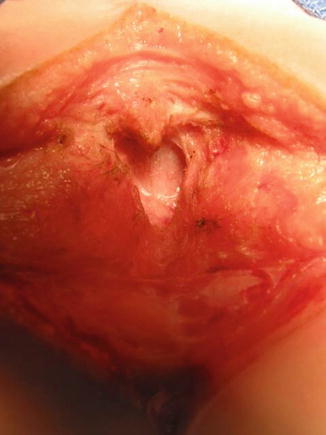

Fig. 9.9
Parasagittal muscle fibers on both sides of the wound
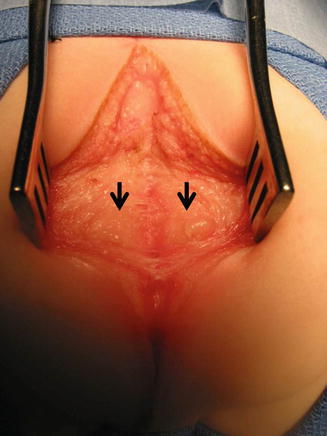
Fig. 9.10
Ischiorectal fossa located deeper than the parasagittal fibers. Arrows – ischiorectal fossa
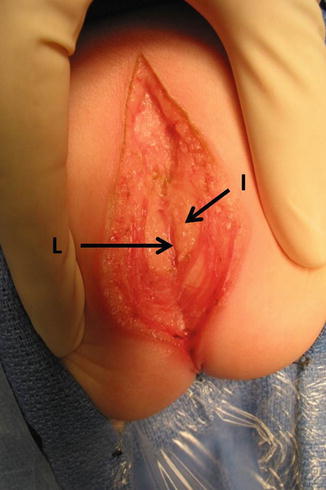
Fig. 9.11
Levator muscles, found deeper than the ischiorectal fossa. L levator, I ischiorectal fossa
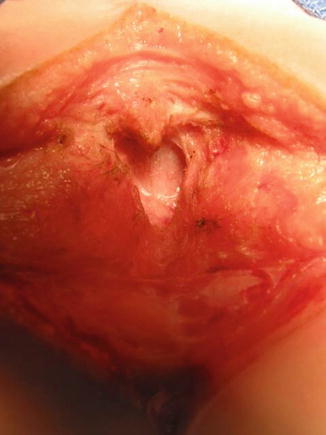
Fig. 9.12
The levator muscle is divided in the midline
In the area of the anal dimple, we find another group of fibers that run perpendicular to the parasagittal fibers, from the skin toward the urethra. These we call the muscle complex (Fig. 9.13). The muscle complex joins in continuity with the levator muscle, forming an angle usually of about 90° (Fig. 9.14). The muscle complex fibers must also be divided exactly in the midline. After we divide the entire sphincter mechanism, deeper, we identify a characteristic white fascia that covers the rectum posteriorly (Fig. 9.15). The white fascia is divided to create a plane of dissection as close as possible to the rectal wall. The dissection of the rectum must be performed by staying in intimate contact with the rectal wall itself.
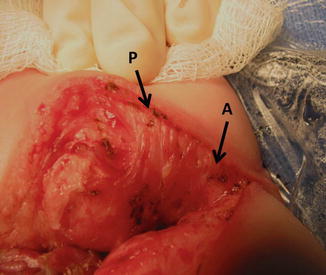
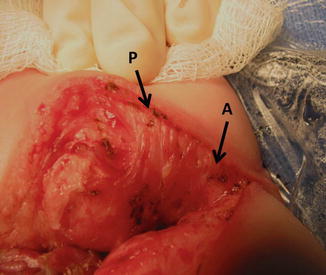
Fig. 9.13




Muscle complex. (a) Anterior limit of the sphincter. (b) Posterior limit of the sphincter
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








