and Andrea Bischoff1
(1)
Pediatric Surgery, Colorectal Center for Children Cincinnati Children’s Hospital, Cincinnati, OH, USA
4.1 Introduction
In dealing with most congenital anomalies, errors that occur during the first few hours or days of life may have serious consequences and sequelae. Early accurate diagnoses, as well as adequate therapeutic decisions, require a high index of suspicion from pediatricians, neonatologists, pediatric surgeons, pediatric urologists, nurses, and other physicians and surgeons who take care of neonatal babies with congenital anomalies.
Our eyes only see what our mind suspects.
It is hard to believe that in this twenty-first century in developed countries, we still hear of patients born with imperforate anus that were sent home as “normal babies.” Subsequently, it was the mother who made the diagnosis or the babies suffer from bowel perforation and some of them die [1–9]. We cannot overemphasize the importance of the anorectal examination during the first physical examination of a neonate. In addition, it is also true what is written in the very old textbooks of pediatric surgery; it is not enough by looking at the external appearance of the anus, but it is rather necessary to introduce a little catheter or thermometer to be sure that the anus is patent. There is one specific type of defect in which the babies have a normal-looking anus externally, a normal anal canal, approximately 1–2 cm deep, and then an atresia. That type of defect is the one that can only be diagnosed by trying to pass a thermometer, catheter, or an instrument through the anus. That particular malformation only occurs in 1 % of all patients born with anorectal malformations [10].
4.2 Most Common Scenario
As pediatric surgeons, we are called to see a baby that is just born and has no anus. There are two very important questions to be answered.
1.
Does the baby have a serious associated defect that may kill him/her within the next few hours or days of life?
2.
Does the baby need some sort of primary anal repair or a colostomy?
These questions should be answered in the same order that they are presented here. In other words, the surgeon must refrain from jumping into trying to find the answer of the second question but rather concentrate during the first 24 h of life in trying to answer the first question.
4.3 Answering the Two Most Important Questions
At this point, the neonatologist and the surgeon should remember that about 30 % of all babies with anorectal malformation have some sort of cardiovascular condition [11]. However, only one third of that 30 % have serious hemodynamic repercussions that mandate to implement some sort of medical or surgical treatment [11]. The most common cardiac congenital anomalies seen in these cases are patent ductus arteriosus, atrial septal defect, ventricular septal defect, and tetralogy of Fallot, and then other more serious conditions are more rarely seen. The presence of cyanosis or respiratory distress should alert the clinician to investigate for the presence of these conditions. At the present time, most neonatal centers have a pediatric cardiologist and an echocardiogram machine which allows ruling out most of these conditions.
Eight percent of babies with anorectal malformations are born with esophageal atresia [12]. Part of the physical examination of the neonate includes the passing of a nasogastric no. 8 feeding tube through the nostril to confirm that the esophagus is patent. When the clinician feels resistance in the passing of the tube about 8–10 cm from the nostril, it is possible that the baby has an esophageal atresia (Fig. 4.1). In addition, babies with esophageal atresia cannot swallow their saliva; this represents a risk of aspiration. The saliva accumulates in their mouth as foam.
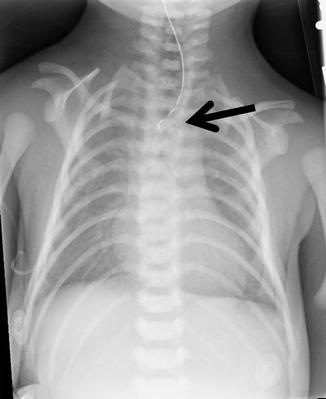
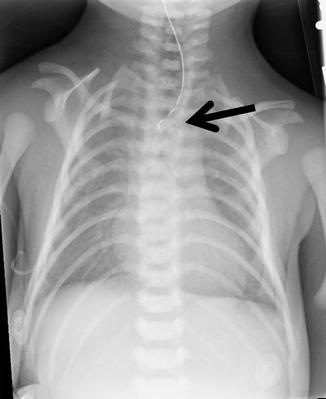
Fig. 4.1
Radiologic image of a baby with esophageal atresia. Arrow shows the blind end of the esophagus
Approximately 3 % of babies with anorectal malformations suffer from duodenal atresia [12]. A simple abdominal film shows a classic “double bubble” image (Fig. 4.2). The “double bubble” represents the stomach and the duodenum full of gas: in addition, there is a conspicuous absence of gas in the rest of the abdomen. Approximately 50 % of all patients with anorectal malformations are born with an associated urologic condition [13]. The most serious of these are hydronephrosis, vesicoureteral reflux, absent kidney, and megaureters. One specific group of patients has a very high risk of having kidney damage; those are patients born with a single kidney, hydronephrosis, vesicoureteral reflux, and megaureter. In those cases, we must remember that the single kidney has been suffering in utero, and therefore, we must expect a serious functional limitation. Every effort should be done to protect the damaged kidney. For this, it is mandatory to do a kidney and bladder ultrasound in all babies with anorectal malformation. If the ultrasound shows abnormalities such as hydronephrosis, then the baby will need a full urologic evaluation including, of course, a voiding cystourethrogram. If the kidney ultrasound is normal and the patient is passing urine without difficulty, we must assume that most likely his urinary tract is otherwise healthy.


Fig. 4.2
Characteristic radiologic image known as “double bubble” in a baby with duodenal atresia
Taking a baby to the operating room to repair an anorectal malformation or to open a colostomy only to find that the baby gets very sick during the operation because he has a serious cardiac, esophageal, or kidney problem is an undesirable and preventable experience.
All babies with anorectal malformations must have an abdominal x-ray film that shows the degree of bowel dilatation, the characteristics of the spine, and the characteristics of the sacrum. The presence of intraluminal calcifications in the rectosigmoid most likely is due to the passing of urine to the bowel. Urine mixed with meconium may produce calcifications [14, 15]. The sacral films must include AP and lateral views (Figs. 4.3 and 4.4). The characteristics of the sacrum are extremely important in order to determine the future functional prognosis for bowel control, urinary control, and sexual function. Traditionally, we evaluated the sacrum by counting the number of vertebrae. We found this to be a rather limited nonuseful way, and therefore, we created what we call the sacral ratio (Figs. 4.5 and 4.6) (see Chap. 6).
Fig. 4.3
X-ray films of a normal sacrum in a baby with an anorectal malformation. (a) AP view. (b) Lateral view
Fig. 4.4
X-ray films of an abnormal sacrum in a baby with an anorectal malformation. (a) AP view. (b) Lateral view
Fig. 4.5
Normal sacral ratio. (a) Diagram. (b) Radiograph
Fig. 4.6
Abnormal sacral ratio. (a) AP view. (b) Lateral view
Taking x-ray films of the sacrum is mandatory also because we must rule out the presence of a hemisacrum, which means that the patient has a presacral mass; this finding has important therapeutic and prognostic implications.
An ultrasound of the lower sacrolumbar spine is extremely useful and must be done during the first hours of life to determine whether or not the baby has tethered cord (Fig. 4.7). This is also important to determine the functional prognosis for bowel and urinary control.
Fig. 4.7
Spinal ultrasound of a newborn baby. (a) Normal. (b) Tethered cord
All these studies can be done during the first 24 h of life. Babies with anorectal malformations are usually not born with a distended abdomen. It takes a few hours for the abdomen to start becoming distended. It is after 24 h of life that the abdominal distention becomes critical, and a management decision must be taken.
4.4 Physical Examination
4.4.1 Male Patients
During our first contact with the baby with anorectal malformation, we should dedicate a special time for a meticulous detailed examination of the baby’s perineum. Babies with anorectal malformations have different external appearances of their perineum, and they have very important clinical significance.
The presence of a flat bottom, meaning absence of the normal midline groove that all human beings have between both buttocks, is usually associated with malformations with bad prognosis and very highly located rectum (Fig. 4.8). In addition, most patients with anorectal malformations have an anal dimple that represents the point in the perineum where the patients have the largest concentration of sphincter fibers (Fig. 4.9). The more prominent the anal dimple, the better the quality of the sphincter and therefore the prognosis. The absence of an anal dimple is a very bad sign, usually present in poor prognosis type of defects. The location of the anal dimple varies from patient to patient. The closer the anal dimple to the scrotum, the worse the prognosis (Fig. 4.10). The longer the distance between the tip of the coccyx and the anal dimple, the poorer the prognosis, either because the anal dimple is located too anteriorly or because the sacrum is very short or both. We call it a “good-looking perineum” when the baby has a well-formed midline groove and a well-located anal dimple (Fig. 4.9a). Even by touching that area, one can see the contraction of the sphincter of the anal dimple.



Fig. 4.8
“Flat bottom” in a baby with a recto-bladder neck fistula
Fig. 4.9
Photograph of the perineum of a newborn baby with (a) good anal dimple. (b) Absent anal dimple. Arrow shows the anal dimple

Fig. 4.10
Location of the anal dimple. (a) Normal distance between the scrotum and the anal dimple (malformation with good functional prognosis). (b) Anal dimple next to the scrotum (malformation with less than optimal functional prognosis). Arrow shows the anal dimple
The most “benign” of all anorectal malformations is called “perineal fistula.” The rectum opens into the perineum, anterior to the sphincter in a rather narrow orifice. This malformation is also known as a “low defect.”
A perineal fistula in a male patient may have different external manifestations. A common one is the presence of a malformation called “bucket handle” (Fig. 4.11) which is a prominent skin band under which we can pass a mosquito clamp. Another external manifestation of a perineal fistula can be a subepithelial fistula (Fig. 4.12). The fistula tract may be full of meconium, giving the appearance of a “black ribbon.” Other times, it may be full of white mucous material (Fig. 4.13). The black or white subepithelial tract may extend toward the scrotum in the midline or even to the base of the penis.




Fig. 4.11
“Buckle handle” malformation in a baby with a perineal fistula

Fig. 4.12
“Black ribbon” appearance of a subepithelial fistula, external manifestation of a perineal fistula

Fig. 4.13
“White ribbon” appearance of a subepithelial fistula, external manifestation of a perineal fistula
A perineal fistula can be repaired with an anoplasty during the neonatal period without a colostomy and has an excellent functional prognosis. The exception would be the group of patients with perineal fistulas associated to an abnormal sacrum and a presacral mass. Ironically, the presence of a presacral mass and hemisacrum seems to be more frequently associated to perineal fistulas than to other anorectal defects.
Occasionally, one may see a patient with a subepithelial fistula or a “bucket handle” malformation; we try to repair the defect only to find that the patient has actually a very long narrow fistula and the rectal pouch is located high in the pelvis. That is a real exceptional situation (Fig. 4.14). Under those circumstances, the surgeon has to decide to continue the operation to mobilize the rectum down or to abort the procedure and open a colostomy. That would depend on the degree of experience of the operator.
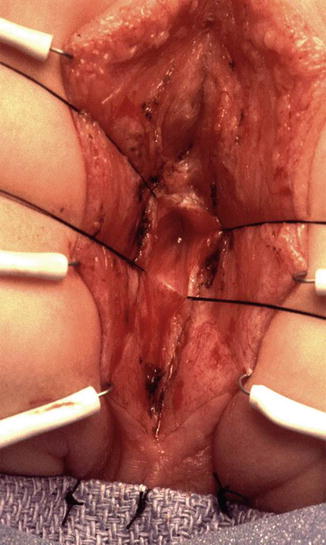
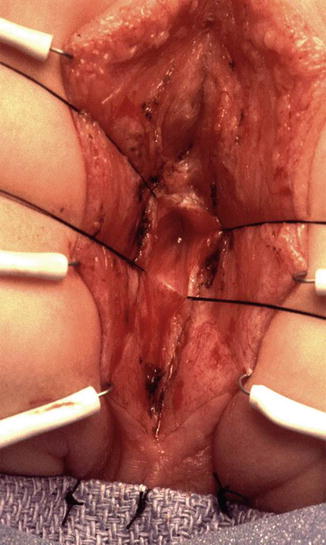
Fig. 4.14
Intraoperative aspect of a long narrow perineal fistula communicating with a very high rectum
The presence of bifid scrotum (Fig. 4.15) is usually associated to a rather complex defect; most likely the rectum is located high in the pelvis, connecting to the urinary tract very high (bladder neck or prostatic fistula), although there are exceptions. The bifid scrotum is something that we usually repair at the same time that we repair the anorectal malformation (see Chap. 23, Sect. 23.5).


Fig. 4.15
Bifid scrotum, a defect frequently associated to a highly located rectum
4.5 Female Babies
In female patients, the surgeon must be particularly careful in the examination of the baby’s perineum and genitalia. One should put the baby in a convenient lithotomy position with somebody holding the baby’s legs. We should have good illumination and magnifying glasses if necessary and take the time to clean the genitalia and to separate the labia to see if there is meconium and precisely where it comes from. Some fistulas are very narrow, and it takes several hours, sometimes up to 24 h, for the babies to pass meconium. The most common defect seen in babies is a malformation called vestibular fistula. As we separate the labia, we can see the urethral opening, the hymen, and the vaginal orifice, and immediately behind that, but still within the introitus of the baby, one can see another little orifice that we call vestibular fistula (Fig. 4.16).