Fig. 45.1
(a) A primary T3N0M0 rectal cancer treated with a lower anterior resection without adjuvant therapy. The anterior recurrent tumor fixed at the base of the bladder was treated with preoperative chemoradiation and then resected with IORT. (b) After a primary low anterior resection for T2N0M0 rectal cancer without adjuvant therapy, this patient developed a lateral pelvic recurrence. After preoperative chemoradiation, the patient underwent an abdominal resection with negative margins. (c) A recurrence after a T3N0M0 lesion treated with postoperative chemoradiation therapy was found to invade the sacrum. After additional EBRT and chemotherapy, IORT combined with an en bloc resection of the tumor and distal sacrum was performed with negative margins. (d) A massive recurrent cancer found in the pelvis after an abdominal perineal resection and postoperative chemoradiation. The tumor was fixed to vital pelvic structures and was deemed unresectable (With permission from Nicholls RJ, Dozois RR, editors. Surgery of the colon and rectum. New York: Churchill Livingston; 1997)

Fig. 45.2
The IORT suite, showing the equipment, the position of the patient on the operating room table, and the linear accelerator

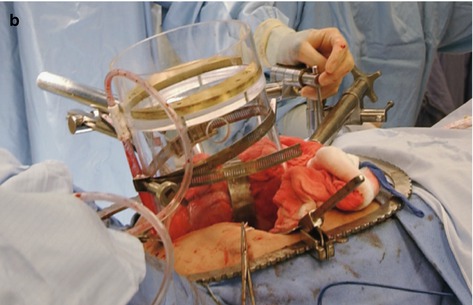
Fig. 45.3
(a) The assortment of the Lucite tubes used to direct the electron beam to a fixed site in the operating field to deliver the IOT. (b) Place of a large Lucite tube to deliver the IORT into the pelvis. The tube is fixed in place by securing it to an external support apparatus attached to the operating table
Although we have found this classification scheme to be extremely useful, it does not reliably predict resectability before surgery because new findings may be discovered at operation.
However, in our experience, some factors are clearly associated with an unresectable tumor (Table 45.1).
Table 45.1
Symptoms or findings suggestive of an unresectable tumor for cure
Sciatic pain |
Bilateral ureteral obstruction |
Multiple points of tumor fixation to the pelvic sidewall |
Circumferential involvement of the pelvic sidewall |
S1 or S2 bony or neural involvement |
Extrapelvic disease |
Any circumferential tumor that extends to the pelvic sidewall is considered unresectable.
Evidence of bilateral ureteral obstruction is a very worrisome finding. Unless there is focal infiltration of the bladder trigone causing bilateral ureteral obstruction, this finding usually indicates that a bulky tumor has invaded both lateral pelvic sidewalls.
Finally, S1 and S2 nerve root involvement or evidence of invasion of the sacral bone at the level of S1 and S2 indicates an unresectable tumor.
Pain from nerve root involvement with tumor occasionally needs to be differentiated from sciatic nerve compression. Nerve compression symptoms may completely resolve after pelvic irradiation and chemotherapy. On the other hand, persistent buttock and perineal pain usually resulting from tumor expansion and ingrowth is a more ominous symptom.
Multimodality Therapy for Advanced or Locally Recurrent Rectal Cancer
Surgery with curative intent is the mainstay of treatment for advanced or locally recurrent rectal cancer. However, surgery alone results in a high rate of local and distant failure.
To improve outcomes, surgery is combined with multimodality therapy, radiation, and chemotherapy. Radiotherapy is used to improve local control and systemic chemotherapy is used to treat possible disseminated disease.
In the setting of a locally advanced or recurrent rectal cancer, centers have combined multimodality therapy with intraoperative radiotherapy – either as electron-beam radiation therapy, high-dose rate brachytherapy, or traditional perioperative brachytherapy to further improve patient outcomes.
These forms of locally directed radiation reduce toxicity by limiting normal tissue exposure and deliver a high biologically equivalent dose to the localized area of the tumor.
In general, patients who never received prior pelvic radiation therapy, a full course of external-beam radiation (5,040 cGy) is administered with concurrent 5-fluorouracil chemotherapy.
Often, patients with recurrent rectal cancer have previously received a full course of pelvic external-beam radiation.
Such patients can be treated with an additional course of 2,000 cGy of external-beam radiation combined with additional 5-fluorouracil chemotherapy before repeating pelvic surgery.
A recent multicenter study has shown that hyperfractionated preoperative chemoradiation can be safely administered in recurrent rectal cancer patients who have previously received pelvic radiation. The overall tumor response rate was 44.1 %. Furthermore, there was no increase in postoperative complications as compared to patients who did not receive the hyperfractionated therapy.
Surgery
Before surgery, the magnitude of the operation and the possible complications are discussed in depth with the patient and family members.
In cases of large locally advanced primary rectal cancers, the sphincter mechanism is preserved. In recurrent cancers, there is little role for an attempt at sphincter preservation, as the risk of complications or poor functional outcomes is quite high.
In addition, the resection of adjacent structures or organs and the functional implications and reconstruction alternatives, such as an ileal conduit, need to be discussed. All patients visit with and are marked for multiple ostomies by an enterostomal therapist.
In the OR, the patient is placed in the lithotomy position with both arms tucked and the legs supported in Allen stirrups. Special care is taken to ensure that the arms are well padded and in a neutral position to avoid any nerve injury. The calves are positioned and padded to avoid any pressure from directly resting on the stirrups, since the lengthy operation may result in compartment syndrome and/or venous thrombosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






