Fig. 31.1
(a) Preoperative KUB demonstrated a 6 × 8 mm lower pole renal stone. (b) Postoperative KUB demonstrated no residual stone in kidney

Fig. 31.2
Postoperative KUB demonstrates a ureteral stent in good position with a large steinstrasse. Patient underwent successful ureteroscopic stone removal
Ultrasound can be helpful to diagnose the presence of hydronephrosis which may be indicative of ureteral obstruction. While ultrasound is accurate in diagnosing hydronephrosis it is less accurate in determining residual stone burden [4]. The main goal, therefore in using ultrasound, is to determine the presence of hydronephrosis. Using ultrasound in conjunction with a KUB is reasonable; however, the vast majority of patients with obstruction are usually symptomatic. In symptomatic patients an ultrasound would be warranted. A bedside or office ultrasound may be extremely helpful in this clinical scenario (Fig. 31.3). If patients are found to have hydronephrosis, either a CTU, IVP, or cystoscopy with retrograde pyelography may be indicated to further delineate the etiology of the hydronephrosis. The AUA guidelines panel reported an overall incidence of ureteral stricture following ureteroscopy at approximately 1% [14]. The need to search for silent hydronephrosis as a result of ureteral stricture by adding ultrasound to a KUB exam is probably superfluous.
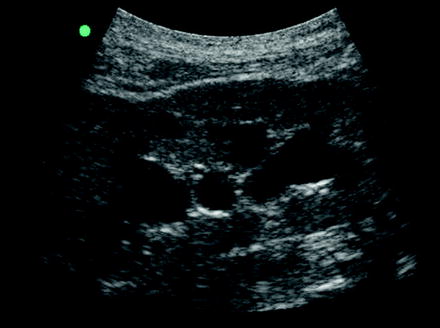
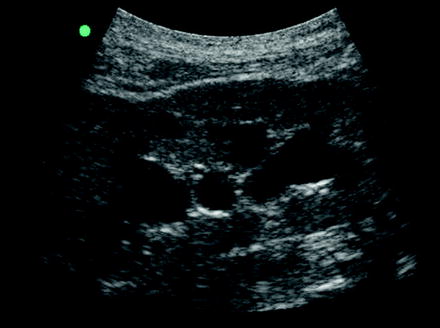
Fig. 31.3
Patient presented with postoperative pain 3 days following teroscopic laser lithotripsy. Bedside ultrasound demonstrated moderate hydronephrosis. KUB demonstrated a 2 mm distal ureteral fragment at the ureterovesical junction. Patient successfully passed the fragment with medical expulsive therapy and follow-up ultrasound revealed resolution of the hydronephrosis
NCCT is probably indicated in patients with non-radiopaque stones (uric acid, cystine). Judicious use of NCCT is warranted given the theoretical radiation exposure risk from repeated exams, especially in the pediatric and young adult population [15–17].
Patients who undergo balloon dilation of the ureteral orifice have no greater incidence of postoperative stricture than those who do not undergo balloon dilation [18]. In patients with an atraumatic balloon dilation of the ureteral orifice, no follow-up imaging is required specifically as a result of the balloon dilation.
The use of ureteral sheaths is now a common ancillary procedure used in conjunction with ureteroscopic stone management. Ureteral sheaths facilitate treatment of large stones, provide easy multiple access to the kidney, and decreases intra-operative intrarenal pressure during treatment. In routine cases where a ureteral sheath was used, a follow-up renal ultrasound for detection of hydronephrosis is not indicated. In instances where ureteral splitting of the urothelial lining was noted, a routine follow-up ultrasound 4–6 weeks post-procedure is recommended to rule out silent obstruction in the asymptomatic patient and earlier if patient develops symptoms consistent with ureteral obstruction [19].
Follow-Up Imaging After Complicated Ureteroscopy
Complicated ureteroscopy could be defined as performing a ureteroscopy on a patient with preexisting conditions such as renal insufficiency or a preexisting ureteral stricture, a known impacted stone, intraoperative traumatic balloon dilation, ureteral perforation, or the presence of an impacted stone found at the time of ureteroscopy. In these instances postoperative imaging is definitely warranted. As in uncomplicated ureteroscopy, a KUB at the time of follow-up is helpful to ascertain stent position (usually placed in all of the scenarios listed above for variable time lengths) as well as for residual stone burden. After the stent is removed, an anatomic study such as a renal ultrasound or NCCT is reasonable to obtain at 1–3 months post-stent removal, provided the patient was rendered stone-free initially. These studies can be done earlier if the patient is symptomatic (pain, fever, serum creatinine elevation). Functional studies such as a CTU, IVP, or nuclear renal scan can also be helpful in following patients after a complicated ureteroscopy (Figs. 31.4 and 31.5). In cases of newly diagnosed stricture, worsening hydronephrosis of a preexisting stricture, or symptomatic ureteral stricture, a cystoscopy and retrograde pyelogram is certainly indicated. A cystoscopy and retrograde pyelogram provides a means to ascertain the location, degree, and length of the stricture (Fig. 31.6). It also provides concomitant treatment options which could be definitive ureteroscopic treatment or temporary relief with placement of a ureteral stent.
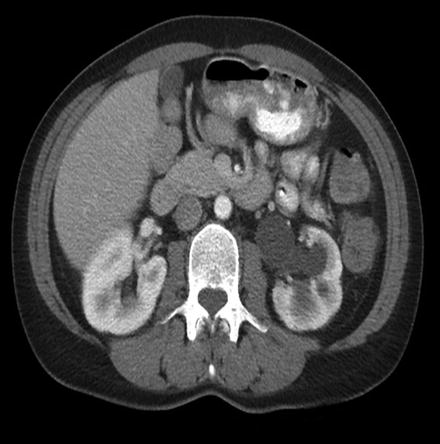


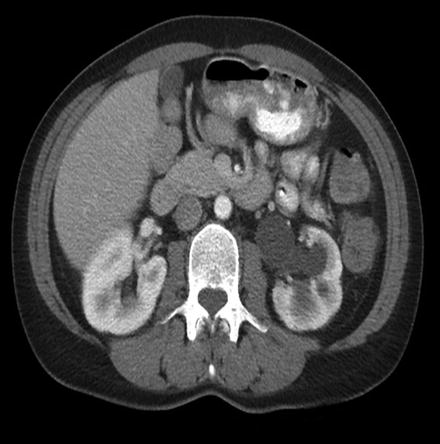
Fig. 31.4
Follow-up NCCT following treatment of a large severely impacted proximal ureteral stone. NCCT demonstrated moderate to severe hydronephrosis despite patient having minimal symptoms

Fig. 31.5
Retrograde pyelography of above patient demonstrated a long proximal ureteral stricture. Patient underwent a difficult but successful open flap pyeloplasty

Fig. 31.6
Patient was referred for further management of a complicated proximal ureteral stricture after an ureteroscopic laser lithotripsy which was complicated by a significant perforation at the site of the stone. Patient underwent successful ureterocalycostomy
Impacted stone or known stricture: In cases of patients with a known ureteral stricture, or with a severely impacted stone who had a perforation at the time of ureteroscopic stone treatment, serial functional exams may be warranted (Fig. 31.7). A 24% stricture rate has been reported in patients who underwent ureteroscopic stone treatment for an impacted stone complicated by ureteral perforation at the site of impaction [20].
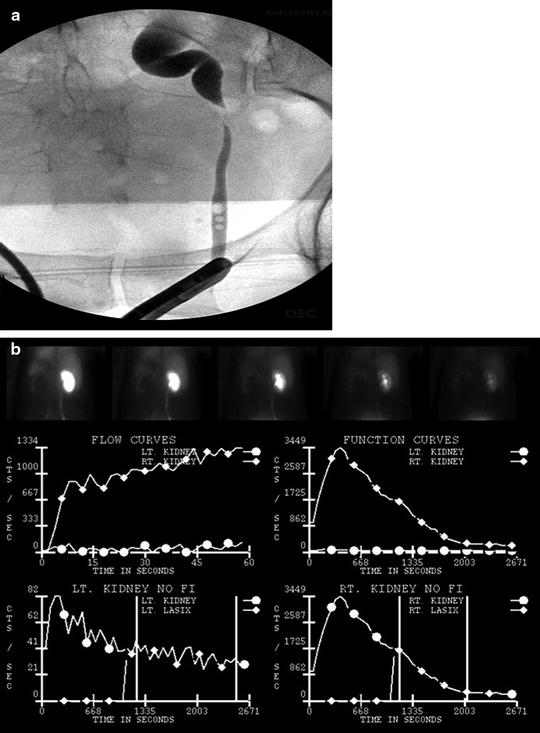
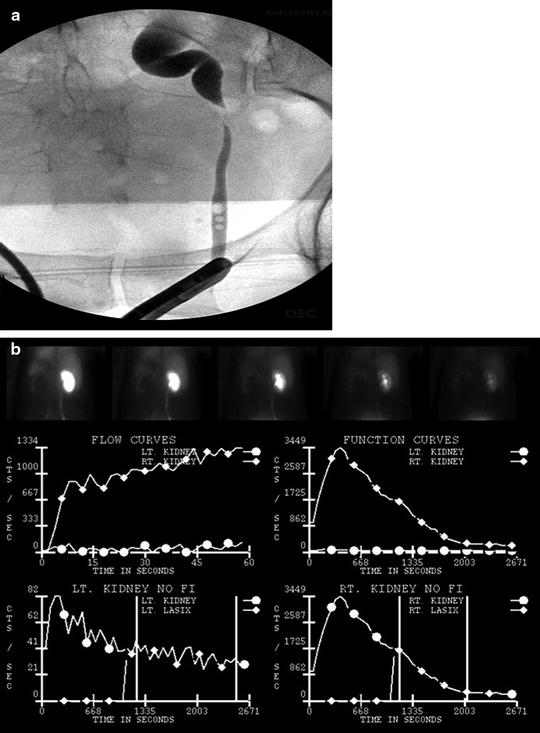
Fig. 31.7




Patient had ureteral perforation at the level of the iliac vessels while performing semirigid ureteroscopy. (a) Follow up cystoscopy and retrograde pyelogram demonstrated a severe stricture. (b) Renal scan demonstrated differential function of 4% on the affected side. Patient subsequently underwent laparoscopic nephrectomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







