Chapter 13 Portal Hypertensive Bleeding
Introduction
Portal hypertension is a clinical syndrome defined as an increase in portal venous pressure greater than 5 mm Hg.1,2 It can arise from any condition interfering with the blood flow within the portal system. Among several complications of portal hypertension, including ascites, hepatic encephalopathy, and renal insufficiency, variceal hemorrhage is the most dramatic with a high mortality. Under physiologic conditions, collaterals exist between the portal venous system and the systemic venous circulation; in portal hypertension, these collaterals enlarge in an attempt to decompress the portal circulation and form varices. This chapter focuses on the gastrointestinal (GI) bleeding that results from portal hypertension; other complications of portal hypertension are reviewed separately.
Etiopathogenesis
The portal vein supplies about 1050 mL of blood into the liver sinusoids every minute. An additional 300 mL of blood is supplied by the hepatic artery with the total averaging around 1350 mL/min, which amounts to about 27% of the cardiac output. The liver receives fresh oxygenated blood from the hepatic artery and nutrient-rich blood from the stomach, spleen, and small and large intestine via the portal vein. Measuring approximately 8 cm in length, the portal vein is formed by the union of the superior mesenteric vein and splenic vein behind the neck of the pancreas. Immediately before reaching the liver, the portal vein divides into right and left branches. The right branch receives the cystic vein and enters the right lobe of the liver. The left branch receives the umbilical and paraumbilical veins, which can dilate to form caput medusae in cirrhosis. Blood from the hepatic artery and blood from the portal vein mix for the first time in the hepatic sinusoids. After mixing, the blood is drained from the lobule by the central vein, a branch of the hepatic vein. With this understanding, the portal system can be divided anatomically into presinusoidal, sinusoidal, and postsinusoidal. Portal hypertension can arise from any condition interfering with blood flow at any level within the portal venous system (Table 13.1).
Table 13.1 Common Causes of Portal Hypertension
| Prehepatic | Hepatic | Posthepatic |
|---|---|---|
| Portal vein thrombosis | Presinusoidal | Inferior vena cava obstruction |
| NCPF | ||
| IPH | ||
| Sarcoidosis | ||
| Schistosomiasis | ||
| Nodular regenerative hyperplasia | ||
| Myeloproliferative disorders | ||
| Splenic vein thrombosis | Sinusoidal | Cardiac failure |
| Cirrhosis | ||
| Hepatoportal arteriovenous fistula | Postsinusoidal | Constrictive pericarditis |
| Budd-Chiari syndrome | ||
| Venoocclusive disease | ||
| Splenomegaly | ||
IPH, Idiopathic portal hypertension; NCPF, noncirrhotic portal fibrosis.
Cirrhosis is the most common cause of portal hypertension in the Western world,3,4 accounting for about 90% of cases; schistosomiasis is the leading cause in many developing countries. Other causes of portal hypertension include portal vein thrombosis, polycystic liver disease, nodular regenerative hyperplasia of the liver, congenital hepatic fibrosis, myeloproliferative disorders, hepatic sarcoidosis, and hereditary hemorrhagic telangiectasia. The primary factors influencing increased pressure in the portal hepatic system are resistance and flow. In cirrhosis, both resistance and flow are altered. Increased portal venous resistance is central to the development of portal hypertension in cirrhosis. This increased resistance can be attributed to two specific factors. The first is mechanical obstruction to flow secondary to fibrotic disruption of the liver architecture and regenerative nodules. The second factor is a dynamic component produced by active contraction of vascular smooth muscles and activated stellate cells, believed to be due to a relative deficiency of nitric oxide (vasodilator),5,6 and high levels of endothelin-1 (vasoconstrictor) leading to increased sinusoidal resistance.7–9 Also, cirrhosis results in a hyperdynamic circulatory state that is characterized by peripheral and splanchnic vasodilation, reduced mean arterial pressure, and increased cardiac output. Nitric oxide–mediated splanchnic vasodilation8–16 produces an increase in inflow of systemic blood into the portal circulation, which causes an increase in portal pressure.10,11
The correlation between collateral blood flow and the transmural pressure gradient in the varix is expressed as: P1 − P2 = Q × R, where P1 and P2 are the pressures within and outside the varix, Q is the blood flow per unit of time, and R is the resistance to flow through the varix. Poiseuille’s formula states that the resistance to flow may be expressed as follows: R = 8 nl/p r4, where n is blood viscosity, l is length, and r is radius of the vessel. The transmural pressure and radius of the varix along with the mural thickness of the varix (w) determines the wall tension of the varix according to the law of Laplace: Wall tension = Q × (8 nl/p r4) × r/w. The propensity for a varix to bleed is directly linked to its wall tension. Theoretically, large long varices with thin walls and high rates of flow are most prone to bleed. Decreasing collateral flow (by decreasing portal pressure) should decrease the risk of variceal rupture.12,13
Clinical Presentation
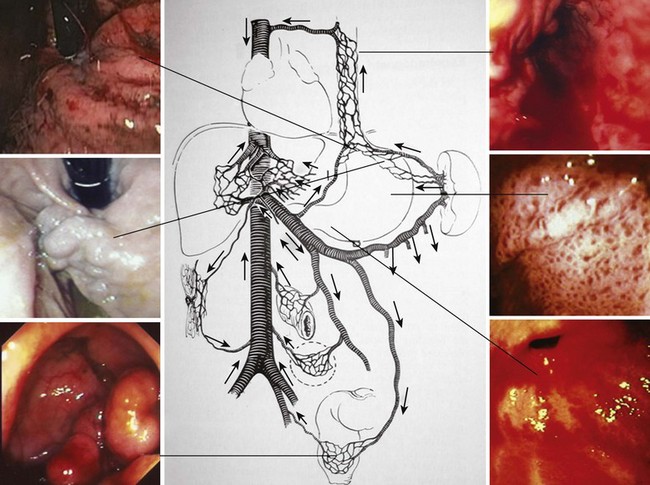
Portal hypertension should be suspected in all patients with GI bleeding in conjunction with signs of liver disease, such as ascites, jaundice, spider angiomata, gynecomastia, palmar erythema, testicular atrophy, and splenomegaly. Variceal bleeding classically manifests as effortless and recurrent hematemesis with or without dark red stools (melena). In the stomach, portal hypertension may manifest as portal hypertensive gastropathy (PHG)14,15 or gastric antral vascular ectasia (GAVE).16,17 Bleeding from either of these two conditions is usually more indolent and chronic (Fig. 13.1).
Variceal bleeding is usually associated with systemic effects including hypotension, shock, new onset of spontaneous bacterial peritonitis, or worsening encephalopathy. Spontaneous bacterial peritonitis after variceal bleeding is believed to be secondary to translocation of bacteria across the compromised mucosae.18,19 Patients with spontaneous bacterial peritonitis who were not given antibiotics had a high failure to control bleeding and higher rates of rebleeding.20 Also, in patients with ascites, infections may induce acute impairment in systemic circulatory function and hepatorenal syndrome. It is proposed that endotoxins released during bacterial infection result in an increase in portal pressure through the introduction of endothelin (a potent substance for contraction of the stellate cells), vasoconstrictive cyclooxygenase products, and contraction of hepatic stellate cells. Endotoxin-induced nitric oxide and endothelin-induced prostacyclin could inhibit platelet aggregation and reduce hemostasis at the level of the varix. Hepatic encephalopathy, which is a serious and potentially reversible disorder and known to be associated with advanced liver failure, can also be exacerbated by portal hypertension–associated GI bleeding. GI bleeding and consequent cerebral adaptation to gut-derived neurotoxins is one possible explanation. Increased levels of ammonia and mercaptans by the intestinal bacteria lead to impaired neural function secondary to cellular swelling and depletion of glutamate.
Diagnosis
Endoscopy
EGD is the most effective method for screening and surveillance of portal hypertension in patients with cirrhosis.21 The distal esophagus is the most common location for varices; however, varices can also develop in the stomach and small and large intestine.2,22 Esophageal varices occur in about 50% of all patients with cirrhosis. Gastric varices are found in approximately one of five patients with portal hypertension. About 5% to 10% of patients with gastric varices may not have esophageal varices.23 Although endoscopic evaluation of small or large bowel is not recommended in patients who are suspected to have portal hypertension (unless symptoms warrant), varices could be encountered in the small or large intestine (see Fig. 13.1).
Although EGD is recommended for all patients with a new diagnosis of cirrhosis to screen for varices, the procedure is costly, may be unpleasant, and has potential risk for complications. EGD is often performed under sedation,24–26 which includes its own cost and complications that may be more severe in patients with cirrhosis. Unsedated EGD performed with small-diameter endoscopes is being evaluated as an alternative to conventional endoscopy to avoid the direct and indirect costs of conscious sedation.27,28
Hepatic Vein Pressure Gradient
The hepatic vein pressure gradient (HVPG) is more invasive but is an accurate tool to measure portal hypertension. Portal venous pressure can be measured either directly by portal venography or indirectly by HVPG. HVPG is the difference between the wedged hepatic venous pressure (a measure of portal venous pressure) and the free hepatic vein pressure.29,30 In acute variceal bleeding, the measurement of HVPG provides prognostic information and identifies difficult-to-treat patients. In patients with acute variceal bleeding, HVPG of 20 mm Hg or greater measured soon after admission was associated with a significantly longer intensive care unit (ICU) stay, longer hospital stay, greater transfusion requirements, and worse short-term and long-term survival (1-year mortality 64% vs. 20%; P > .002).31 HVPG greater than 10 mm Hg is a good predictor of the development of varices. A threshold value of 12 mm Hg has been identified for variceal rupture.32 In cirrhotic patients with portal hypertension, the reduction of HVPG to less than 12 mm Hg or by 20% or more of the baseline value significantly reduces the risk of bleeding. Most importantly, a reduction of HVPG 20% or greater of baseline reduces the risk of death.33,34
Other Methods
Several methods have been proposed as alternatives to conventional EGD or HVPG for noninvasive diagnosis of esophageal varices,35 including platelet count-to-spleen diameter ratio, Fibrotest, and Fibroscan. Multidetector computed tomography (CT) esophagography and esophageal capsule endoscopy are considered minimally invasive. Transient elastography (Fibroscan) is a novel noninvasive method for assessing liver stiffness and is useful for diagnosis of advanced fibrosis and portal hypertension. Transient elastography is painless, rapid, and easy to perform at the bedside or in the outpatient setting. Results are expressed in kilopascals (kPa), and values range from 2.5 to 75 kPa.36 A study assessed the correlation between liver stiffness with Fibroscan and HVPG in diagnosing significant portal hypertension in 150 patients who underwent a liver biopsy and hemodynamic measurements.37 In patients with significant portal hypertension (HVPG >10 mm Hg), area under the receiver operating characteristic curves for Fibroscan was 0.945. The cutoff value of 21 kPa accurately predicted significant portal hypertension in 92% of patients for whom measurements were successful. Larger studies are needed to define precisely the role of Fibroscan in the diagnosis of portal hypertension.
Esophageal capsule endoscopy is a practical, safe, well-tolerated, and accurate method for the diagnosis of esophageal varices.38 However, interpretation of esophageal capsule endoscopy can be compromised by the presence of secretions or bubbles, and it does not detect gastric varices. An unpredictable transit time and poor interobserver agreement could account for a significant rate of failure (6% in some studies). The use of multidetector CT esophagography to grade esophageal varices has been evaluated more recently.39,40 The esophagus is insufflated with air via a catheter passed through the mouth. In the study by Kim and associates39 that included 90 patients with cirrhosis, 30 patients had large esophageal varices. CT scan performance for the diagnosis of large varices was 0.931 to 0.958 (estimated by the area under the receiver operating characteristic). Perri and colleagues40 prospectively evaluated 102 patients who underwent both CT and endoscopic screening for gastroesophageal varices. CT was found to have approximately 90% sensitivity for the identification of large esophageal varices but only about 50% specificity. The sensitivity of CT in detecting gastric varices was 87%.
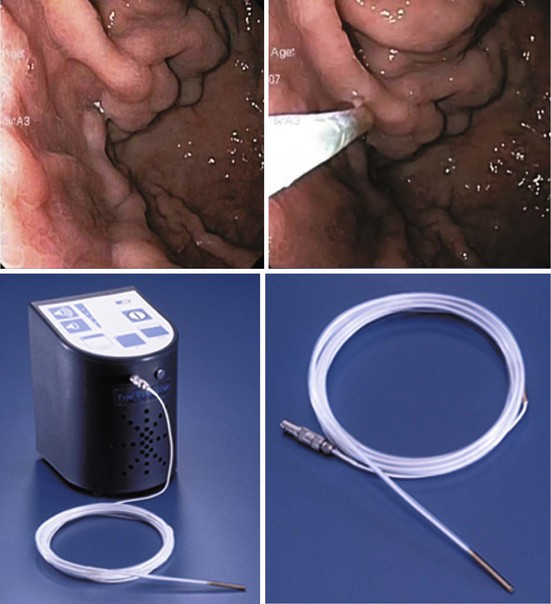
Gastric varices are harder to detect by endoscopy, especially if they are small and isolated. Small varices in the fundus are often mistaken for a mucosal fold. Their identity as varices is based on their shape (grapelike clusters) and their bluish tinge. At endoscopic ultrasound (EUS), they can be seen as circular or linear anechoic channels within the gastric wall. The addition of color Doppler or through the scope Doppler probe can differentiate gastric varices from mucosal folds.41
Grading and Classification of Varices
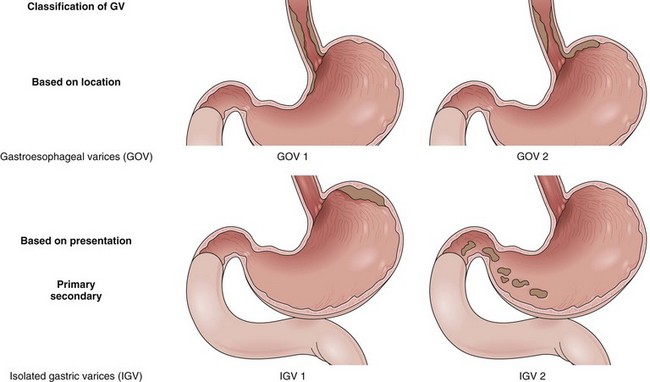
Varices are easily diagnosed by upper GI endoscopy and are categorized by their location into esophageal and gastric varices. Varices are most often seen in the distal esophagus and may extend beyond the Z line into the gastric cardia. The distal esophagus must be insufflated with air while assessing the variceal size. The most recent guidelines by the American Association for the Study of Liver Diseases (AASLD) recommend classifying esophageal varices as either small (<5 mm) or large (>5 mm) (Fig. 13.2).42
Esophageal varices can also be graded using several classifications for documentation and research purposes.43–45 According to Conn,43 the number of varices is graded as follows: 1+, a single varix; 2+, two to three varices; 3+, four to six varices; and 4+, more than six varices. The size of the varices is graded as follows: 1+, small varices detectable only on performing Valsalva maneuver; 2+, small varices (approximately 1 to 3 mm in diameter) visible without Valsalva maneuver; 3+, varices of moderate size (3 to 6 mm in diameter); and 4+, large varices (>6 mm). Extent of esophageal involvement is graded as follows: 1+, terminal 3 cm; 2+, terminal 6 cm; 3+, terminal 9 cm; and 4+, involving more than the terminal 9 cm.
Certain types of varices are more likely to appear depending on the cause of portal hypertension. Isolated gastric varices located on the fundus (IGV1) classically occur in association with splenic vein thrombosis. Duodenal and biliary varices can occur more often with extrahepatic causes of portal hypertension.46 A simple classification of gastric varices depending on their anatomic location in the stomach can also help in understanding their natural history and approach to management.47 Gastroesophageal varices are located in the esophagus and extend in continuity to the lesser curve (GOV1) or greater curve (GOV2) of the stomach. Isolated gastric varices are located usually on the fundus (IGV1) or greater curve or other sites in the stomach or first part of duodenum (IGV2) (Fig. 13.3). In more recent publications as well as in our own experience, the use of a through the scope Doppler probe not only facilitates the diagnosis, but it also confirms successful therapy of gastric varices (Fig. 13.4).41
Predictors of Variceal Bleed
The North Italian Endoscopic Club uses the extent of liver disease, large variceal size, and the presence of red color signs on endoscopy as an index for the likelihood of first variceal bleeding.48 Of the above-mentioned indicators, variceal size seems to be the most important predictor of first variceal bleeding. The probability of variceal bleeding is significantly greater in patients with larger esophageal varices (P = .0001), with more severe red wale marks (P = .0001), or with more severe liver dysfunction according to the Child-Pugh classification (P = .007).49 However, because only one-third of patients who present with variceal hemorrhage have the previously mentioned risk factors, a better definition of predictive factors is needed.
Sarin and Kumar47 examined 12 clinical, endoscopic, and hemodynamic variables in 126 patients with portal hypertension (72 bleeders and 54 nonbleeders). The variceal size and intravariceal pressures were the most important predictors of hemorrhage. In another study, the risk of bleeding was 0% when the variceal pressure was 13 mm Hg or less, 9% when the variceal pressure was 13 to 14 mm Hg, 17% when the variceal pressure was 14 to 15 mm Hg, 50% when the variceal pressure was 15 to 16 mm Hg, and 72% when the variceal pressure was greater than 16 mm Hg.50
HVPG is a measure of portal pressure and intravariceal pressure in patients with cirrhosis. Garcia-Tsao and colleagues32 found that HVPG was significantly greater in 49 patients who had bled from esophageal varices than in 44 patients with cirrhosis who did not bleed (20.4 ± 5.1 mm Hg vs. 16.0 ± 5.2 mm Hg). They also found that none of the patients who had bled had HVPG less than 12 mm Hg. In one study, the portocaval pressure gradient decreased after transjugular intrahepatic portosystemic shunt (TIPS) procedure (from 19.7 ± 4.6 mm Hg to 8.6 ± 2.7 mm Hg), and a subsequent increase in pressure greater than 12 mm Hg (18.4 ± 7.46 mm Hg) was associated with rebleeding.51 Moitinho and coworkers31 reported that patients admitted because of variceal bleeding who had HVPG greater than 20 mm Hg measured within 48 hours had a fivefold increased risk of (1) failure to control bleeding with the emergency treatment or (2) experiencing early rebleeding. Dynamic measurements of HVPG are more valuable to assess the influence of therapeutic interventions or alcohol abstinence. Active bleeding at endoscopy was statistically shown to be an independent risk factor in predicting failure to control variceal bleeding.52
Natural History of Varices
Gastroesophageal varices are the most significant portosystemic collaterals because their rupture results in variceal hemorrhage, the most common lethal complication of cirrhosis.53 The prevalence and rate of growth of varices in cirrhotics are often related to the severity of liver disease. All patients should be screened for varices at the time of diagnosis of cirrhosis. Patients who have no varices on screening endoscopy should be rescreened every 2 to 3 years if their liver function is stable or earlier if there are signs of hepatic decompensation. Patients who have small varices on screening endoscopy should be rescreened every 1 to 2 years because the development of large varices is greater in patients with small varices on initial endoscopy compared with patients with no varices.42
About one-third of patients with varices experience a variceal hemorrhage. The 2-year bleeding risk in patients with cirrhosis and moderate to large varices is 25% to 30%. Lifelong risk of variceal bleeding is almost 50%.54 In portal vein obstruction, the bleeding rate is even higher. After varices start bleeding, hemorrhage spontaneously stops in only 50% of cases. Patient’s with Child C cirrhosis and actively spurting varices are particularly likely to continue to bleed without active intervention. After cessation of active bleeding, the risk of rebleeding is higher for approximately 6 weeks. The risk of early rebleeding is greatest within the first 48 hours, and about half of all early rebleeding episodes occur during this time. Risk factors for early rebleeding include large varices, age older than 60 years, severity of initial bleed, renal failure, ascites, active bleeding on endoscopy, and red wale marks (defined as longitudinal dilated venules resembling whip marks on the variceal surface). Aggressive volume replacement may exacerbate portal hypertension and precipitate early rebleeding.
Of patients who bleed from esophageal varices, the variceal hemorrhage is fatal in roughly 20% of patients. The incidence of new varices is approximately 5% to 15% per year, depending on the Child-Turcotte-Pugh class1 and the etiology of the liver disease.2,22 The risk of gastric variceal bleeding is lower than the risk of esophageal variceal bleeding, but gastric variceal bleeding, especially fundal varices, tends to be more severe, to require more transfusions, and to have a higher rate of mortality.23 Gastric variceal bleeding has been reported to account for 3% to 30% of all acute variceal bleeding episodes. The risk of bleeding from gastric varices depends on the location. Although GOV1 constitute more than 70% of gastric varices, only 11% of GOV1 ever bleed. In contrast, although IGV1 constitute less than 8% of all gastric varices, 80% of IGV1 bleed.19 IGV1 are often fed by spontaneous large collaterals that partly decompress the portal vein, and IGV1 are associated with lower portal pressures than esophageal varices. IGV2 are rare (4.7% of all gastric varices); commonly seen in antrum (53%), duodenum (32%), or at both sites (11%); and rarely in body and fundus (4%). Overall, gastric varices bleed less often but more severely than esophageal varices.55
Management
Endoscopic and Pharmacologic Therapy
Primary Prophylaxis to Prevent Esophageal Variceal Bleeding
Primary prophylaxis of variceal bleeding or prevention of the first episode of variceal hemorrhage is the most logical approach to decrease morbidity and mortality after a variceal bleed. Because only about 10% to 20% of patients bleed, it is essential to select carefully patients who are at a high risk of variceal hemorrhage. In patients without varices, nonselective β blockers were proposed with the aim of preventing the development of varices.56 In a large multicenter study, 213 cirrhotic patients with portal hypertension (HVPG >5 mm Hg) but without varices were randomly assigned to receive timolol or placebo in double-blind conditions for a median of 55 months.57 The rate of the development of esophageal varices did not differ between the two groups, and the timolol group reported more adverse events. These results do not support the universal use of β blockers in cirrhotics without varices. In patients with no varices on endoscopy, there is no indication for treatment to prevent the formation of varices.
Patients who have varices may benefit from the interventions directed toward prevention of first bleeding. Endoscopic sclerotherapy, which is not commonly used at the present time, was compared with no treatment in 20 randomized trials that included 1756 patients, most of whom had medium-sized or large-sized varices. In the sclerotherapy group, there was a significant reduction in bleeding in 5 trials, increase in bleeding in 2 trials, and no difference in 13 trials.58 Because of significant heterogeneity in the results with regard to bleeding and mortality among the different trials, prophylactic sclerotherapy is not recommended for primary prophylaxis.59,60 In patients who have small varices that have not bled, β blockers can be used to prevent the progression of varices and bleeding. A meta-analysis evaluating nonselective β blockers in the prevention of first variceal bleed investigated the results of three trials that included patients with small varices.61 The group receiving β blockers showed a reduction in the incidence of first variceal hemorrhage (2% over 2 years) compared with the nontreated group (7% over 2 years), but the reduction was not statistically significant.
Prophylaxis is important in patients who are considered at high risk for bleeding because of advanced liver disease and the presence of red wale marks on varices.21 Regarding patients with medium to large varices, a meta-analysis of 11 trials comprising 1189 patients evaluated nonselective β blockers (i.e., propranolol, nadolol) versus placebo in the prevention of first variceal bleeding and showed that the risk of bleeding was significantly reduced by β blockers (30% in control vs. 14% in β blocker group). This meta-analysis indicates that one bleeding episode is avoided for every 10 patients treated. More importantly, mortality was lower in the β blocker group compared with the control group, and this difference has been shown to be statistically significant.62 β blockers might not be tolerated by all patients, and there might be some contraindications, such as in patients with asthma, insulin-dependent diabetes, and peripheral vascular disease. The most common side effects in cirrhotics are lightheadedness, fatigue, and shortness of breath.
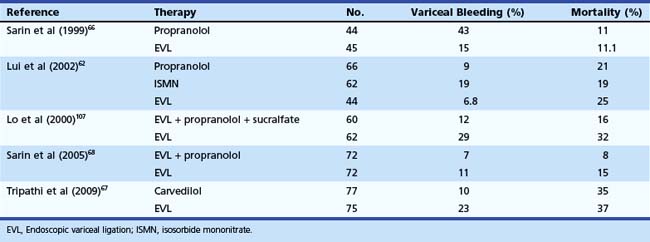
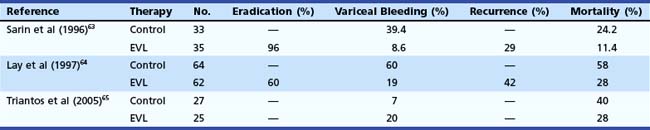
In the last 2 decades, EVL has essentially replaced sclerotherapy as a mode of variceal eradication, and it has been evaluated for preventing the first bleed from esophageal varices. In a series of 68 patients, Sarin and coworkers63 showed the superiority of EVL compared with no therapy to prevent first variceal bleed (Table 13.2). Their results were subsequently confirmed by Lay and colleagues,64 who found significant reduction in the incidence (19% vs. 60%) and mortality (28% vs. 58%) of first bleed when EVL was compared with no therapy. In contrast to these reports, a more recent study showed no benefit of EVL; however, the patients included in this study were either intolerant to or had contraindication for the use of β blockers.65
Table 13.2 Endoscopic Variceal Ligation (EVL) versus No Treatment for Prevention of First Bleeding from Esophageal Varices
After the initial encouraging reports, it was logical to assess whether EVL is comparable to the current therapy for primary prophylaxis—β blocker therapy. Sarin and coworkers66 randomly assigned 89 patients with high-risk varices to receive EVL or propranolol. The actuarial probability of bleeding at 18 months was significantly lower in the EVL group (15.8%) compared with the propranolol group (43%). There was no survival benefit with EVL, however. Lui and colleagues62 assigned 172 patients to EVL (n = 44), propranolol (n = 66), or isosorbide mononitrate (ISMN) (n = 62) therapy (Table 13.3). On intention-to-treat analysis, variceal bleeding was observed in 7% of patients randomly assigned to EVL, 14% of patients randomly assigned to propranolol, and 23% of patients randomly assigned to ISMN; the difference between EVL and nitrates was significant. A significant number of patients reported side effects with drug treatments (45% propranolol and 42% ISMN vs. 2% EVL), resulting in withdrawal from treatment in 30% of patients receiving propranolol and 21% of patients receiving ISMN. There was no significant difference in mortality rates in the three groups.
A more recent randomized controlled trial found carvedilol to be more effective in preventing first variceal bleed than EVL in patients with high-risk esophageal varices.67 Sarin and coworkers68 noted that although addition of propranolol to EVL does not decrease the probability of first bleed or death, the recurrence of varices is lower if propranolol is added to EVL. Several meta-analyses have been performed comparing EVL with β blockers.69–71 The meta-analysis performed by Imperiale and Chalasani69 included five trials with 601 patients. Khuroo and associates70 included eight trials comprising 596 patients. More recently, Gluud and coworkers71 performed a meta-analysis of 15 randomized controlled trials comprising 1174 patients. Imperiale and Chalasani69 and Khuroo and associates70 concluded that in patients with large varices that are high risk for bleeding, EVL decreases bleeding episodes; however, there was no reduction effect on mortality. Gluud and coworkers71 noted that the positive effects associated with the EVL group were more commonly seen in the trials that had shorter follow-up.
There are several distinct advantages of EVL over β blockers, as follows:
Teran and colleagues72 examined the cost-effectiveness of various treatments in primary prophylaxis of variceal bleeding. They found that β blockers were more cost-effective than sclerotherapy or shunt surgery in patients with cirrhosis with a cost savings between $440 and $1460. The other treatments were not cost-effective. Spiegel and coworkers found empiric β blocker therapy for primary prophylaxis of variceal hemorrhage to be a cost-effective measure because the use of screening endoscopy to guide therapy adds significant cost with only marginal increase in effectiveness.
The Baveno IV consensus recommended that nonselective β blockers should be considered as first-choice treatment to prevent first variceal bleeding in patients with high-risk varices, and EVL should be offered to patients with contraindications or intolerance to β blockers.21 HVPG can also be monitored while receiving treatment with a β blocker. If HVPG is reduced by 25% or more or the gradient is less than 12 mm Hg after 4 to 6 weeks of therapy, the drug should be continued. A more noninvasive method of measuring efficacy of β blockers is by noting a decrease in the patient’s pulse rate. AASLD and American College of Gastroenterology also consider β blockers as first choice in patients with medium to large varices that have not bled and are not high risk. In patients with high-risk varices, the combination of EVL and β blockers is considered first-choice therapy.
Management of Active Esophageal Variceal Bleeding
Active bleeding has been defined by the Baveno II Consensus Workshop as oozing or spurting at the time of endoscopy. Clinically significant bleeding is defined as bleeding with a transfusion requirement of 2 or more units of blood within 24 hours of time zero, together with a systolic blood pressure less than 100 mm Hg or a postural change of greater than 20 mm Hg or pulse rate greater than 100 beats/min at time zero.73