Chapter 52 Endoscopic Management of Post–Bariatric Surgery Complications
![]() Video related to this chapter’s topics: Prototype Operating Endoscope
Video related to this chapter’s topics: Prototype Operating Endoscope
Introduction
As the field of bariatric surgery continues to grow in pace with the increasing prevalence of obesity, an increasing number of patients are referred for endoscopic evaluation after bariatric surgery. Endoscopic findings may represent the normal postsurgical appearance or a complication. A basic understanding of the anatomic changes and potential complications associated with bariatric procedures is essential for optimal endoscopic assessment and appropriate management. A thorough review of the surgical report and any relevant imaging studies are key elements for a successful endoscopic procedure.1 Recognizing that certain complications are unique to specific types of bariatric surgery allows for accurate diagnosis and therapy. Close communication and collaboration with the bariatric surgeon is strongly recommended before endoscopy, particularly when therapy is contemplated.
Roux-en-Y Gastric Bypass
Marginal or Stomal Ulcers
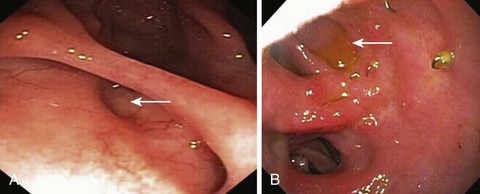
Marginal or stomal ulcers are ulcerations at the gastrojejunostomy that frequently occur on the jejunal side of the anastomosis (Fig. 52.1). Marginal ulcers may be seen in 16% of patients after Roux-en-Y gastric bypass (RYGB).2 Many ulcers remain subclinical, and the true incidence is likely higher. Ulceration can occur at any time but patients usually present within 3 months of surgery with pain, nausea, bleeding, or perforation.3,4 Several potential and controversial inciting factors are implicated, including gastrogastric fistula, large gastric pouch with inclusion of parietal cells and resultant acid exposure, ischemia, foreign body reaction to staples or nonabsorbable sutures at the anastomosis, Helicobacter pylori, nonsteroidal anti-inflammatory drugs (NSAIDs), and gastric pouch orientation.5–7 The etiology is probably multifactorial with ischemia the likely culprit. Preoperative H. pylori testing and eradication is not routinely recommended because of conflicting data that this practice reduces the incidence of marginal ulceration.8,9 During upper endoscopy, the gastric pouch should be closely inspected for a gastrogastric fistula, and biopsy specimens should be obtained for H. pylori. Patients usually respond to treatment with proton pump inhibitors, liquid sucralfate, and H. pylori eradication therapy when appropriate.10,11 NSAIDs should be avoided, and smoking should be discontinued. Endoscopic removal of foreign material, such as nonabsorbable suture or staples, may help ulcer resolution. In cases of symptomatic refractory ulceration, surgical revision may be required.
Stomal Stenosis
Stomal stenosis is an important complication that occurs in approximately 3% to 12% of patients after open RYGB and in 11% to 27% of patients after laparoscopic RYGB.2,4 Most strictures occur within the first year after surgery, with a mean time interval of 2 to 3 months to diagnosis.12,13 Patients present with nausea, vomiting, pain, or dysphagia. The exact mechanism for stricture formation is unknown, but ischemia, ulceration, subclinical anastomotic leak, circular stapler size, and surgical expertise are potential contributing factors.13,14 The gastrojejunostomy is intentionally created to be 11 to 15 mm in diameter. Although there is no clear definition for stomal stenosis, the latter is diagnosed when the luminal diameter is less than 10 mm or when passage of a standard upper endoscope through the anastomosis is met with resistance (Fig. 52.2).
In cases of symptomatic strictures, serial dilation using a through the scope balloon dilation catheter is preferred with the goal of achieving a stomal diameter of 10 to 12 mm. Dilation should not exceed 15 mm. The initial balloon size is based on the estimated diameter of the anastomotic stricture. Three sequential sizes may be inflated during one session, in keeping with the recommended “rule of 3’s” for stricture dilation. An effective dilation results in partial disruption of the anastomotic wall. Caution is warranted in the setting of coexistent marginal ulceration because of increased risk of perforation. Overzealous dilation, which can result in perforation or an overstretched anastomosis with resultant dumping syndrome and regain of weight, should be avoided. When a tight stricture precludes traversal with the endoscope and impairs visualization of the postanastomotic jejunal limbs, wire-guided through the scope balloon dilation under fluoroscopy is recommended. The reported perforation rate after balloon dilation approximates 2% to 3%.13,15 Small perforations can be managed conservatively.
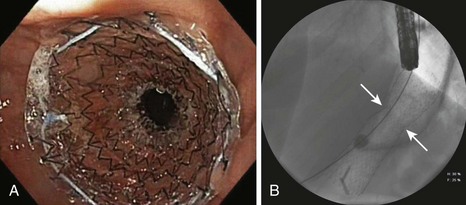
Most (>90%) strictures are responsive to endoscopic balloon therapy.12,16 Most strictures can be effectively dilated in one or two sessions, but tight strictures may require several sessions. The time interval between sessions ranges from 1 to 3 weeks.15,16 The successful use of bougie dilators has been reported, but this technique requires guidewire placement within the jejunal Roux limb before dilation.17 Although temporary placement of a fully covered stent in selected patients with refractory strictures may be successful at achieving long-term stoma patency, a high rate of stent migration (>50%) has been observed in some studies (Fig. 52.3).18 If stent placement is contemplated, it is best to avoid dilating the stricture before stent placement to minimize the risk of migration. The duration of stent placement is typically 3 months. Other therapeutic techniques, including needle-knife electroincision of the anastomosis (which carries an increased risk of perforation) and intralesional steroid injection after balloon dilation, have been reported with some success.19,20 In the rare case in which endoscopic therapy is ineffective, surgical revision may be necessary. Patients with a modified RYGB with a Silastic ring around the proximal pouch to prevent dilation of the gastrojejunostomy may require surgical removal or replacement of the band.
Gastrogastric Fistula
The reported incidence of staple line dehiscence with resultant gastrogastric fistula varies with the extent of division of the excluded stomach and is greater than 20% when the gastric pouch and bypassed stomach are undivided or partially divided to less than 5% when the segments are completely transected.21,22 Gastrogastric fistula denotes an abnormal communication between the neogastric pouch and the bypassed stomach. There are several postulated reasons for the development of fistulas, including surgical technique without complete division of the gastric pouch, marginal ulceration, anastomotic leak, and foreign body erosion.21,23 Even when the pouch is completely transected, a gastrogastric fistula can occur if the pouch is situated in close proximity to the bypassed stomach. Surgical interposition of omentum or a loop of jejunum between the segments may reduce this complication.24 Patients usually present with regain of weight, abdominal pain, or reflux symptoms. When a gastrogastric fistula is suspected, diagnosis is confirmed by upper endoscopy, upper gastrointestinal (GI) series, or in some instances abdominal computed tomography scan with oral contrast agent.
Gastrogastric fistulas are frequently small and easily overlooked. Endoscopically, a small gastrogastric fistula can appear as a diverticulum in the gastric pouch; larger fistulas allow endoscope passage into the excluded stomach (Fig. 52.4). When gastrogastric fistulas are associated with marginal ulceration, gastric biopsy specimens for H. pylori should be obtained. Barium studies are helpful in diagnosing small dehiscences. Most symptomatic patients require surgical intervention. However, in patients with small gastrogastric fistulas and associated marginal ulcers, an initial conservative approach consisting of proton pump inhibitor therapy, liquid sucralfate, or H. pylori eradication, as appropriate, may be effective.21,23 NSAID use and smoking should be strictly avoided. Patients are reevaluated after 4 to 8 weeks; if the fistula is healed, long-term use of a proton pump inhibitor is advised.21,23 In patients with small gastrogastric fistulas (<5 mm) who are unresponsive to medical therapy, endoscopic therapy, in the form of endoscopic suturing, argon plasma coagulation, fibrin glue injection, hemoclip application, or a combination thereof, may be considered given the reported successful outcome in small case series.23,25,26 Long-term follow-up data are awaited before any particular endoscopic therapy can be formally recommended for this select group of patients.