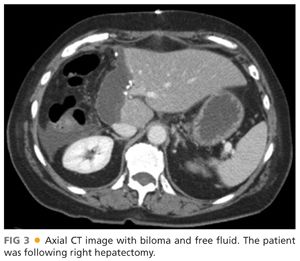
■ When a broader view of the abdomen is needed, a CT scan can be performed. Intravenous (IV) contrast is routinely administered, and due to the nature of the exam, the patient will be exposed to radiation (equivalent of ~100 chest x-rays) (FIGS 2 and 3).

■ MRCP can also be performed to evaluate the biliary system and surrounding liver parenchyma. Note that the nature of the magnetic resonance (MR) protocol that is required to optimally visualize, the biliary system, does not optimally assess surrounding structures, thus limiting the evaluation of nonbiliary pathology (FIG 4).

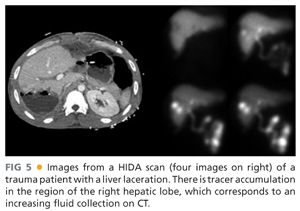
■ When evaluating for a bile leak, cholescintigraphy (also known as a hepatobiliary iminodiacetic acid [HIDA] or diisopropyl iminodiacetic acid [DISIDA] scan) can be performed. The radiopharmaceutical is taken up by the liver and excreted into the bile. When the tracer is seen accumulating outside of the liver, or in intrahepatic cavities, the diagnosis of leak can be confirmed (FIG 5).
SURGICAL MANAGEMENT
Preprocedure Planning
■ All related imaging to the patient’s condition should be reviewed. A PTC/PTHD can be performed either under conscious sedation or with general anesthesia (preferred). Thus, the patient ideally will be nil per os for at least 6 hours prior to the procedure.
■ For any procedure that manipulates the biliary system, there is an increased risk of septicemia and endotoxemia. The patient should receive antibiotics within 1 hour of start time. The mix of gastrointestinal flora should guide antibiotic choice (gram negatives and anaerobes). At our institution, piperacillin/tazobactam 3.375 g is routinely used. In patients who are penicillin allergic, ciprofloxacin 400 mg and metronidazole 500 mg are given.
■ Unless the left-sided ducts are unilaterally dilated, a right-sided approach is routinely used, as this will drain a larger portion of the liver and will decrease radiation exposure to the interventionalist.
Positioning
■ Biliary procedures are performed with the patient in the supine position, arms at the side.
TECHNIQUES
PERCUTANEOUS TRANSHEPATIC CHOLANGIOGRAPHY
Immediate Preprocedure
■ The patient’s abdomen should be cleaned and prepped from the nipple line to the left midaxillary line to 5 cm below the umbilicus and beyond the right posterior axillary line.
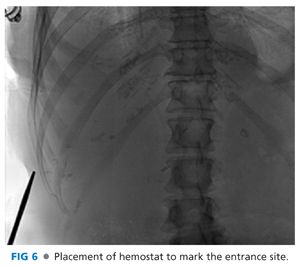
■ When right-sided access is warranted, a hemostat should be placed at the right midaxillary line at the selected access site during deep inspiration (FIG 6). This is used to verify that the entrance site is below the greatest diaphragmatic excursion. Access above this mark should not be attempted as it exposes the patient to the risk of violating the pleura, resulting in pneumothorax or biliary–pleural fistula.
■ Local anesthetic should be used and a small incision (2 to 3 mm) made to facilitate needle passage.
Duct Cannulation
■ Duct cannulation can be performed with a 15-cm, 21- or 22-gauge Chiba needle. These needles are relatively small (thereby reducing bleeding risk) and can accept a 0.018-in wire.
■ When left-sided access is required, US is routinely used to localize a relatively superficial duct. The duct is then cannulated under direct US guidance.
■ Due to the overlying ribs, right-sided access is usually accomplished with a “blind” technique, which can either be subclassified into an antegrade or retrograde approach.
■ When using the retrograde approach, the Chiba needle is advanced from the liver margin to the midaxillary line. The stylet is removed, and under fluoroscopy, a small amount of dilute contrast is injected as the needle is pulled back.
■ When using the antegrade approach, the stylet is removed from the Chiba needle, and under fluoroscopic guidance, the needle is advanced while injecting dilute contrast until reaching the midclavicular line.
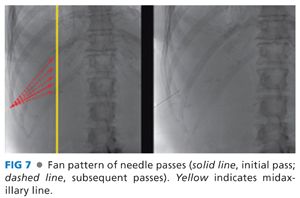
■ Regardless of approach, multiple passes through the liver at different obliquities (cranial–caudal and anterior–posterior) are often required before a duct is cannulated (FIG 7). The technical challenge and number of passes required for successful cannulation is directly related to the extent of intrahepatic biliary dilation. This is particularly problematic in the setting of bile duct injury with a biliary tree that is fully decompressed into the peritoneal space.
■ Peripheral cannulation is the goal. Cannulation of centrally located duct increases the risk of arteriobiliary or venobiliary fistula and hemorrhage.
Cholangiogram
■ It is very easy for a well-placed needle to dislodge while the patient is breathing. To prevent this from occurring, a 0.018-in wire is placed through the Chiba needle and coiled within the biliary system. The needle is exchanged for the inner portion of an AccuStick catheter. A Tuohy-Borst sidearm introducer is then placed over the wire and attached to the catheter, allowing for contrast injection without loss of wire access.
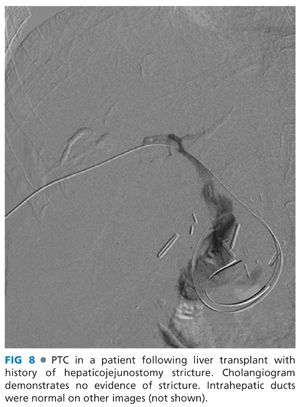
■ While injecting dilute contrast, either an angiographic run or static images are obtained in multiple obliquities (FIG 8).
■ Once adequate images are obtained, the catheter and wire are removed.
PERCUTANEOUS TRANSHEPATIC DRAIN
■ If durable access to the biliary tree is indicated, once a 0.018-in wire is coiled within the biliary system, a fully assembled AccuStick is advanced and the inner metallic cannula and 4-Fr catheter are removed. A hydrophilic wire and hockey-stick catheter are then used to cannulate the small bowel.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








