Chapter 32 Percutaneous approaches to the treatment of gallbladder disease
Image-Guided Intervention
Image-guided interventional techniques have been developed to provide minimally invasive treatment of gallbladder disease (see Chapters 28 and 31). Percutaneous, image-guided cholecystostomy is now an accepted method to decompress the acutely inflamed gallbladder if surgery is not indicated. Various methods aiming at elective, nonsurgical removal of gallbladder stones were introduced in the early 1990s, including extracorporeal shock-wave lithotripsy (ESWL), contact dissolution of gallstones with methyl tert-butyl ether (MTBE), and percutaneous mechanical cholecystolithotomy. As a result of the successful introduction of laparoscopic cholecystectomy (see Chapter 34), surgical treatment of cholecystolithiasis has become less invasive, and definitive treatment of cholecystolithiasis may be accomplished with much shorter hospitalization. Because none of the existing nonsurgical techniques of gallstone removal can prevent recurrent gallstone formation, the indication to perform percutaneous gallstone removal without surgery is now very limited. This chapter gives an overview of image-guided treatment methods for gallbladder disease.
Percutaneous Cholecystostomy for Acute Cholecystitis
Surgical cholecystostomy (see Chapters 28 and 31) has long been used to provide external decompression of the acutely inflamed gallbladder in patients who are at high risk for operation or general anesthesia, such as those with sepsis, diabetes, or severe cardiac, pulmonary, hepatic, or renal failure. Percutaneous cholecystostomy was initially developed to provide a minimally invasive method of gallbladder decompression in elderly and very ill patients with acute acalculous or calculous cholecystitis or with gallbladder hydrops secondary to malignant disease (Elyaderani & Gabriele, 1979; Pearse et al, 1984). Percutaneous cholecystostomy also has been used to treat complications of cholecystitis (e.g., gallbladder perforation, empyema, or pericholecystic abscesses) or as an alternative to percutaneous transhepatic drainage of the bile ducts in obstructive jaundice. More recently, percutaneous cholecystostomy has been used to provide access to the gallbladder for elective gallstone treatment with stone dissolution techniques, percutaneous cholecystolithotomy, or other techniques.
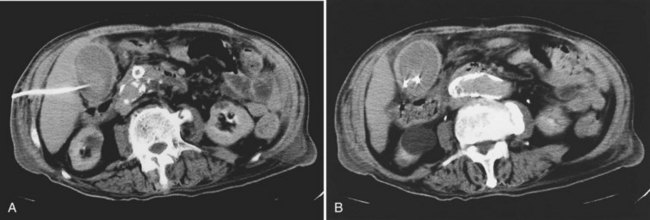
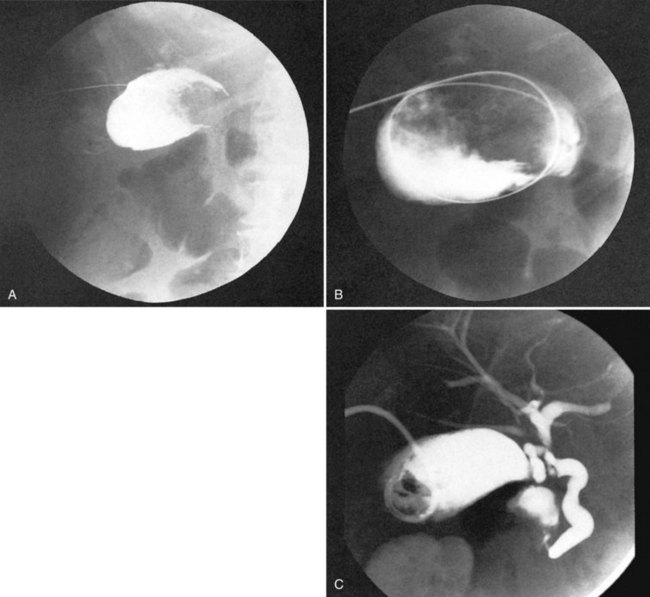
The percutaneous access route to the gallbladder usually is determined with ultrasound (US) and is based on the individual anatomic situation. Computed tomography (CT) can be used if US does not provide sufficient information. Most authors favor the transhepatic approach to the gallbladder, because a puncture through the attached portion of the gallbladder should reduce the risk of bile leakage into the peritoneal cavity (Fig. 32.1). The area of attachment cannot be anticipated reliably with imaging techniques, and the direct, transperitoneal route also has been used successfully (Vogelzang & Nemcek, 1988). The acutely inflamed gallbladder is usually distended and immediately adjacent to the anterior abdominal wall, and the direct approach through the gallbladder fundus avoids the trauma to the liver that may be associated with percutaneous gallstone removal at a later date. The use of a removable percutaneous anchor was proposed to prevent the gallbladder wall from moving away from the trocar or from the catheter during exchange over a guidewire (Cope et al, 1990).
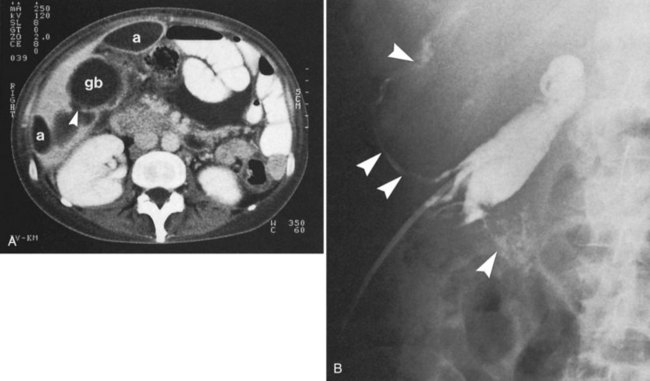
The initial gallbladder puncture is performed under local anesthesia, and prophylactic administration of atropine has been recommended to prevent vasovagal reactions (vanSonnenberg et al, 1984). With portable US equipment, the percutaneous cholecystostomy procedure can be performed at the patient’s bedside (e.g., in the intensive care unit). If there is doubt regarding a safe access route, however, it may be preferable to combine US or CT with fluoroscopy (Fig. 32.2). Several suitable needle/catheter or needle/guidewire systems are available, and the optimal method of catheter introduction is a matter of personal preference. Repeat punctures with introducer needles should be avoided, because leakage of gallbladder content through the puncture channel may lead to internal decompression of the gallbladder into the peritoneal cavity and prevent further attempts to enter the gallbladder lumen. A catheter size of 6.5 to 7 Fr is usually sufficient to provide effective external gallbladder drainage, but 8 Fr or more may be necessary to drain gallbladder empyema or pericholecystic abscesses (Fig. 32.3; vanSonnenberg et al, 1991). If percutaneous cholecystostomy is done for acute cholecystitis, catheter manipulations should be kept to a minimum to avoid inadvertent perforation of the frail inflamed gallbladder wall or leakage of gallbladder contents alongside the catheter. To prevent inadvertent dislodgment of the catheter on the ward, it is preferable to use a self-retaining catheter. Diagnostic cholangiography through the cholecystostomy catheter may be obtained after a few days to assess the presence of gallstones and patency of the cystic duct. It is advisable to leave the cholecystostomy catheter in place for 7 to 10 days to let a tract develop and to avoid bile leakage into the peritoneal cavity.
Although transient right upper quadrant pain is a relatively common side effect of percutaneous cholecystostomy, serious procedure-related complications are uncommon. In a review of 252 percutaneous cholecystostomies reported in the English language literature, there were 4 cases of bile peritonitis and 1 death (0.3%); other procedure-related complications included vasovagal reaction or hypotension, self-limited hemobilia, and acute cholecystitis secondary to an impacted stone in the cystic duct (Teplick, 1989). In a series of 127 patients undergoing gallbladder puncture and cholecystostomy, the reported rate of minor and major complications was 3.9% and 8.7%, respectively. The 30-day mortality rate of that series was 3.1%, but all deaths were due to underlying diseases (vanSonnenberg et al, 1992).
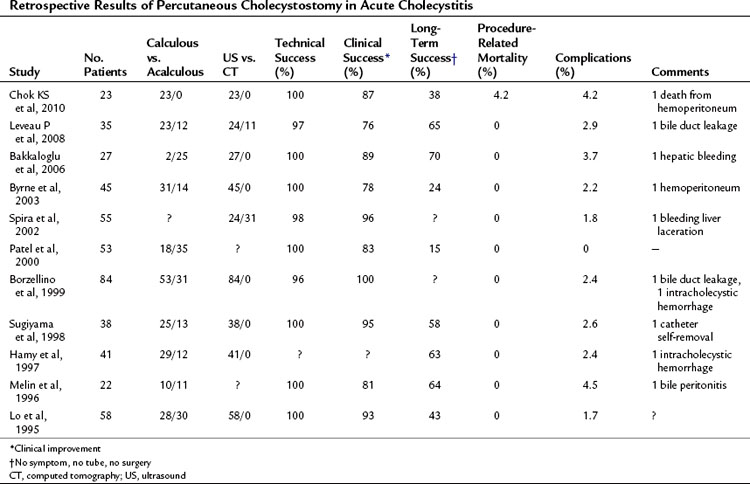
In view of the severely compromised health of most patients undergoing the procedure, percutaneous cholecystostomy is relatively safe. The efficacy of percutaneous cholecystostomy is difficult to determine, because the diagnosis of acute cholecystitis is often unreliable in patients with multiple concomitant medical and surgical problems (McGahan & Lindfors, 1988, 1989). If the indication for percutaneous cholecystostomy is restricted to patients with clinical or imaging findings of acute cholecystitis, a response rate of 90% can be expected (van Overhagen et al, 1996). If patients with unexplained abdominal sepsis are included, the response rate is lower (Boland et al, 1994; Lee et al, 1991; McGahan & Lindfors, 1989). In patients with acute acalculous cholecystitis, interval cholecystectomy may be unnecessary, and percutaneous cholecystostomy may be a definitive therapy (Vauthey et al, 1992). A randomized, controlled trial showed that percutaneous cholecystostomy and drainage is significantly more effective than simple gallbadder aspiration (Ito et al, 2004). Results of retrospective clinical studies on percutaneous cholecystostomy are summarized in Table 32.1. Current experience indicates that percutaneous cholecystostomy is an effective temporizing measure in elderly or critically ill patients with acute cholecystitis and a safe alternative to emergency surgery (Chok et al, 2010). Recently, this has been recognized by a surgical consensus conference (Miura et al, 2007). In clinical situations that warrant, interval cholecystectomy can be performed on an elective basis.
Nonsurgical Techniques to Remove Gallbladder Stones
Percutaneous Gallstone Removal via Cholecystostomy
Percutaneous Contact Dissolution of Gallbladder Stones with Methyl Tert-Butyl Ether
MTBE is the most potent cholesterol solvent available. Because of its boiling point of 55.2° C, it remains liquid at body temperature and is easier to handle than diethyl ether. Direct instillation of MTBE through a small percutaneous cholecystostomy catheter has been used successfully to dissolve cholesterol stones of the gallbladder within hours (Allen, 1985). Most treatments with MTBE have been done on an elective basis in patients who had an increased risk of surgery or anesthesia because of coexisting medical conditions or who refused to undergo surgery for other reasons (Hellstern et al, 1990; Thistle et al, 1989). The selection criteria for MTBE therapy includes symptomatic uncomplicated gallstone disease, uncalcified gallstones on CT, and normal hepatic laboratory test results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree