Chapter 13 Pediatric Gynecology
APPROACH TO THE PEDIATRIC GYNECOLOGY PATIENT
Establishing Confidentiality
With an older child (over age 10) with concerns of sexual abuse and with all adolescents, all questions regarding sexual history, vaginal discharge, and vulvar itching should be asked without a parent in the room. Adolescents are often loathe to answer questions honestly with a parent listening, especially if they are engaging in a risk behavior about which they don’t want the parents to know. Older children with suspected sexual abuse may not wish to disclose with the perpetrating parent or the spouse of the perpetrator present for fear of punishment at disclosure or for fear of not being believed, with consequences for “lying.” Establishing confidentiality provides an opportunity to ask questions directly of the child without the influence of the parents, with an expectation of honesty. The child or adolescent may still withhold the truth, often delaying to determine whether the clinician is “trustworthy” or if he/she can really help.
The HEADS Questions
The major adolescent morbidities and mortalities stem from risk-taking behaviors rather than disease processes. Therefore, questions designed to elucidate those risk-taking behaviors in an expedient way can be used to avoid the “Oh By the Way” experience, or the major problem casually mentioned in the last few minutes allotted for a visit. A useful acronym for obtaining the psychosocial history from an older child or adolescent is HEADS.1,2 Table 13-1 outlines these questions, which are geared more toward the adolescent but can be modified into simpler terms for the child. With risk behaviors such as cigarettes or drugs, asking about peers’ or friends’ use can be particularly helpful with the older child or younger adolescent, because they may easily talk about others’ risk behaviors, which can then make it easier to talk about themselves.
Table 13-1 The HEADS Examination
| Home: Who lives in the home? What happens when there is an argument in the home? |
| If father is not in the home, how often does the child see him? Does that feel like the right amount? In cases of sexual abuse, any boy babysitters? Any alone time with stepfathers, uncles, neighbors, cousins? |
| Education: What grade is the child in? How are their grades this year? How were they last year? |
| Activities: How does the child spend their time? Any sports, or other activities? For teens, are they in a gang or do they have access to a gun? |
| Drugs: Do they know anyone who smokes cigarettes? Do they smoke cigarettes? How much, how often, what have they tried to quit? Do their friends use any drugs? If so, which ones? Have they tried any drugs? Do their friends drink alcohol? Have they tried alcohol? How much, how often, ever to the point of blacking out or passing out? |
| D is also for depression: Ever been depressed? Ever to the point of wanting to hurt yourself? Have you tried to hurt yourself? Ever to the point of wishing you were dead? (passive suicidal ideation). Ever to the point of wanting to kill yourself? Have you specifically had a plan? Which plan(s)? Have you ever tried to kill yourself? Which ways? |
| Sex: Have you ever had sex? Are you sexually attracted to guys, girls, or both? Sexually, has anyone ever touched you in a way that made you uncomfortable? Have you ever had to swap sex for food, clothes, drugs, or shelter? |
The Gynecologic Examination Itself: The Rules
The genital examination of the child should be approached with special verbal acknowledgement to the child and parent before requesting the child to disrobe. With the younger child at preventive healthcare visits, the clinician can state that he/she will look at her bottom every year to make sure that everything is okay, reminding the child and parent that this part of the examination is an expected and routine part of every well-child visit. With younger children, it is useful to state, “It is okay if a doctor looks at your private parts with your mommy here, but it’s not okay if anyone else looks at your private parts without your mommy’s permission. If anyone ever did that, what would you do?” If the child does not respond, often the parent will chime in, “Oh, she knows about strangers, tell the doctor what you know.” Give positive feedback for whatever response the child gives, especially if the child states that she would tell mommy (and the doctor and the police).
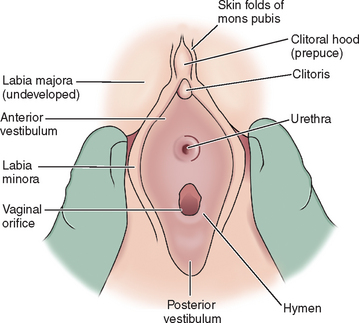
Parents often have misconceptions about the hymen. Before and during the examination, the clinician can teach the parents that hymens come in varying shapes and sizes, and that the examination will not harm or “break” the hymen in any way. Use of a diagram can help educate the parent or child about normal female anatomy and can help clear up any misconceptions (Figs. 13-1 and 13-2). Because not all clinicians routinely inspect genitalia despite national recommendations that it should be part of the annual examination, parental anxiety may set a tone for the child. The clinician can educate both parent and child while allaying anxiety and teaching parents to send calming cues to their child, helping reassure the child rather than raise anxiety. Occasionally, this may require more than one visit to complete a gynecologic examination.
Helping the Child Feel in Control
Attention to the little things can help a child feel in control. Rather than asking if the child wants to be in a gown, asking, “Do you prefer the green gown or the yellow one?” allows the child some autonomy in the process. The otoscope or hand lens can be used for magnification; allowing the child to look through the lens to see how it works can help put her at ease. If a colposcope will be used, letting the child view jewelry or fingers through the instrument and showing her how the light turns on and off can demystify the examination. Asking the older child if she prefers the parent in or out of the room can also help the child feel in control.
The child can also maintain control by being asked to assist in holding her labia apart. If the clinician acts relaxed and confident, the patient (and parent) will usually cooperate.3 An abrupt or hurried approach may lead to a child’s refusal to continue, so patience and a calm, confident tone are required. If a child needs more time, the examiner can leave the room until the patient feels ready. Several visits may be necessary to set the child at ease and build confidence that she will not be hurt. If an acute need for an examination exists, as in the case of vaginal bleeding, often an examination under anesthesia may be necessary.
The Actual Examination
Examination of the child with gynecologic complaints should include measuring height, weight (and body mass index if obese), performing a visual inspection from head to toe, including head, neck, heart, lungs, abdomen, Tanner staging (see Chapter 11), breasts (inspection and palpation for masses or discharge), and skin for rashes/lesions. A simple way to remember Tanner staging is as follows. For pubic hair, Tanner I means prepubertal, or no hair. Tanner II hair is fine and downy, and you can count them. Tanner III hair is coarse, in a triangular pattern, and you can count them if you are obsessive-compulsive! Tanner IV pubic hair means too many to count, and Tanner V means out to the thighs. For breast development, Tanner I means no bud yet, or prepubertal. Tanner II means just a breast bud under the nipple. Tanner III extends beyond the nipple, and Tanner IV is a mound of areola on top of a mound of breast. Tanner V refers to adult breasts, with the areola now flush with the breast but the nipple protruding.
Gynecologic assessment includes inspection of the external genitalia, palpation of the inguinal area for hernias or masses, and visualization of the vagina. Hymenal anatomy should be noted and documented in the medical record (see Figs. 13-1 and 13-2). Hymens come in different configurations, with many variants of “normal.” Hymens can be classified as crescentic or posterior rim, annular, or redundant.3,4 Recognition of an imperforate hymen before puberty is generally greatly appreciated by parents, so that anticipatory guidance can be given and an easy procedure accomplished before menstrual flow accumulates behind a blocked passageway. Cribriform or microperforate hymens and septate hymens can also be confusing to the untrained eye; pictures of each are seen in Figure 13-2. Further subtleties of the hymenal examination are addressed in the section Approach to the Child who Has Been Sexually Abused.
Often foreign bodies such as bits of toilet paper can be identified with the child in this position. A butterfly catheter of any size with the needle cut off can be attached to a tuberculin syringe with 1 μL of saline, and then placed inside a 12-inch red rubber bladder catheter to irrigate or wash off the genitalia.5 This catheter within a catheter can be squirted on the patient’s hand or thigh, so as not to surprise her, with explanation that it may feel cold and wet, allowing the area to be irrigated easily.
During the gynecologic examination, the clinician should note the presence of pubic hair, the size of the clitoris, hymenal configuration, signs of estrogenization of the vagina and hymen, and perineal hygiene.3 A clitoris larger than 10 mm in a pubertal girl is considered enlarged. The clitoris in the premenarchal child averages 3 mm in length and 3 mm in transverse diameter.6 If the hymen is viewed in lithotomy or frogleg position and likened to the face of a clock, irregular notching or transactions of the hymen between 5 and 7 o’clock are suggestive of sexual abuse, forced sexual intercourse, or trauma.
In the adolescent, inspection of the genitalia allows for identification of normal versus abnormal medical findings, including folliculitis or “razor burn” in patients who shave or use other means of hair removal (usually noninfectious). Candidal vulvovaginitis can also be seen and may be the first presenting sign of diabetes. In patients who present repeatedly with yeast vaginitis, a urinalysis can rule out diabetes, and a culture on bismuth sulfate (BiGGY) agar can determine whether Candida is the offending organism. Visual inspection allows the opportunity to educate the adolescent in tampon use and in proper hygiene techniques; it may also elicit questions that the teen may have been too embarrassed to ask about (e.g., clitoral size, irregularities in size or shape of labia). A “lump” felt by a teenager may be a Bartholin’s cyst rather than perceived cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree