■ The most important technical aspect of this anastomosis is establishing adequate mobilization of the remnant pancreatic body and tail. At least 3 cm is required, but greater mobilization is not discouraged provided it does not compromise perfusion.
■ A posterior, transverse gastrotomy is created. Attention to the size of the gastrotomy is paramount and should take the elastic nature of the stomach into consideration. The need to dilate the gastrotomy to accommodate the pancreatic remnant is a welcome finding.
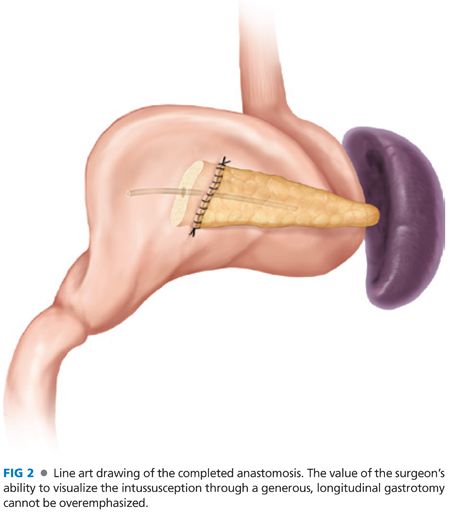
■ A generous longitudinal, anterior gastrotomy is performed directly opposite of the posterior gastrotomy to provide access to the lumen side of the PG. (Alternatively, the staple line from the antrectomy that will be used for a subsequent gastrojejunostomy is removed.)
■ The pancreaticogastric anastomosis is fashioned by taking full-thickness bites of the stomach to the pancreas.
■ Start at the most cranial aspect of the anastomosis. Work caudally, alternating between the posterior and anterior sutures so that the anastomosis is finished at the caudal aspect. This approach facilitates exposure to each subsequent bite without having to put undue tension on previously placed sutures.
■ Interrupted 3-0 silk sutures are used. Pass the needle through the pancreas tissue outside of the stomach lumen so that the needle can be retrieved on the extraluminal side. Then, pass the suture through the gastrotomy and then “back inside-out,” taking a full-thickness bite of the stomach wall.
■ Most experienced surgeons prefer to tag each suture; they will be tied after all sutures have been thrown.
■ Place the sutures circumferentially, spaced every 3 to 4 mm.
■ As the sutures are tied, the pancreas is invaginated into the lumen of the stomach.
■ The anterior gastrotomy is closed in two layers as classically described.
INVAGINATING PANCREATICOGASTROSTOMY
■ Aranha9 describes a one-layer invaginating PG after pancreaticoduodenectomy.
■ For this approach, the pancreatic remnant is mobilized for a distance of 4 cm.
■ As mentioned earlier, the size of the gastrotomy must accommodate stretching of the gastric wall, and an anterior longitudinal gastrotomy is created to provide exposure to the lumen.
■ Interrupted 3-0 silk sutures are placed.
■ The beauty of this technique is the visualization and simplicity. It is performed entirely while visualizing the luminal aspect of the anastomosis.
■ Begin inside the lumen of the stomach, taking a full-thickness bite. In one move, take a bite of pancreas, entering the exterior gland exiting in the transected edge that can be seen from the luminal side of the intended anastomosis.
■ The sutures are tied as they are placed; the end result is a mild invagination of the pancreas into the stomach (FIG 2).
DUCT TO MUCOSA
■ As an alternative PG, Telford and Mason10 have reported that direct anastomosis of the pancreatic duct to gastric mucosa provides better patency of the pancreatic duct as compared to a simple invagination procedure (FIG 3).
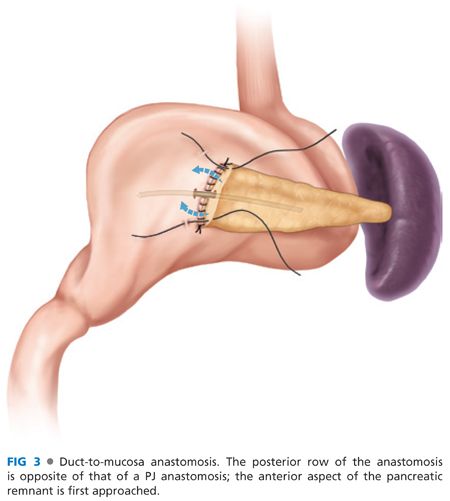
■ Initially, silk sutures are placed from the posterior, cephalad gastric wall to the anterior pancreas body. Importantly, this is contrary to PJ, where the posterior aspect of the pancreas is first addressed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








