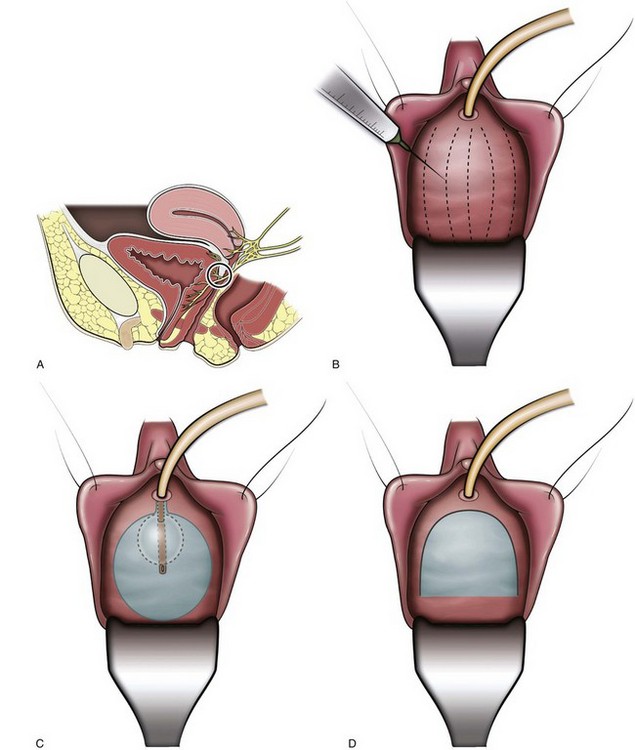
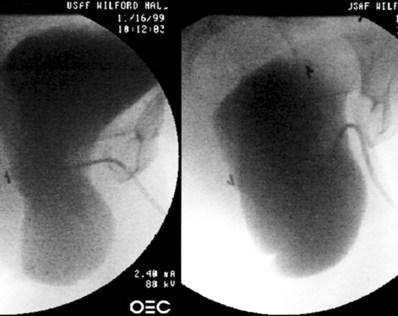
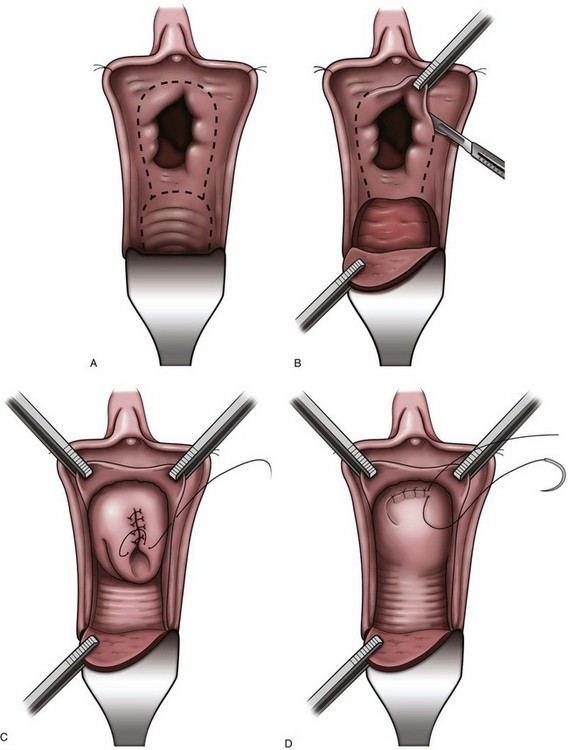
R. Duane Cespedes, MD, Jason L. Gerboc, DO The etiologies of voiding dysfunction are diverse and may occur as a result of neurologic, inflammatory, or infectious disorders. Other factors such as surgical or nonsurgical trauma and aging are also important causes. Obstruction continues to occupy a central role in the development of emptying failure and, when present chronically, may lead to poor bladder compliance and the failure to store. For both filling/storage and emptying disorders, dysfunction may originate primarily from the bladder, sphincter, or a combination of both. The majority of patients with voiding dysfunction will respond favorably to standard therapy (discussed elsewhere in this book). The treatment of complex cases should be individually tailored and may entail a combination of techniques, especially if approached through different mechanisms. Tables 61–3 and 61–4, list the numerous strategies devised to meet this goal, a testament to the complex management of voiding dysfunction. Additional treatments that have been developed for the management of storage and emptying failure are discussed in this chapter. Some of the topics are covered in other areas of this text but require special mention, while other topics are covered nowhere else in this edition. While some of these approaches offer promising results and are deserving of continued follow-up, others have been mentioned for historic reference only. Altering the innervation of the urinary tract is the focus of several strategies for the management of storage failure and is the central mechanism for procedures that vary from sacral rhizotomy to intravesical botulinum toxin. In addition, interventions may involve different levels of the nervous system, such as the spinal cord, nerve roots, or peripheral nerves. Of note, noncentral denervation proximal to the postganglionic neuron is properly termed “decentralization” and because the bladder is innervated by a short-neuron system, almost all denervation procedures outside the central nervous system that we will describe are properly referred to as decentralization. In general, more central procedures would appear more suitable for patients with spinal cord injury (SCI) or neurogenic detrusor overactivity, and although central denervation is theoretically very effective, it may also have a potentially wider range of unintended consequences. Peripheral decentralization is more selective for the bladder and more suitable for idiopathic detrusor overactivity, as other structures innervated by the sacral nerves remain neurologically intact (Madersbacher, 2000). There would seem to be only a small role for most of the procedures discussed in this section, because conservative measures are often sufficient in significantly improving or alleviating storage symptoms in most patients. Although favorable results have been reported with denervation techniques, some of these procedures have been accompanied by significant adverse outcomes that have limited their usefulness. One significant problem with central denervation and decentralization is that neuroplasticity often results in a variable restoration of neurologic function, with an even less desirable result than was present originally in many cases (Madersbacher, 2000). This section will focus on surgical techniques of bladder denervation, both central and peripheral. Sacral neuromodulation is covered in Chapter 70. Improvements in bladder storage function have been reported following intrathecal injection of neurolytic compounds (Misak et al, 1962; Gibbon, 1966). Urologic applications followed the observation that neurogenic detrusor overactivity was often converted acutely to areflexia in procedures performed primarily for somatic spasticity. The resultant flaccid bladder required clean intermittent catheterization or alternative methods to assist bladder emptying. The obvious disadvantage of this type of procedure is a lack of end-organ selectivity, with unintended motor or sensory loss to other organ systems. Impotence was a common sequela, and residual motor or sensory function was often significantly altered or lost. Further, an areflexic bladder was not always maintained on a long-term basis, and decreased compliance often developed in these patients, resulting in significant storage problems. Significant complications and relative long-term ineffectiveness have precluded continued use of this procedure. Several variations of sacral rhizotomy exist, however, the goals for all variations are to improve bladder capacity and compliance, abolish autonomic dysreflexia, and improve continence. Denervation may be achieved by sectioning anterior (motor), posterior (sensory), or both sacral roots, converting an overactive bladder into an areflexic one. These procedures are generally performed in association with lumbar or sacral laminectomy and involve the S2 through S5 nerve roots; however, newer, less invasive techniques, such as percutaneous radiofrequency rhizotomy and cryoneurolysis, have been described (Mulcahy et al, 1978; Awad et al, 1987). Typically, intraoperative electrostimulation of prospective nerve roots along with continuous urodynamic monitoring help identify appropriate nerves for transection. Significant side effects may develop following rhizotomy and may affect bladder, bowel, sphincter, sexual, and motor/sensory elements of the lower extremities. With this in mind, patient selection and informed consent is imperative. Meirowsky and colleagues (1950) were among the first to observe that SCI patients undergoing rhizotomy for severe somatic spasticity exhibited beneficial effects in bladder management. Subsequently, several reports followed on the use of anterior rhizotomy alone or in combination with posterior rhizotomy for the treatment of bladder hyperactivity (Misak et al, 1962). Initial studies reported increased bladder capacity with more efficient bladder emptying. Likely contributing to these findings was the reduction in urethral resistance, which often resulted from concomitant denervation of the external urinary sphincter (Rockswold et al, 1973). Unfortunately, bladder areflexia rarely persisted, and detrusor overactivity commonly recurred after a short time. Investigators also discovered that bilateral anterior and posterior rhizotomy, or conusectomy, adversely affected the rectum, anal and urethral sphincters, sexual function, and the lower extremities. In an attempt to reduce side effects, selective anterior (motor) rhizotomy was introduced with the hope of attaining a more specific response (Rockswold et al, 1973). To enhance clinical efficacy, differential sacral rhizotomy is typically preceded by stimulation and blockade of the individual sacral roots with cystometric and sphincterometric control. In this manner, only motor roots responsible for involuntary contractions are divided. The basis of this technique follows observations by Heimburger and associates (1948) that the anterior S3 nerve root is the dominant motor innervation of the human bladder. Torrens (1985) summarized the collective results of anterior rhizotomy reporting that success ranged from 48% for idiopathic detrusor overactivity to 81% for patients classified as having a “paraplegic bladder.” Unfortunately, the definition of “success” varied substantially among series and among patients. Clearly, when anterior rhizotomy procedures are performed, they should be preceded by urodynamic and urologic evaluation of the effects of selective nerve blocks before proceeding, especially in patients without fixed neurologic disease or injury. Even then, unintended effects on pelvic and lower extremity sensory or motor functions may occur, with disastrous medical and legal sequelae. The role, if any, of anterior rhizotomy procedures within a plan of treatment for detrusor overactivity, still remains to be defined. Expanded interest in dorsal (posterior) rhizotomy followed the realization of the importance of afferent stimuli in generating detrusor overactivity. Tanagho and Schmidt (1988), Tanagho and associates (1989), and Brindley (1990) further popularized the idea of sensory deafferentation using dorsal rhizotomy to increase bladder capacity. Similarly, dorsal root ganglionectomy has been reported to increase bladder capacity (McGuire and Savastano, 1984). Interruption of the afferent reflex arc by complete transection of all dorsal roots (sacral or sensory deafferentation) abolishes detrusor overactivity (Brindley, 1994b). Dorsal rhizotomy may also restore continence and may decrease the incidence of autonomic dysreflexia in many instances (Schurch et al, 1998). In addition, striated sphincter dyssynergia is often abolished without altering resting tone (Brindley, 1994a). Madersbacher (2000) stated that deafferentation of the bladder is best achieved using an intradural approach because in this location, motor and sensory fibers can easily be separated. If an intradural procedure is not possible, he believes that a deafferentation at the level of the conus medullaris should then be performed. Proper patient selection is paramount in selecting patients for this procedure because dorsal rhizotomy of the S2 through S5 nerve roots abolishes reflex erections, reflex ejaculation, and sacral sensation, and it can reduce reflex defecation. Partial or selective procedures should be considered only in patients who retain some sensation or have excellent reflex erections that they wish to preserve. Selective dorsal rhizotomy of only a few nerve roots is not as effective as procedures that transect all dorsal roots from S2 to S5, because the former procedure often results in incompletely blocked reflex impulses and persistent detrusor overactivity (Sauerwein, 1990). Complete and long-term resolution of detrusor overactivity has been attained with complete sensory deafferentation (Madersbacher, 2000; Kutzenberger et al, 2005). Koldewijn and associates (1994) reported on the effects of intradural bilateral posterior root rhizotomies from S2 to S5 with implantation of an anterior root stimulator in a group of patients with suprasacral SCI. All showed persistent detrusor areflexia afterward, although two required subsequent secondary rhizotomy at the level of the conus. Madersbacher (2000) treated 65 tetraplegic or paraplegic patients with post-SCI reflex urinary incontinence resistant to all other means of conservative treatment. Continence was achieved in 90% of these patients. Complete deafferentation produces detrusor areflexia that requires clean intermittent catheterization (CIC) or alternative methods to empty the bladder. Insertion of an anterior root stimulator, to electrically induce voiding, is often performed concurrently with dorsal rhizotomy procedures (Seif et al, 2004). A significant potential shortcoming of anterior root stimulation is simultaneous, unphysiologic contraction of the bladder and urethral sphincter, which may result in clinically significant detrusor sphincter dyssynergia (DSD) or increased intravesical pressures during voiding (Schumacher et al, 1999). Anterior root stimulators may also be used to induce erections. Patient satisfaction rates following combined sacral deafferentation and anterior root stimulation has been reported to be very high (Kutzenberger et al, 2005). For more on anterior nerve root stimulation and related procedures, see Chapter 70. Sacral neuromodulation is currently the most commonly used surgical procedure to treat patients with refractory urgency-frequency or urgency incontinence. For more information on the indications, procedural aspects, treatment results, and complications of sacral neuromodulation, see Chapter 70. Regarding the literature on transvaginal denervation, in many articles, there is little description of what “success” actually means. In addition, there are few studies with long-term follow-up, and “postoperative assessment” often means a few months of follow-up. A comprehensive summary of the surgical treatment of detrusor overactivity by peripheral denervation was reported by Mundy in 1985; however, many reports have been published since that time. Transvaginal partial denervation of the bladder was originally described by Ingelman-Sunberg in 1959. The original procedure, which was an extensive denervation, was used mostly for the treatment of refractory urge-urinary incontinence, and in the originator’s hands, success rates of up to 80% were achieved. Mundy (1985) reported that other investigators found success in 50% to 65% of cases, and Torrens (1985) noted that “the technique has not found favor with other workers.” More recently, Cespedes and associates (1996) described McGuire’s modification (limited lateral vaginal dissections) of the Ingelman-Sundberg procedure in 25 women with urinary urgency incontinence and detrusor overactivity who had failed behavioral and medical therapy (Fig. 75–1). Transvaginal local anesthesia was used as a test to determine which patients would benefit from the procedure, with significant improvement of urgency symptoms considered a positive test. Twenty-five patients were found to have a positive test; the number of patients unsuccessfully tested was not reported. Sixteen (64%) of these patients were cured of urgency incontinence at a mean follow-up of 14.8 months. Of the 16 patients cured, 9 patients required one medication, and 2 required two medications. Madersbacher (2000) comments that a follow-up period of 15 months is too short to determine long-term effects. Long-term follow-up was reported by Westney and associates (2002), who retrospectively reviewed 28 patients with refractory urgency incontinence, having undergone the modified procedure with a mean follow-up of 44.1 months. Of these, 68% were cured (54%) or improved (14%). Based on these results and the prior series, the authors concluded that the modified Ingelman-Sundberg procedure is an efficacious, minimally invasive option for this difficult-to-treat patient population. These procedures are seldom used today and are fully discussed on the Expert Consult website. Bladder transection involves a complete circumferential division of the full thickness of the bladder wall at a level just above the ureteric orifices, although Mundy (1985) believed that only the posterior part of the transection was important. Initial encouraging reports in the early 1970s were followed by longer-term reviews of larger series, all reporting success rates in excess of 50% for at least detrusor overactivity, using varying criteria. Mundy (1985) reviewed his large experience with transection in patients with detrusor instability and reported that of 104 patients with a follow-up for 1 to 5 years, 74% were cured, 14% were improved, and 12% were failures. Between 20 and 32 months, 10% of the group initially judged to have a satisfactory response suffered a relapse, giving a long-term subjective success rate of 65%. Only 35% of those who claimed to be symptomatically cured reverted to urodynamically stable detrusor behavior, however. Crooks and colleagues (1995) reported on the results of open bladder transection in 12 patients with urinary frequency and nocturia unresponsive to more conservative measures. Three patients were cured, 7 were better, and 2 had failures. Interestingly, 6 patients with preoperative enuresis were cured of at least this symptom by the procedure. Parsons and coworkers (1984) described endoscopic bladder transection in patients with phasic detrusor hyperactivity. Their early results were encouraging, but Lucas and Thomas (1987) reported essentially no change in 14 of 18 patients with intractable detrusor overactivity treated by this technique. Two achieved complete symptomatic relief, and 2 more were rendered continent but with the complaint of urgency and nocturia. Hasan and associates (1995) reported on the results of endoscopic bladder transection in 50 patients with urinary frequency, urgency, and urgency incontinence refractory to anticholinergic therapy. Subjective assessment revealed an overall symptomatic improvement in 12%, while objective urodynamic analysis demonstrated no significant improvement. Overall, it is unclear whether bladder transection is a viable procedure for patients with a refractory overactive bladder (OAB); however, if attempted, open transection appears to be superior to endoscopic transection. Chemical neurolysis has been used in an attempt to reproduce the results of the surgical approaches outlined above but in a minimally invasive manner. Mundy (1985) and Torrens (1985) credit the original technique, using transvesical infiltration of the pelvic plexus with phenol, to Ewing and colleagues (1983), who reported successful treatment of 19 of 24 patients with multiple sclerosis (MS). The potential risks of this procedure were found to be urinary retention and vaginal fistula. Blackford and associates (1984) reported a satisfactory response in 82% of women with refractory neurogenic detrusor overactivity and in 69% of women with detrusor overactivity who were more than 55 years old, but in only 14% of females younger than 55 years old. Cameron-Strange and Millard (1988) reported a 70% success rate in 11 patients with neurogenic detrusor overactivity secondary to MS. Although they achieved a 58% success rate in 29 patients with detrusor overactivity, Wall and Stanton (1989) reported only a 29% significant response rate to therapy in a mixed group of 28 females with urinary urgency incontinence. Chapple and coworkers (1991) reported success in only 2 of 18 patients with idiopathic detrusor overactivity, who were observed for 6 months, and in 2 of 6 with neurogenic detrusor overactivity. Two fistulas resulted, one vesicoureterovaginal and one vesicovaginal. They concluded, on reviewing their results and those of others, that subtrigonal phenol should be used in such cases only when no other treatment is possible. One of the more recent innovations is the use of botulinum toxin to chemically denervate the detrusor musculature. Originally used in spinal cord injury patients to denervate the external sphincter, it has recently found much success in patients with refractory overactive bladder. The exact mechanism and the site within the nervous system by which botulinum toxin exerts its effects is largely unknown. A further discussion of the possible mechanisms and site of action at which botulinum toxin exerts its effects is covered in Chapter 60, and its clinical use in the management of detrusor overactivity is covered in Chapter 68. The use of acupuncture as a therapeutic treatment modality is described in Chinese medical texts as early as 300 BC. Acupuncture is a form of somatic sensory stimulation using a variety of procedures that involve stimulation of specific anatomical locations by insertion of thin, solid, metallic needles into the skin. In the classic forms of acupuncture, needles are stimulated manually to achieve the desired effects. In more modern forms of acupuncture, heat or electrical stimulation may be provided by the addition of an energy source or be performed needleless, as in laser acupuncture. Indeed, McGuire and coworkers’ (1983) developed transcutaneous posterior tibial nerve stimulation for bladder inhibition that was based on the acupuncture points. The use of acupuncture has been described for a number of urologic symptoms, including urinary urgency, frequency, incontinence, nonobstructive urinary retention, enuresis, and neurogenic detrusor overactivity. Acupuncture is generally a well-tolerated procedure, and although side effects are generally uncommon and minimal in nature, treatment may occasionally result in localized pain, hematoma, infection, and even organ puncture. Several treatment sessions are usually required. There has been much interest in determining the mechanism by which acupuncture exerts its beneficial effects. According to traditional Chinese medicine, concepts such as the meridian system, circulation of Qi, and other related theories remain difficult to define and characterize. Sato (1997) has shown somatovisceral reflexes evoked from somatic afferent stimulation may induce either excitatory or inhibitory changes in bladder function and sphincter activity. Bergström and associates (2000) hypothesized any one or a combination of (1) endorphinergic effects at the sacral spinal cord level or above, (2) inhibitory somatovisceral reflexes, and (3) increase in peripheral circulation as possible mechanisms of action. The true nature of how acupuncture exerts its beneficial effects remains incompletely understood. Bergström and associates (2000) reported on the results of classic acupuncture performed twice weekly in a group of 15 elderly women with urgency or mixed incontinence. In this open, uncontrolled study, subjective assessments of improvement and objective measurements in the form of grams of leakage over 48 hours were encouraging, not only at the end of the study but also after 1 and 3 months. More recently, Emmons and Otto (2005) compared acupuncture versus placebo acupuncture in the treatment of women with overactive bladder and urinary urgency incontinence. The number of incontinent episodes decreased by 59% in the treatment group compared with 40% in the placebo group. The treatment group had a significant improvement in bladder capacity, urgency, frequency, and quality-of-life scores compared with the placebo group. Initially described by Helmstein in 1972 for the treatment of patients with bladder carcinoma, this treatment modality has undergone several modifications. Bladder overdistention, most familiar for its use in the treatment of interstitial cystitis (see Chapter 12), has also been used for other diverse indications, including nocturnal enuresis, irritative symptoms following radiation or BCG, and for patients with overactive bladder. No standard technique has been clearly defined for this procedure and, as such, several variations exist. Bladder distention may be performed under regional or general anesthesia. The bladder is then distended by either a balloon catheter or more commonly by saline infused cystoscopically or through a urethral catheter. The ideal pressure and duration needed to distend the bladder has not been well defined. Dunn and colleagues (1974) described prolonged bladder distention of several hours at a pressure equal to the patients’ systolic blood pressure. At this pressure, therapeutic benefit is thought to derive from ischemic changes induced in submucosal afferent nerve endings and stretch receptors (Dunn et al, 1977). In a primarily interstitial cystitis population, Hanno and Wein (1991) described distending the bladder to 80 cm H2O for several minutes with good results. Bladder rupture, historically as high as 5% to 10%, is the most significant complication after bladder distention therapy. Other possible complications include hematuria, back pain, and urinary retention. Ramsden and colleagues (1976) reported good to excellent results in the treatment of patients with detrusor overactivity, while most others have reported inferior results with this treatment modality. In this same patient population, Jorgensen and coworkers (1985) reported a success rate of only 1 in 15 (6%) patients. In a retrospective review by Taub and Stein (1994), 8 of 22 (36%) of patients with frequency and urgency of various etiologies had subjective improvement, while no patient with detrusor overactivity improved. They also demonstrated that short duration distention therapy (15 to 30 minutes) was as efficacious as prolonged therapy (6 hours). Lloyd and colleagues (1992) reported that only 6 of 29 women with severe irritative symptoms, including 6 patients with interstitial cystitis and none with neurogenic detrusor overactivity, had a good response to treatment. In a study of 26 women with frequency and urgency, Liapis and associates (2001) found a statistically significant increase in bladder capacity after treatment; however, only 4 (15%) had any improvement in symptoms beyond 9 months. Although largely regarded as an ineffective procedure in patients with storage failure secondary to neurogenic detrusor overactivity, bladder overdistention may provide substantial, but usually temporary, improvement to some patients with non-neurogenic storage symptoms who have failed medical therapy. Key Points: Storage Failure Due to Bladder Overactivity, Decreased Compliance, or Hypersensitivity See the Expert Consult website for a discussion of this topic, as well as Figures 75-2 and 75-3. Key Points: Storage Failure Due to Sphincter Underactivity Urethral compression devices have been used to successfully control urinary incontinence in males for over 250 years, with little change in their construction during this time. Indeed, the Heister penile clamp was described in Institutiones Chirurgicale, a surgical textbook published in 1750. This device closely resembles the Cunningham clamp, a device commonly used today (Madjar et al, 2001). These devices are primarily used to treat patients with pure sphincteric incontinence, most commonly postprostatectomy incontinence (PPI), because normal bladder capacity and storage pressures are a relative requirement. Continence is achieved by mechanically compressing the urethra between two foam pads. The device is adjusted by slowly increasing the level of compression until continence is attained, because this allows the lowest pressure to be applied, keeping obstruction of blood flow to a minimum. Regardless, these devices should be unclamped regularly at 3- to 4-hour intervals, because prolonged or excessive compression can cause pressure-related injury to the penis. Additionally, these devices should not be worn during an erection or while sleeping. Pressure-related injuries may also be more prevalent in patients with impaired sensation or cognition; therefore penile clamp usage in this population should be considered a relative contraindication. Several other compression devices are available and are similar in both design and function to the Cunningham clamp. Moore and colleagues (2004) reported efficacy, comfort, and patient satisfaction with three penile compression devices: the Cunningham clamp, the C3, and the U-Tex. The study population included 12 men with postprostatectomy incontinence requiring continuous pad protection. Over 4 consecutive days, patients were randomly assigned to use either one of the three devices, or pads alone as a control group. Each group wore the device or pads continuously for 4 hours (maximum time recommended for continuous usage), and pad weights were obtained before and after the study period to quantify leakage. Additionally, patients were asked to complete a questionnaire at the conclusion of the study. Urine leakage was significantly reduced by all three devices evaluated; however, the Cunningham clamp was the most efficient of the three devices tested, reducing urine leakage by nearly 85%. The Cunningham clamp was also noted to reduce cavernosal blood flow significantly more than the other devices. Overall, patients rated the Cunningham clamp the most acceptable and preferable of the devices evaluated. The renewed interest in conservative management of female sphincteric incontinence, and lower urinary tract symptoms associated with pelvic organ prolapse, has prompted the development and investigation of several nonsurgical devices. Unfortunately, due to the location and anatomy of the female urethra, no compressive or occluding device has been introduced that successfully treats sphincteric incontinence without causing significant side effects or patient discomfort. In addition, reliable external urinary collection devices do not exist for females, making the Foley catheter the most common method of treatment for intractable sphincteric incontinence. Therefore the role of these devices in the algorithm of conservative management of female sphincteric incontinence remains unclear. A more thorough description of these devices, along with the indications and efficacy, are discussed in Chapter 69. Injection therapy is commonly employed as a minimally invasive treatment option for male and female stress incontinence. Although it is theoretically a temporary treatment, typically lasting only 6 to 12 months, the ease of reinjection in a clinical setting renders it a potentially permanent solution in selected patients. Injectables treat stress incontinence by increasing the abdominal leak point pressure by several mechanisms, including increased mucosal sealing pressure and improvement in the mucosal seal mechanism (Appell, 2002). Females most likely to benefit from this procedure have intrinsic sphincter deficiency (ISD), a normally contractile bladder, and a well-supported urethra. This constellation of requirements is most commonly fulfilled by elderly females; however, several authors have demonstrated improvement in younger patients with stress urinary incontinence (SUI) due primarily to urethral hypermobility (Appell, 2009). The rarity of injectable use in this population really reflects the efficacy and widespread use of the newer minimally invasive slings, compared with the relative ineffectiveness of injectables. In males, postprostatectomy incontinence can also be managed with injection therapy. The best results are obtained with patients with mild incontinence (one to three pads per day), while patients who have undergone radiation, bladder neck incision, or cryotherapy have less favorable responses (Cespedes, 2000). Most patients require four to five injections, with reinjections every 6 to 12 months to maintain dryness (Cespedes, 2000). Westney and colleagues (2005) reported their results of collagen injection in 322 men with ISD after therapy for prostate carcinoma or benign prostatic hyperplasia. The authors reported that after a mean of 4.37 injections, and irrespective of therapy, overall improvement was approximately 50% with a mean duration of 6 months. The ideal bulking agent should be durable, biocompatible, should not migrate, or cause significant inflammatory reaction at the injection site. Unfortunately, no current injectable has all of these qualities. In the future, advances in the field of tissue engineering, including autologous chondrocytes and cultured myoblasts, may offer new and exciting options in the treatment of stress urinary incontinence using injectables. For a more thorough discussion of the history, indications, techniques, and results of bulking procedures, including a review of the injectable agents currently available, refer to Chapter 77. Vesicourethral suspension procedures, such as the Burch and MMK (Marshall-Marchetti-Krantz) procedures, have been successfully used for many years to treat stress incontinence secondary to urethral hypermobility, most commonly defined as stress incontinence occurring with an abdominal leak point pressure (ALPP) greater than 100 cm H2O. More recently, with the increasing popularity of the minimally invasive mesh slings, their use has diminished substantially, and they are rarely used unless a simultaneous abdominal procedure, such as a hysterectomy or abdominal sacral colpopexy, is planned. In addition, the Burch colposuspension was recently shown to be inferior to the autologous pubovaginal sling in a randomized, controlled study (Albo et al, 2007). Although vaginal prolapse does not, per se, cause urinary continence, a deficiency of vaginal support is shared by both conditions. Therefore, urinary incontinence secondary to hypermobility would imply that vaginal prolapse, especially the anterior wall, likely coexists and should be repaired at the same time. Severe vaginal wall prolapse has also been associated with occult urinary incontinence, defined as stress incontinence that only occurs with reduction of the prolapse. Patients with severe vaginal prolapse, with or without complaints of incontinence, should be carefully assessed preoperatively by reduction of the prolapse during the stress incontinence evaluation (see Fig. 75–2). This condition and additional descriptions of these procedures are further discussed in Chapters 71 and 72. Autologous fascia pubovaginal slings, popularized by McGuire in the 1980s, were originally used for female patients with poor sphincteric function. Historically, female patients with stress incontinence have been divided into groups based on etiologies of either urethral hypermobility or intrinsic sphincter deficiency (ISD). It has become clearer over time that almost all patients leak due to a combination of hypermobility and intrinsic sphincter deficiency, with each component of incontinence on a continuum. Using this logic, a sling would be the ideal treatment because it successfully corrects both urethral hypermobility and ISD. More recently, pubovaginal slings have been supplanted by a wide variety of minimally invasive tension-free mesh sling procedures. These procedures, although less invasive, have never shown success rates superior to the 90% cure rate of the original pubovaginal slings, which are still considered by most to be the gold standard therapy. Autologous or cadaveric fascial slings are still commonly used in situations where the sling must be pulled more tightly, as with the obstructing slings sometimes used in patients with neurogenic incontinence. Theoretically, mesh slings are “tension- free” slings and therefore would be much more likely to erode into the urethra if pulled tightly. In cases where mesh is preferred, a “spiral” or “circumferential” sling, which wraps completely around the urethra, can be used; however, this requires a urethrolysis to gain access to the retropubic space and passage of the needles from the abdomen to the opposite side of the vagina to gain circumferential compression. This procedure and many others are more fully described in Chapter 73. The introduction by Scott and coworkers (1974) of the artificial urinary sphincter (AUS) signified a major advancement in the treatment of sphincter-related incontinence. The AUS has been successfully used in the management of stress incontinence of various etiologies and can be implanted in adults and children of both sexes. Postprostatectomy incontinence remains the most common indication for AUS insertion, with female patients accounting for only 1% of the patients in whom the devices are implanted yearly, typically for neurogenic disease (Lee et al, 2009). Although the AUS is commonly used in patients with neurogenic incontinence, it is important to remember that because of the ability of the AUS to greatly increase outlet resistance, social continence may be gained at the expense of renal deterioration in patients with poor detrusor compliance. In general, storage pressures and bladder capacities should be normalized prior to placement of an AUS. For treatment of PPI, the AUS has been quite successful and remains the gold standard therapy. Nevertheless, revisions may be necessary due to atrophy, infections, erosions, or mechanical problems. In addition, some patients are reluctant to have the AUS placed for a variety of reasons, including the desire to “void normally” without having to manipulate a device. More recently, the male sling has had a resurgence of popularity in the search for a minimally invasive, efficacious, “natural voiding” alternative to treat PPI. The male sling is a passively obstructive device that appears to function by increasing the urethral closure pressure and functional sphincteric length, thereby augmenting existing sphincteric function. This may be why it does not work as well in patients with severe sphincteric incontinence. Male slings are easily placed using a perineal approach and can be fixated using either bone anchors (into the inferior pubic ramus) or a transobturator approach. Although slings are more commonly used in patients with mild to moderate PPI, and the AUS with more severe PPI, high rates of continence and patient satisfaction have been reported using both the male sling and AUS in properly selected patients (Rajpurkar et al, 2005; Gallagher et al, 2007). A more thorough and in-depth discussion of the male sling and artificial urinary sphincter are covered in Chapter 79. Complete closure of the bladder neck is rarely necessary, because a compressive bladder neck sling is more easily performed, is less morbid, and allows transurethral access if necessary. The main indication for bladder outlet closure is urethral destruction secondary to prolonged catheter drainage in neurogenic bladder patients. The clinical course is typically a progressive worsening of leakage around the catheter, requiring progressively larger-bore catheters and larger volumes of fluid in the balloon, ultimately resulting in a dilated, nonfunctional urethra and bladder neck. It is thought that a long-term Foley catheter and balloon can cause pressure necrosis and bladder neck erosion, especially in the setting of recurrent bladder spasms. In these patients, an obstructing sling or AUS is rarely feasible. For patients with some residual normal urethra, Chancellor and colleagues (1994a) reported on the use of a combined “tight” autologous pubovaginal sling and lower urinary tract reconstruction in 14 female patients with urethras destroyed by long-term Foley use. At 24 months, they reported excellent results with minimal incontinence or other complications. They concluded that at least 1 cm of normal urethra was required for proper functioning of the sling. For patients without residual normal urethra, management options include transvaginal, transabdominal, or combined closure of the bladder neck with simultaneous continent or incontinent urinary diversion, incontinent ileovesicostomy, or suprapubic catheter placement. Feneley (1963) reported on 24 female patients with neurologic disease who underwent transvaginal bladder neck closure and suprapubic tube placement. Overall results were good; however, a vesicovaginal fistula developed in 4 patients, resulting in persistent incontinence. Zimmern and associates (1985) reported on 6 female patients using a transvaginal closure. At 21 months of follow-up, all patients were cured with no fistulas or incontinence reported. Levy and colleagues (1994) reported a 40% success rate using a transvaginal bladder neck closure. They subsequently modified the approach, using a combined transvaginal-transabdominal approach, and reported a 100% success rate at a mean 16-month follow-up for the subsequent 10 patients. Shpall and Ginsberg (2004) reported on 39 patients who underwent a combined transabdominal bladder neck closure and various continent and incontinent diversions. At a mean of 37 months, 6 patients (15%) developed fistulas; however, 4 patients were successfully repaired, for an overall 95% cure rate. Most recently, O’Connor and colleagues (2005) reported on 35 patients with a mean 79-month follow-up who underwent a transabdominal bladder neck closure for refractory incontinence. They were initially successful in 28 (83%) patients with an overall 94% cure rate after one revision. As illustrated in this historical perspective, the risk of complications, specifically a vesicovaginal fistula, is relatively common and can be difficult to repair. It is important to remember that a bladder neck closure is much more difficult than a simple closure of the bladder wall. The bladder neck is usually hyperactive in patients with neurologic disease, and every voiding reflex includes active opening and closing of the bladder neck, which forcibly attempts to destroy the bladder neck closure. To reduce this risk, postoperative suppression of the voiding reflex using prolonged continuous catheter drainage (3 weeks) and liberal use of anticholinergics is imperative. In addition, to reduce the risk of fistula, the repair must be watertight from the beginning, and this requires a precise mucosal closure using a running suture and multiple additional layers of muscle to reinforce the strength of the repair (see Fig. 75–3). Lastly, a drain should be used to minimize fistula formation should suture line leakage occur. When performed correctly, a bladder neck closure with simultaneous lower urinary tract reconstruction remains an excellent treatment option in those patients with a destroyed bladder neck or urethra. Sphincteric incontinence with a fixed, nonvolitional, open bladder outlet may be congenital or acquired. In most cases, the sphincteric musculature is insufficient and denervated and therefore does not provide sufficient closure pressure to prevent incontinence. Techniques have been developed that concentrate on increasing urethral resistance by either tightening or lengthening the urethral segment, such as the Kropp and Pippi-Salle procedures (see Chapter 129) or by constructing a mechanism more similar to the native sphincter. In 1919, Hugh Hampton Young first described a technique to reconstruct the bladder outlet to improve sphincteric continence. Originally, the procedure included resecting a portion of bladder neck and reconstructing the bladder outlet with constricting sutures to effectively narrow its caliber. This technique was further modified by Dees (1949) and Leadbetter (1964). In theory, circularly arranged muscle fibers located in close proximity to the bladder neck are used to re-create a functional, tubularized neourethra that replicates the outlet resistance of a normal sphincteric outlet, but with variable volitional control. The Leadbetter modification involves proximal reimplantation of the ureters to allow more extensive tubularization of the trigone and, theoretically, improved outlet resistance. The construction of this neourethra may be formed from tissue of the anterior bladder neck as described by Tanagho (1981), or from the posterior surface of the bladder wall and trigone, according to any of the variations of the Young-Dees-Leadbetter technique. Leadbetter (1985) reported long-term success rates of 60% to 70% in 34 patients; however, the exact definition of success in this paper is unclear. Clinically, these procedures are most useful for patients with a good-capacity, acontractile bladder and who are mentally and physically able to perform CIC on a regular basis. In addition, care should be taken in the setting of poor bladder compliance or significant detrusor overactivity, because these patients commonly need bladder augmentation. For further discussion regarding the original technique described by Young, and its several variations, refer to Chapters 124 and 129. The Holy Grail for sphincteric incontinence may well be the replacement of the dysfunctional sphincter with a new, functional native replacement. The first attempt at this type of sphincteric replacement was a skeletal muscle transposition reported by Deming (1926). He used unstimulated gracilis muscle wrapped around the urethra, which reportedly did improve sphincteric continence; however, the unstimulated skeletal muscle required the patient to voluntarily contract (adduct) the leg for prolonged periods to provide outlet resistance. Additional problems with the use of unstimulated graciloplasty include (1) poor sustainability of the contraction due to the fast twitch, non–fatigue-resistant fibers of the gracilis, (2) high passive resistance resulting in urethral obstruction, (3) postsurgical changes resulting in the loss of resting tension and reduced contractility, (4) the potential for fibrosis due to segmental vascularization (Stenzl, 1998). The next improvement in functional sphincteric replacement was the development of external stimulation of the gracilis using implanted electrodes (Janknegt et al, 1995). They developed an electrical stimulation program that was able to transform fatigable type 2 skeletal muscle fibers to the slow type I fibers that were able to sustain a long-lasting contraction. This early report described three patients who achieved “good results” and one patient who became dry at night. Two years later, Chancellor and colleagues (1997) reported their series using a gracilis urethral wrap in five men with neurogenic bladder dysfunction and severe sphincteric stress incontinence. The procedure was considered successful in four patients; however, three required CIC, and two of these patients had persistent stress incontinence. The shortcomings of using the gracilis was noted by Stenzl (1998), who commented that the electrically stimulated gracilis muscle was an improvement over the unstimulated muscle; however, the bulky musculature and propensity for stricture formation caused an inherent passive obstruction. This shortcoming was scientifically overcome by Palacio and coworkers (1998) in an animal model using a free but innervated flap of well-vascularized proximal gracilis muscle in female dogs. The smaller size of the graft allowed it to be more easily transposed around the urethra while stimulation of the sphincter was carried out using the graft’s own motor innervation. Unfortunately, this apparently successful animal model has never been reported in a human clinical study. The most recent twist in an attempt to improve the function of a neurologically damaged sphincter includes injecting allogenic muscle–derived progenitor cells (MDPC) directly into the sphincter (Cannon et al, 2003). The authors used a rat model in which the urethra was mechanically denervated and subsequently injected with MDPCs, which dramatically improved the fast-twitch muscle contraction amplitude from 8.8% to 87% (compared with normal amplitude). Although promising, this innovative and minimally invasive option for sphincteric incontinence has not yet been proven in follow-up human clinical studies. Key Points: Lower Urinary Tract Reconstruction, Diversion, and Bladder Substitution
Decreasing Spasticity and Increasing Cystometric Capacity
Lower Urinary Tract Denervation, Decentralization, and Neuromodulation
Central (Subarachnoid) Block
Chemical Rhizolysis—Intrathecal Injection of Alcohol/Phenol
Nerve Root Procedures
Sacral Rhizotomy and Conusectomy
Selective Anterior Sacral Rhizotomy
Dorsal Rhizotomy
Sacral Neuromodulation
Peripheral, Perivesical, and Intravesical Bladder Denervation
Transvaginal Denervation
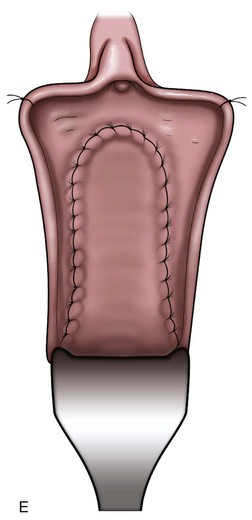
Bladder Transection and Peripheral Chemical Neurolysis
![]()
Chemical Neurolysis
Intravesical Botulinum Toxin Injections
Acupuncture
Bladder Distention Therapy
Increasing Outlet Resistance
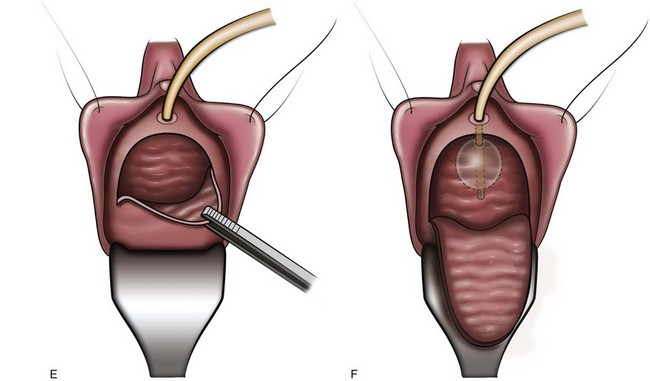
![]()
Nonsurgical Compressive and Occlusive Devices
Sphincteric Injection Therapy
Surgical Compression/Closure of the Bladder Outlet
Vesicourethral Suspension and Prolapse Repair (Female)
Pubovaginal Slings and Tension-Free Tape Procedures
Artificial Urinary Sphincter and Male Perineal Sling
Closure of the Bladder Outlet
Bladder Outlet Reconstruction
Myoplasty for Functional Sphincter Reconstruction
Lower Urinary Tract Reconstruction, Diversion, and Bladder Substitution
![]() See the Expert Consult website for a discussion of the topic.
See the Expert Consult website for a discussion of the topic.
Other Therapies for Storage and Emptying Failure
• Adequate capacity, low detrusor storage pressures, continence, and the absence of involuntary bladder contractions are the goals of managing storage failure.
• Urethral compression devices are primarily used to treat patients with pure sphincteric incontinence, most commonly postprostatectomy incontinence (PPI). Normal bladder capacity and storage pressures are a relative requirement. Pressure-related injuries may occur with these devices and may be more prevalent in patients with impaired sensation or cognition.
• Bladder augmentation offers the best chance to construct a “normal” urinary system, but the ability to void without catheterization is not guaranteed; therefore, only patients who have the ability and motivation to perform CIC should be considered for this procedure.