Fig. 1
Candida esophagitis: there are multiple, plaque-like lesions of varying size in the mid esophagus. Note how the lesions have discrete margins and are separated by normal, intervening mucosa. These findings are characteristic of candidiasis
Drug-Induced Esophagitis
Drug-induced esophagitis is caused by various oral medications, including tetracycline, doxycyline, potassium chloride, quinidine, alendronate, and nonsteroidal antiinflammatory drugs (NSAIDs) [6]. These patients often have a history of ingesting the pills with little or no water immediately before retiring. As a result, the pills tend to lodge in the mid esophagus, where it is compressed by the aortic arch or left main bronchus. This can result in a focal contact esophagitis, manifested by a focal cluster of small, discrete ulcers in the mid esophagus [6]. Affected individuals may present with severe odynophagia, but there is usually rapid clinical improvement after withdrawal of the offending agent.
Eosinophilic Esophagitis
Eosinophilic esophagitis usually occurs in young men with long-standing dysphagia and occasional food impactions. Affected patients may have an atopic history, asthma, or peripheral eosinophilia. Barium esophagography may reveal a ringed esophagus, with distinctive ringlike indentations, or a small-caliber esophagus, with diffuse loss of distensibility of the thoracic esophagus in the absence of a discrete stricture (Fig. 2) [7, 8]. The diagnosis can by confirmed by endoscopic biopsies showing >20 eosinophils per high-powered field. These patients often have a dramatic response to treatment with oral steroids or inhaled steroid preparations.


Fig. 2
Small-caliber esophagus in eosinophilic esophagitis. There is diffuse loss of distensibility of the entire thoracic esophagus, which has a smooth, uniform contour. This young man with long-standing dysphagia and asthma had proven eosinophilic esophagitis
Esophageal Carcinoma
Early esophageal cancer (EEC) is typically manifested on double-contrast studies by small, polypoid or plaque-like lesions [9]. Other patients may have superficial, spreading carcinomas with a focal cluster of poorly defined nodules and plaques that merge one with another, producing a coalescent area of disease [9]. EEC is rarely diagnosed in Western countries, because most patients develop symptoms only after the tumor has invaded the mediastinum [9]. In contrast, advanced cancers typically appear as polypoid, ulcerated, or infiltrating lesions with irregular luminal narrowing and shelf-like margins [9]. Rarely, esophageal cancers may be varicoid lesions that simulate varices due to submucosal spread of tumor.
Whereas squamous cell carcinomas tend to be located in the upper or mid esophagus, adenocarcinomas are mainly located in the distal esophagus and have a marked tendency to invade the gastric cardia and fundus. At one time, esophageal adenocarcinomas were thought to be rare lesions, because these tumors, when invading the proximal stomach, were erroneously classified as primary gastric carcinomas invading the distal esophagus. However, adenocarcinomas are now thought to constitute as many as 50% of all esophageal cancers [9], so this is a more common malignant tumor than previously recognized.
Stomach
Erosive Gastritis
Erosive gastritis is usually characterized on double-contrast studies by varioliform erosions seen as punctate or slit-like collections of barium surrounded by radiolucent halos of edematous mucosa. Varioliform erosions tend to be located in the gastric antrum and are often aligned on the crests of the folds. NSAIDs are by far the most common cause of erosive gastritis, accounting for >50% of cases. Occasionally, NSAID-induced erosive gastritis may also be manifested by distinctive linear or serpiginous erosions that tend to be clustered in the gastric antrum or body or near the greater curvature [10]. These erosions are thought to result from localized mucosal injury as the dissolving NSAID tablets collect by gravity in the dependent portion of the stomach. Detection of this finding should therefore lead to careful patient questioning regarding a recent history of NSAID use, and if confirmed, the offending medication should be withdrawn.
Helicobacter Pylori Gastritis
Helicobacter pylori gastritis can be diagnosed on barium studies by the presence of thickened folds in the antrum, body, or, less commonly, fundus of the stomach [11] (Fig. 3). Other patients with H. pylori may show a polypoid form of gastritis characterized by grossly thickened, lobulated folds, mimicking the appearance of Menetrier’s disease, lymphoma, or even a submucosally infiltrating adenocarcinoma [11]. Endoscopy and biopsy are therefore required for a definitive diagnosis.
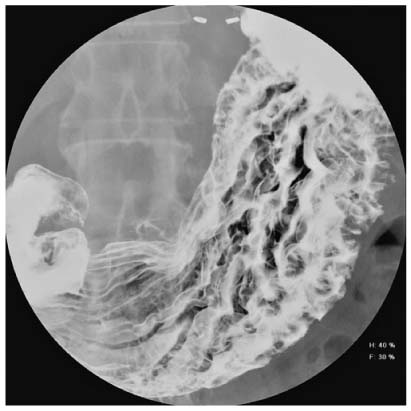
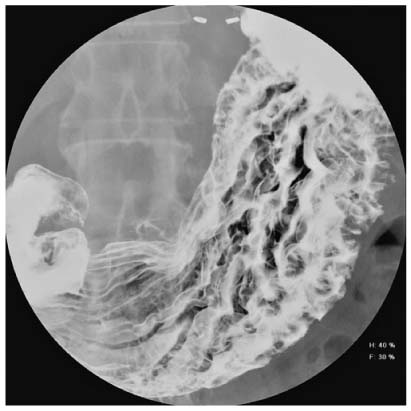
Fig. 3




Helicobacter pylori gastritis. There are considerably thickened folds in the body of the stomach due to chronic H. pylori gastritis. More than 90% of all patients with thickened folds in the stomach are found to have this infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








