Fig. 1 a–3
Magnetic resonance imaging (MRI) follow-up study in a 35-year-old man with chronic hepatitis B virus (HBV) infection. A massive presence of dysplastic nodules is seen within the liver parenchyma. By analyzing a T1- and b T2-weighted baseline and c, d dynamic study, none of the nodules shows characteristic feature that may suggest progression to malignancy. On e hepatobiliary acquisition, no nodule shows signs of biliary impairment
Hepatocellular Carcinoma: Imaging Findings
Actually, the main important clue suggesting the diagnosis of HCC within cirrhosis is the identification of a typical vascular supply of the nodule, characterized by contrast-agent washin during the arterial phase and washout on the portal venous or late phase. However, a typical vascular behavior at dynamic imaging modalities is not present in the 30% of HCC [5]. In these cases, baseline and postcontrast MRI, especially after administration of hepatospecific contrast media, may lead to a definitive diagnosis of HCC. On baseline T1-WI, HCC usually appears as a hypointense nodule because of its increased cellularity, and thus its higher amount of intracellular water, whereas on baseline T2-WI, HCC usually shows mild signal hyperintensity [2]. Well differentiated HCC might not show these signal intensities on baseline sequences, resulting examination, resulting isointense on T2-WI. Although their application has not yet been introduced into diagnostic guidelines, the use of tissuespecific contrast agents may give additional information, especially in the presence of borderline lesions (DNs) or well-differentiated HCCs. Regarding hepatobiliary contrast agents, the lack of contrast uptake is strongly related to overt HCC due to the loss of normal metabolic function, whereas uptake is preserved in early HCCs, resembling that of HGDN [6]. In daily practice, the advantages of the most recent generation of MRI contrast media can be exploited, as they illustrate the nodule’s characteristic vascular and hepatospecific phases, i.e., neoangiogenesis and lack of hepatobiliary function, respectively, which allow a highly confident diagnosis of malignancy (Fig. 2).
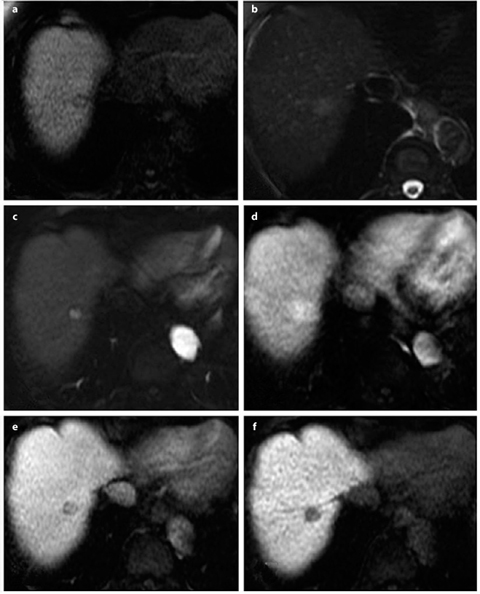
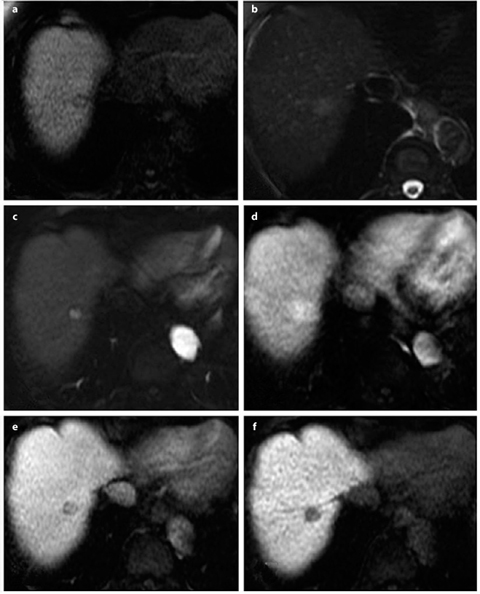
Fig. 2 a–f
Typical hepatocellular carcinoma (HCC) in a 77-year-old woman with chronic hepatitis C virus (HCV) infection. At magnetic resonance imaging (MRI), a baseline T1-weighted imaging (WI) shows the presence of a hypointense nodule of segment VII, which appears clearly hyperintense on b T2-WI. After gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA) administration, the nodule shows washin during the c early arterial phase that persists during the d parenchymal arterial phase and clear washout on the e delayed phase. f On hepatobiliary acquisition, the lesion appears hypointense because of complete loss of biliary activity of de-differentiated hepatocytes
Therapy and Follow-up
Nowadays, the advantages of imaging-guided treatments have enlarged the therapeutic approaches of cirrhotic patients with HCC, permitting a tailored therapeutic strategy on the basis clinical and functional data and on patient staging [7]. Despite transplantation represents the best therapeutic approach for a cirrhotic patient, miniinvasive treatments, such as percutaneous ablation with radiofrequency or microwave, are actually considered a good alternative to resection. Intravascular procedures, such as chemoembolization, should instead be applied in intermediate patients with good performance status, as a palliative treatment, and in patients on waiting list for transplantation, in order to down stage those exceeding Milan’s criteria [8]. Radioembolization is the newly introduced intravascular approach, reserved for patients with good performance status with large, locally advanced HCC, also involving a portal branch; this therapy permits downstaging patients otherwise classified as intermediate, who can then benefit from subsequent therapeutic approaches [9].
Peripheral Cholangiocellular Carcinoma
Peripheral intrahepatic cholangiocellular carcinoma (IHCCC) arises from cholangiocytes of the second order of intrahepatic biliary ducts and represents 10% of all CCC; it generally occurs in the elderly (70s and 80s) and more frequently affects men than women [10]. The vast majority (95%) of these tumors are represented by adenocarcinomas. Well known risk factors for developing such neoplasm are primary sclerosing cholangitis or other chronic conditions, such as hepatolithiasis, bile stenosis, congenital hepatic fibrosis, and recurrence of biliary inflammations [11]. In recent years, moreover, the evidence of a number of concomitant chronic hepatitis C virus (HCV) infections associated with IHCCC suggests that the virus might play a role in the development of biliary neoplasm due to the common precursor (oval cell) of hepatocytes and cholangiocytes [12].
IHCCC Classification and Prognosis
According to the Liver Cancer Study Group of Japan consensus [13], IHCCC are classified on the basis of macroscopic appearance and growth characteristics into three distinct forms: (1) mass-forming type; (2) periductal infiltrating type; (3) intraductal growing type. Different prognoses are related to different types: if the mass-forming and periductal infiltrating types usually have a poor prognosis, intraductal growing types might successfully benefit from surgery. As for the majority of pathological conditions, in cases of IHCCC, imaging modalities play a key role in lesion detection and characterization.
Mass-Forming IHCCC
Mass-forming IHCCC appears at US as a solitary macro-nodule within liver parenchyma; echogenicity strictly depends on lesion dimension, as lesions <3 cm tend to be hypoechoic, whereas larger neoplasms can appear as slightly hyperechoic, mainly because of the large fibrous component. At multidetector CT (MDCT) examination, the lesion appears as a solitary mass or a main lesion with irregular margins, sometime surrounded by satellite nodules, appearing as a hypodense area associated with capsular retraction; dynamic study often reveals a thin rim of enhancement at the periphery of the neoplasm; on the arterial phase, whereas the central portion of the mass usually shows as hypodense, as it is constituted by fibrotic and necrotic areas. On delayed images, the slight enhancement of the fibrous component is detectable: such finding, together with the aforementioned capsule retraction and dilatation of the intrahepatic ducts located peripherally to the lesion, represent the most reliable elements for a confident diagnosis of IHCCC (Fig. 3). MRI shows a typically hypo/ isointense mass on baseline T1-WI and slightly inhomogeneously hyperintense on baseline T2-WI, depending on the hydration of fibrous tissue and mucinous components within the lesion [14]. On the hepatobiliary phase acquired after administration of hepatospecific contrast agents, the lesion appears as hypointense in respect to the surrounding parenchyma because of the lack of functioning hepatocytes.


Fig. 3 a–c
Peripheral mass-forming cholangiocarcinoma in a 55-year-old man. On the a arterial phase, it is possible to appreciate a massforming lesion within the dome of the liver that shows a rim like, peripheral enhancement; on b portal venous and c late phases, slight enhancement of some central portions of the lesion are appreciable. Capsular retraction of the lateral margin of segment VII is evident in all phases, as is the marginal, millimetric calcification
Periductal Infiltrating IHCCC
Periductal infiltrating IHCCC generally arise in the proximity of the hilum, thus sometimes leading to a difficult differential diagnosis from hilar primitive neoplasm (Klatskin tumor). US often shows dilation of the intrahepatic bile ducts located above the obstruction, and a hypoechoic lesion, located near the hepatic hilum, with irregular margins and mural thickening.
At MDCT, the lesion is not clearly defined, showing a slight enhancement mainly in the late phase. Portal vein branches are not frequently involved. MR cholangiopancreatography (MRCP) is largely applied in staging the neoplasm, as it can excellently and noninvasively evaluate obstructed ducts, the presence of material within them, and irregularity of duct walls, providing another clue to support the diagnosis [15].
Intraductal Growing IHCCC
Intraductal growing IHCCC presents at US as a variable dilatation of peripheral biliary ducts, usually involving an entire segment. In some ducts, and especially the more dilated ones, a single or multiple and slightly hyperechoic papillary projection might be appreciable. At MDCT, a subsegmental or segmental dilatation of peripheral biliary ducts is the major clue for suggesting this form. No clear intrahepatic mass is usually appreciable; capsular retraction is usually depicted, as well as atrophy of the involved segment. At dynamic MDCT, papillary lesions might show as slightly enhancing masses within the dilated ducts on portal venous/late phases [16]. MR may provide additional information for correct diagnosis and staging. In particular, at MRCP, it is possible to detect the presence of papillary projections within the dilated ducts, as they appear as hypointense filling defects within the bright lumen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








