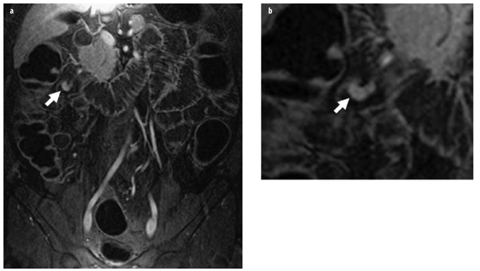
Fig. 1 a, b
Active Crohn’s disease: magnetic resonance (MR) enteroclysis. a T2-weighted axial single-shot turbo spin-echo (SSH-TSE) and b T1-weighted postgadolinium (Gd) contrast gradient echo (GRE) with fat saturation following biphasic intraluminal contrast administration (methylcellulose). A segment of small bowel in the right lower quadrant demonstrates significant wall thickening and submucosal edema, indicated by a hyperintense layer within the intestinal wall (a arrow). There is marked transmural enhancement of the respective loop with even peri-intestinal involvement (b arrow). These signs are indicators of active Crohn’s disease
Early and Mild Stages
Early and mild stages of CD may present at MRI with subtle findings, such as a focal or regional disruption of the fold pattern with mildly or no increased enhancement. Superficial erosions may not be detected at all given the limited spatial resolution of MRI. In contrast to overt wall thickening and stenosis, these lesions can easily be missed on MRI, especially when distension is suboptimal. This is why MR enteroclysis compared with capsule endoscopy or invasive double-balloon endoscopy reaches an overall sensitivity of only 75–80% [13, 14]. In subacute CD and under effective treatment, wall thickening may persist initially but decreases over time. The hyperintense signal intensity from submucosal edema disappears and turns into intermediate signal intensity. Likewise, formerly increased contrast enhancement decreases.
Another important asset in MRI for assessing inflammatory bowel disease is the recent experience with diffusion weighted imaging (DWI). Preliminary data suggest that DWI and the derived quantitative apparent diffusion coefficient (ADC) demonstrate good correlation with standards of reference to detect active CD, specifically gadolinium enhancement [15]. DWI is also helpful in diagnosing internal fistula and abscess [16]. The use of DWI might be specifically beneficial in pediatric patients, in whom avoiding the use of gadolinium must be considered [17].
Fibrostenosing Type
Fibrostenotic lesions are less conspicuous and more difficult to identify on MRI, as they typically show no wall thickening or abnormally increased enhancement. The seemingly normal wall thickness and contrast enhancement in fibrostenosis mimic normal bowel wall. Low signal intensity on T2-weighted images with and without fat suppression reflects fibrosis but is difficult to quantify [9]. Persistent focal and fixed circumscript intestinal stenosis and marked prestenotic dilatation are the most conspicuous and reliable indicators and indirect signs of fibrous strictures.
Fistulizing Type
Internal and external fistula and peri-/extramural abscesses represent the most severe complications of CD. They can be accurately diagnosed with MRI (92%). Fistulas are tubular inflammatory pathways between bowel loops, bowel and other hollow organs, or bowel and the abdominal wall. They are defined as internal fistulas (IF) when between bowel loops (enteroenteric) or to internal hollow organs (e.g., enterovesical). External fistulas (EF) are those that abut the skin (enterocutaneous or perianal). A vast majority of IF may remain asymptomatic or cause nonspecific symptoms, especially if located in distal bowel segments. Complex IF typically involve multiple bowel loops [18]; they are most frequently associated with bowel stenosis and symptoms of obstruction. Abnormal tubular tracts within the mesentery containing air or fluid are highly indicative of IF and are well depicted on steady-state free precession (SSFP), e.g., true fast imaging with steady-state precession (true-FISP) imaging. The outlines of IF show intermediate signal intensity on T2-weighted images, similar to the intestinal wall, and may show moderate enhancement after intravenous administration of gadolinium. For complex IF, a somewhat stellate arrangement of the bowel loops (star sign) is characteristic and has been described as a strong indicator for the presence of IF (Fig. 2) [19]. The inflamed bowel loops converge to a common center, which is often the origin of abscess formation. Urinary bladder involvement is likely when there is marked thickening of the bladder wall in the vicinity of an inflamed bowel segment [18]. A contiguous inflammatory tract between inflamed bowel and bladder wall may not always be seen.
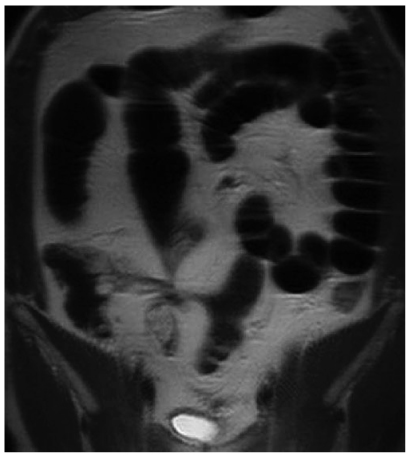
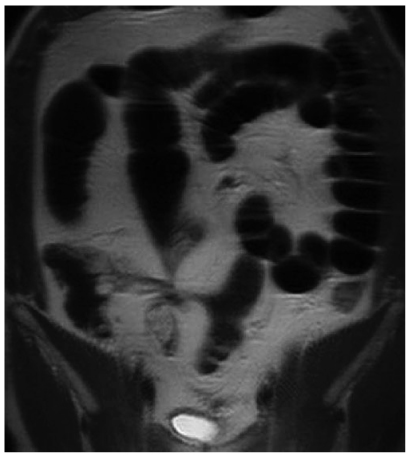
Fig. 2
Internal fistula in Crohn’s disease: Magnetic resonance (MR) enteroclysis following negative intraluminal contrast application (Lumirem, Guerbet, France). Note stellate configuration of bowel loops in the right lower quadrant with segment stenosis; most loops demonstrate prestenotic dilatation. This configuration is characteristic and strongly predicts the presence of an internal fistula complex: enteroenteric fistula in Crohn’s disease
Differential Diagnosis of Crohn’s Disease
Although less frequently a reason for imaging than CD, infectious enteritis is an important differential diagnosis to consider. Infectious enteritis is typically of bacterial origin, such as Enterococcus, Salmonella, Yersinia, tuberculous bacilli, and others. In immunocompromised patients, viral and fungal infections, such as cytomegalovirus (CMV), must be considered. Following bone marrow transplant, CMV and graft-versus-host disease (GVHD) are likely. Infectious enteritis presents with nonspecific findings on CT or MRI, with the main and most common feature being submucosal edema. For tuberculosis, mesenteric lymphadenopathy is a major finding and a helpful diagnostic indicator. Ischemic bowel disease is to be considered if arteriosclerosis and vascular obstruction is additionally observed.
Small-Bowel Neoplasms
Small-bowel neoplasms are rare and account for <5% of all GI tumors. The most frequent tumor entities are adenocarcinoma, carcinoid, lymphoma, GIST, and metastases. MR enteroclysis is an effective diagnostic tool for detecting small-bowel tumors, with sensitivity, specificity, and accuracy of 86%, 98%, and 97%, respectively [20]. Small-bowel cancer incidence has risen in the past 30 years, with the greatest increase being in carcinoid tumors. Adenocarcinoma is the most common among intestinal malignant neoplasms, followed by carcinoid tumors. Following the duodenum, the jejunum is the second most common location for adenocarcinoma and typically involves the ileum. Imaging morphology for adenocarcinoma and lymphoma (Fig. 3) follows the previously described patterns (see “Duodenal Neoplasms”). Both malignancy types may complicate CD.
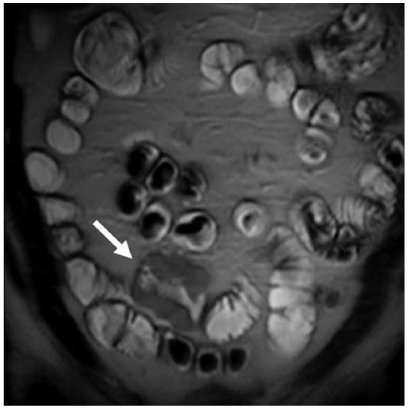
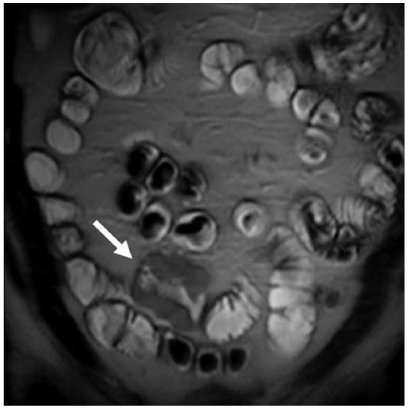
Fig. 3
Small-bowel lymphoma: magnetic resonance (MR) enteroclysis following biphasic intraluminal contrast application (methylcellulose). T2-weighted single-shot turbo spin-echo (SSH-TSE) images in coronal plane demonstrate appropriate filing of all smallbowel loops. A short segment with marked thickening of the smallbowel wall is noted in the lower quadrants to the right of the midline (arrow). Intermediate signal intensity is similar to that of the bowel wall. Note that the lumen is preserved despite significant wall thickening. Also, there is no prestenotic dilatation. This appearance is characteristic of small-bowel lymphoma
NET: Carcinoid
Carcinoid tumors are neuroendocrine neoplasms and constitute approximately 2% of all GI tumors. They may be found along the entire GI tract (85%), in the pancreas, and in the lung (10%). The appendix (50%) and the ileum (~0%) are the most common primary locations. Up to 30% of intestinal carcinoids are multifocal. Carcinoids have a tendency to metastasize early to lymph nodes and liver, even when they only are 1–2 cm in size [21]. Therefore, distension of the bowel lumen in MR enteroclysis is required for better detection. Carcinoids are typically hypervascularized and therefore are best identified on contrast-enhanced T1-weighted fat-saturated gradient echo (GRE) sequences (Fig. 4). Single-shot fast spinecho (SS-FSE) and SSFP sequence types depict these tumors less effectively as slightly hyperintense or isointense to muscle and bowel wall. Approximately one half of them appear as a nodular intraluminal mass, one third as focal wall circumferential thickening, and 20% with both characteristics [22]. If only wall thickening is present, they may easily be confounded with inflammatory disease. Desmoplastic reaction in the adjacent mesentery occurs in up to 73% of cases and can cause vascular engorgement.