Fig. 1 a–c
Diffuse fatty liver. A 41-year-old woman presenting with epigastric pain. a Axial contrast-enhanced computed tomography image demonstrates diffuse low attenuation of the liver without displacement of the hepatic vessels. b In-phase and c out-of-phase T1-weighted images show significant signal drop in the liver on the out-of-phase images. Reproduced from Hodler J, von Schulthess GK, Zollikofer ChL (Eds) (2010) Diseases of the Abdomen and Pelvis 2010–2013. Springer-Verlag Italia, Milan, pp. 56–60
Hepatic fatty change is, however, not always uniform, but it can present as a focal area of steatosis in an otherwise normal liver (focal steatosis) or as subtotal fatty change with sparing of certain areas (focal sparing). On imaging, several features allow accurate identification of focal fatty change or focal spared areas: (1) the typical periligamentous and periportal location, (2) lack of mass effect, (3) sharply angulated boundaries of the area, (4) nonspherical shape, (5) absence of vascular displacement or distortion, and (6) lobar or segmental distribution.
Iron Overload
Iron overload states are categorized in hemochromatosis, where the iron accumulates preferentially within hepatocytes, and in hemosiderosis, where it is deposited in the Kupffer cells.
Primary Hemochromatosis
Hereditary or primary hemochromatosis is an autosomal recessive disorder of iron metabolism characterized by abnormal absorption of iron from the gut with subsequent excessive deposition into hepatocytes, pancreatic acinar cells, myocardium, joints, endocrine glands, and skin. In addition, reticuloendothelial system (RES) cells in patients with primary hemochromatosis are abnormal and unable to store processed iron effectively. As a consequence, patients with primary hemochromatosis do not accumulate iron into the RES. Clinical findings of cirrhosis and its complications [portal hypertension, development of hepatocellular carcinoma (HCC)] predominate in patients with long-lasting disease.
On CT, excessive storage of iron into hepatocytes will result in an overall increased density. However, this CT appearance of a hyperdense liver is nonspecific, as similar features can be seen with gold deposition and in Wilson’s disease, type IV glycogen storage disease, and following amiodarone administration. Performing noncontrast CT in patients with suspected hemochromatosis is important because excessive iron cannot be detected in the setting of enhancing parenchyma.
MRI is far more specific than any other imaging modality for characterizing iron overload due to the magnetic susceptibility effect of iron. The superparamagnetic effect of accumulated iron in hepatocytes results in significant reduction of signal intensity on T2-weighted images. Comparison of liver signal intensity with that of paraspinal muscles provides a useful internal control. HCCs, complicating 35% of patients with advanced hemochromatosis, are usually easily detected on both T1- and T2-weighted images due to the background of decreased liver signal intensity.
Hemosiderosis
In patients with hemosiderosis or siderosis, due to either transfusional iron overload states or dyserythropoiesis (e.g., thalassemia major, sideroblastic anemia, pyruvate kinase deficiency, chronic liver disease), the excessive iron is processed and accumulates in organs containing reticuloendothelial cells, including liver, spleen, and bone marrow.
On CT, there is diffuse, increased attenuation of liver and spleen (Fig. 2). On MRI, the extrahepatic signal intensity changes in the spleen and bone marrow distinguish primary hemochromatosis from hemosiderosis. Although in general the clinical significance of transfusional iron overload states is negligible, patients with chronic hemosiderosis can develop symptoms similar to those of the primary form, as well as cirrhosis and HCC.
Fig. 2
Hemosiderosis. A 45-year-old woman with long history of sickle cell anemia requiring multiple transfusions. Axial non-enhanced computed tomography image demonstrates increased attenuation of the liver. Reproduced from Hodler J, von Schulthess GK, Zollikofer ChL (Eds) (2010) Diseases of the Abdomen and Pelvis 2010–2013. Springer-Verlag Italia, Milan, pp. 56–60
Wilson Disease
Wilson disease, also known as hepatolenticular degeneration, is a rare autosomal recessive abnormality of copper metabolism characterized by accumulation of toxic levels of copper in the brain, cornea (Kayser-Fleischer rings), and liver, the latter being due to impaired biliary excretion. Hepatic deposition of copper, predominantly seen in periportal areas and along the hepatic sinusoids, evokes an inflammatory reaction resulting in acute hepatitis with fatty change. Subsequently, chronic hepatitis may result in liver fibrosis and eventually macronodular cirrhosis.
Due to copper’s high atomic number, a hyperdense liver may be seen on unenhanced CT scans. However, this finding is not universally present, and usually only nonspecific signs such as hepatomegaly, fatty change, and — in advanced cases — cirrhosis are observed. During the early stage of the disease, due to ionic copper paramagnetism, MRI can be valuable by demonstrating focal copper depositions as multiple nodular lesions, typically appearing hyperintense and hypointense on T1-and T2-weighted images, respectively, as described by Cheon et al.
Amyloidosis
Amyloidosis consists of deposition of fibrils of protein-mucopolysaccharide complexes throughout the body and is classified based on the biochemical composition of the amyloid fibrils. Primary amyloidosis is due to the deposition of immunoglobin light chains and is associated with multiple myeloma and monoclonal gammopathy. Secondary amyloidosis is due to deposition of amyloid A protein and is associated with chronic infection, rheumatoid arthritis, and malignancies. Exceeded only by the spleen and kidney, the liver is the third most common solid organ prone to this deposition.
Hepatic amyloidosis has a nonspecific imaging appearance. The most common finding is diffuse hepatomegaly. CT sporadically demonstrates focal areas of low attenuation within the liver, corresponding to sites of amyloid deposition (amyloid pseudotumor). Patients may present with a picture of jaundice, which is due to intrahepatic cholestasis.
Neoplastic Diseases
Metastatic Disease
Neoplastic infiltration due to diffuse metastatic disease can occur with many primary tumors. Melanoma, malignant neuroendocrine tumors, pancreatic adenocarcinoma, breast carcinoma, and colonic adenocarcinoma are some of the more commonly encountered causes of diffuse hepatic metastatic disease.
CT appearances of hepatic metastases depend on lesion vascularity compared with normal liver parenchyma. Diffuse metastatic involvement may produce only subtle imaging findings and be only detectable through indirect features, such as diffuse parenchymal heterogeneity, vascular and architectural distortion, or alterations of the liver contour. The latter, particularly seen in patients with treated breast cancer metastases, has been reported as the pseudocirrhosis sign (Fig. 3). In addition, treated breast cancer metastases may mimic the appearance of liver hemangiomata.
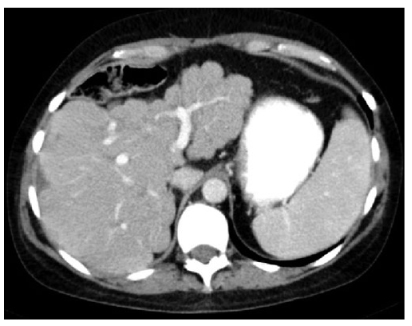
Fig. 3
Diffuse metastatic breast cancer (pseudocirrhosis pattern). A 43-year old woman treated for metastatic breast cancer. Axial contrast- enhanced computed tomography image demonstrate several small, low-density lesions in the liver and a nodular contour of the liver due to hepatic capsular retraction. Reproduced from Hodler J, von Schulthess GK, Zollikofer ChL (Eds) (2010) Diseases of the Abdomen and Pelvis 2010-2013. Springer-Verlag Italia, Milano, pp. 56–60
Lymphoma
Lymphoma can infiltrate the liver both primarily and secondarily. Primary lymphoma of the liver is extremely rare. Conversely, the liver is often secondarily involved in both Hodgkin’s and non-Hodgkin’s lymphoma. Typically, the liver parenchyma is diffusely infiltrated with microscopic nests of neoplastic cells, without significant architectural distortion, and therefore, lymphomatous involvement is difficult to detect by imaging alone. Associated abnormalities, such as splenomegaly and lymphadenopathy, may narrow the differential diagnosis.
Diffuse Infectious and Inflammatory Diseases
Fungal Infections
Hepatosplenic fungal infection is a clinical manifestation of disseminated fungal disease in patients with hematologic malignancies or compromise of the immunologic system. The reported prevalence of fungal dissemination ranges from 20% to 40%. Most hepatic fungal micro – abscesses occur in leukemia patients and are caused by Candida albicans.
Candidiasis
C. albicans in the liver may evoke little or no inflammatory reaction, cause a superlative response, or occasionally produce granulomas. The typical histologic pattern of hepatic candidiasis is characterized by microabscesses, with the yeast or pseudohyphal forms of the fungus in the center of the lesion and a surrounding area of necrosis and polymorphonuclear infiltrate.
At contrast-enhanced CT, fungal microabscesses usually appear as multiple round, discrete areas of low attenuation, generally ranging from 2 to 20 mm (Fig. 4). These microabscesses usually enhance centrally after intravenous administration of contrast medium, although peripheral enhancement may occur.
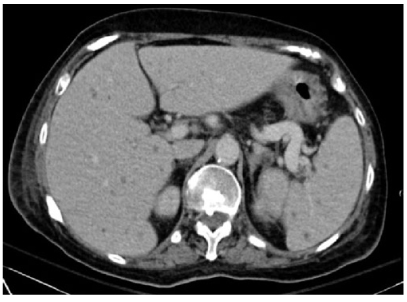
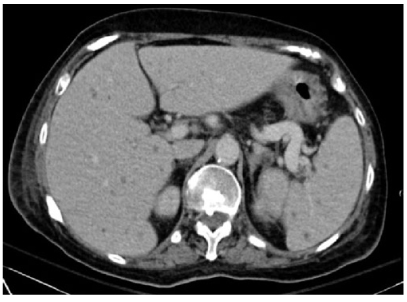
Fig. 4
Hepatic candidiasis. A 66-year-old woman with leukemia presenting with abnormal liver function tests. Axial contrastenhanced computed tomography image demonstrates multiple small, low-attenuation lesions seen throughout the liver and spleen. Splenomegaly and bilateral pleural effusions are also present. Reproduced from Hodler J, von Schulthess GK, Zollikofer ChL (Eds) (2010) Diseases of the Abdomen and Pelvis 2010–2013. Springer-Verlag Italia, Milan, pp. 56–60
At MRI, the untreated nodules are rounded lesions <1 cm in diameter, are minimally hypointense on T1-weighted and gadolinium-enhanced images, and are markedly hyperintense on T2-weighted images. After treatment, lesions appear mildly to moderately hyperintense on T1- and T2-weighted images and demonstrate enhancement on gadolinium-enhanced images. A dark ring is usually seen around these lesions with all sequences. Completely treated lesions are minimally hypointense on T1-weighted images, isointense to mildly hyperintense on T2-weighted images, moderately hypointense on early gadolinium-enhanced images, and minimally hypointense on delayed gadolinium-enhanced images. MRI is superior to CT and US for detecting these fungal foci.
Granulomatous Diseases
Granulomatous hepatitis is associated with a wide variety of conditions, most commonly with sarcoidosis, tuberculosis, and histoplasmosis. Hepatic granulomas usually appear as discrete, sharply defined nodules consisting of aggregates of epithelioid cells by a rim of mononuclear cells, predominantly lymphocytes.
Sarcoidosis
Sarcoidosis is a multisystem disorder of unknown pathogenesis characterized by noncaseating granulomas. Although it may involve almost any organ in the body, pulmonary sarcoidosis is most common. Sarcoidosis of the liver is also relatively frequently seen, but the granulomas are usually not macroscopically detectable and thus may not produce focal abnormalities on imaging studies. Classically, the granulomas develop in a periportal location, resulting in periportal fibrosis, cirrhosis, and eventually portal hypertension.
Hepatic contrast-enhanced CT may typically reveal multiple, diffuse, small, low-density areas in both liver and spleen. MRI features of hepatic sarcoidosis are also nonspecific and include organomegaly, multiple lowsignal- intensity lesions relative to background parenchyma with all sequences, increased periportal signal, irregularity of portal and hepatic vein branches, and patchy areas of heterogeneous signal. Literature reports by Semelka et al. confirm the nonspecific appearance but describes large central regenerative nodules and wedge-shaped areas of peripheral parenchymal atrophy as characteristic features.
Tuberculosis
Tuberculosis (TB) is one of the most common infectious diseases worldwide. Generally, tuberculosis in the liver presents as either miliary or focal form. Focal hepatic TB is further subdivided into nodular (i.e., tuberculous abscess and tuberculoma) and tubular or hepatobiliary tuberculosis (i.e., tuberculosis involving intrahepatic ducts). Hepatic miliary TB is most common and is reported to occur in 50–80% of all patients with terminal pulmonary TB. Miliary TB is usually not detected by imaging. Hepatomegaly may be the only radiological abnormality.
In the healing stage of TB, CT may show diffuse hepatic calcifications (~50% of cases). Reported CT findings of nodular TB are nonspecific and include hypo-attenuating lesions both before and after intravenous application of contrast administration.
At MRI, lesions are hypointense on T1-weighted and hypo- to isointense on T2-weighted images. TB lesions differently enhance after gadolinium administration. Because of these rather nonspecific findings with all imaging techniques, percutaneous liver biopsy is necessary.
Histoplasmosis
Histoplasmosis is the most common cause of fungal infection in the Ohio River Valley of the United States; 99% of patients exposed to histoplasmosis develop only subclinical infections. Liver involvement is common in disseminated histoplasmosis, which usually originates in the lungs. The most common hepatic findings include portal lymphohistiocytotic inflammation, and discrete, well-delineated granulomas. In patients with healed histoplasmosis, the presence of small, punctate calcifications scattered throughout the liver and spleen is a typical but nonspecific finding.
Parasitic Infections
Schistosomiasis
Schistosoma japonicum, S. hematobium, and S. mansoni are the three most important species that infect humans. These organisms live in the bowel lumen and lay eggs in the mesenteric veins. The eggs may then embolize to the portal vein. The eggs themselves do not survive and subsequently calcify. Chronic infections with either S. japonicum or S. mansoni result in formation of cirrhosis and the risk of HCC development. Histologically, schistosomiasis is characterized by white, pinhead-sized granulomas scattered throughout the liver. At the center of each granuloma is a schistosome egg. In severe infections, the surface of the liver shows granulomatous involvement and widespread fibrous portal enlargement (pipe-stem fibrosis).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








