10 Obliterative Procedures for Pelvic Organ Prolapse
Le Fort Partial Colpocleisis
A Le Fort partial colpocleisis is an option if the patient has her uterus and is no longer sexually active. Because the uterus is retained, evaluating any future uterine bleeding or cervical pathologic abnormalities is difficult. Therefore endovaginal ultrasound, endometrial biopsy, and Papanicolaou smear (Pap smear) must be performed before surgery. (Denehy et al, 1995) The ideal candidate for such a procedure is the patient who has complete uterine procidentia with symmetric eversion of the anterior and posterior vaginal walls (Figure 10-1).
Case 1: Le Fort Partial Colpocleisis
 View: Video 10-1
View: Video 10-1
Procedural Steps
1. The procedure is begun by placing the cervix on traction to evert the vagina. The vaginal mucosa is injected with 0.025% bupivacaine or 2% Lidocaine with 1 : 200,000 epinephrine just below the vaginal epithelium. A Foley catheter with a 5- to 10-ml balloon is placed in the bladder for identification of the bladder neck.
2. The areas that are to be denuded are marked anteriorly and posteriorly. The area should extend from approximately 2 cm from the tip of the cervix to 4 to 5 cm below the external urethral meatus. A mirror image on the posterior aspect of the cervix and vagina are also identified.
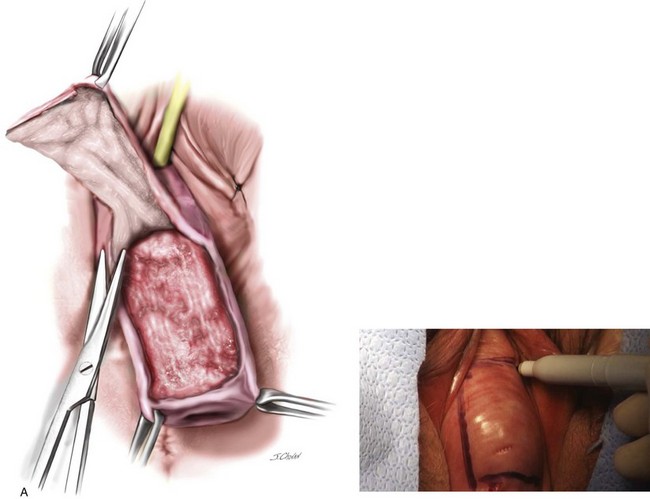
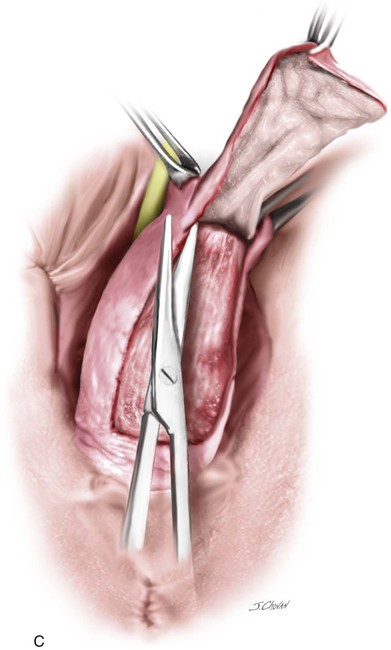
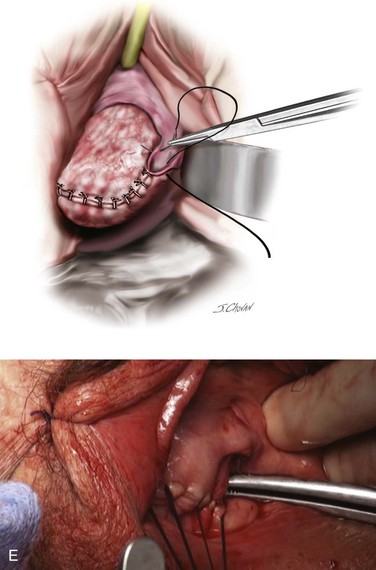
3. The previously outlined areas are removed by sharp dissection (Figure 10-2, A and C). The surgeon should leave the maximum amount of muscularis behind on the bladder and rectum. Hemostasis is an absolute must. While removing the posterior vaginal flap, one should not attempt to enter the peritoneum. If the peritoneum is inadvertently entered, the defect should be closed with an interrupted delayed absorbable suture.
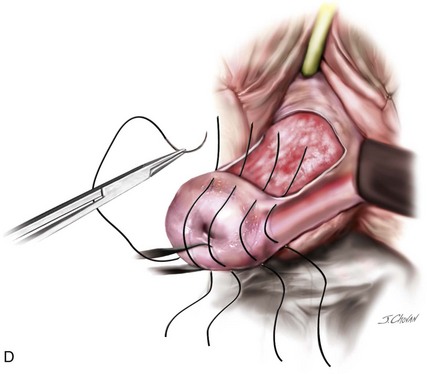
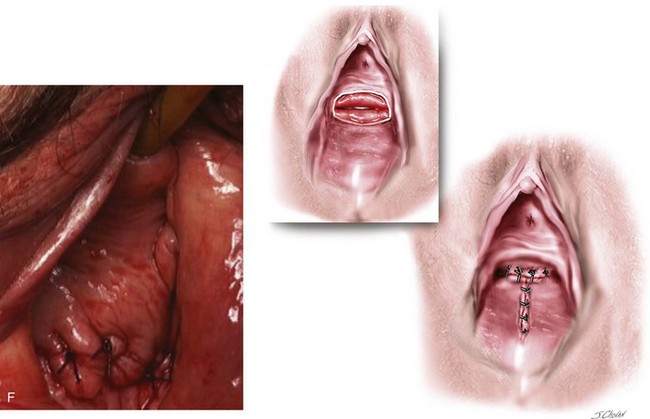
4. The cut edges of the anterior and posterior vaginal walls are sewn together with interrupted delayed absorbable sutures. The knot should be turned into the epithelium-lined tunnels, when possible, which have been created bilaterally (see Figure 10-2, D–E). After the vagina has been inverted, superior and inferior margins of the rectangle can be sutured together (see Figure 10-2, F).
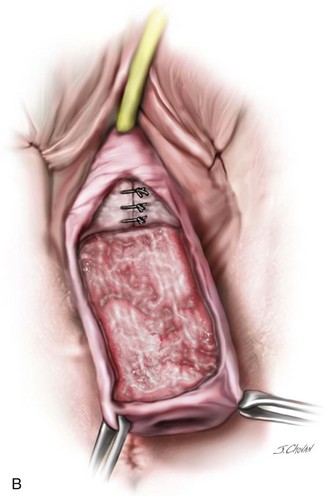
5. In the author’s opinion, a plication of the bladder neck or a synthetic midurethral sling should be routinely performed because of the high incidence of postoperative stress incontinence (see Figure 10-2, B). (Denehy et al, 1995) In addition, an aggressive perineorrhaphy with a distal levator plication should be performed to narrow the introitus, decrease the caliber of the genital hiatus, and build up the perineum. For the technique of levatorplasty, see page 172. (See Video 10-1, “Le Fort Partial Colpocleisis,” for a video demonstration of the procedure. ![]() )
)
Case Discussion
In general, approximately 90% to 95% of patients will have complete relief of symptoms with good anatomic results after undergoing a Le Fort partial colpocleisis. Complete breakdown or partial recurrence can be expected in 2% to 5% of patients, which is mostly because of either poor hemostasis with hematoma formation or an infectious process. Goldman and colleagues (1985) reported results and complications from a modified Le Fort partial colpocleisis in 118 patients; 91% of the patients had good anatomic results, whereas 85% had complete relief of symptoms, 2.5% had recurrence of their prolapse, 10.2% developed incontinence or a worsening of their incontinence, and 1.8% had late vaginal bleeding.
In general, postoperative complications are low in comparison with vaginal hysterectomy and compartmental repairs. De novo stress urinary incontinence is a known risk after obliterative procedures and should be thoroughly evaluated preoperatively with urodynamic testing to ensure that the patient has a normal postvoid residual volume and no evidence of genuine or occult incontinence. (Fitzgerald, 2003) Both the surgeon and the subspecialists should thoroughly assess the postoperative risks of thromboembolic events, cardiovascular issues, and other systemic abnormalities in the patient with multiple co-morbidities to ensure an appropriate surgical and anesthesia plan. (Gerten et al, 2008)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree