Chapter 15 Nuclear medicine techniques in hepatobiliary and pancreatic disease
Positron Emission Tomography
Physics
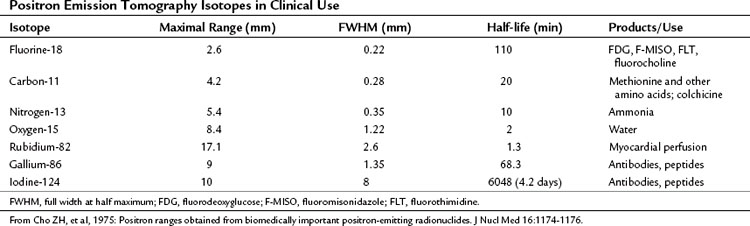
Some elements undergo radioactive decay by ejecting a positron from their nucleus (Table 15.1). A positron is a nuclear particle that has the same mass as an electron, but it has a positive charge. When ejected, the positron moves through surrounding tissues for 1 mm or so, until it eventually combines with a nearby electron, and the mass of both particles is converted to two photons of energy (γ-rays) of 511 keV, which are emitted 180 degrees apart. The PET camera detects these two photons.
Camera Issues
Dedicated Positron Emission Tomography Systems
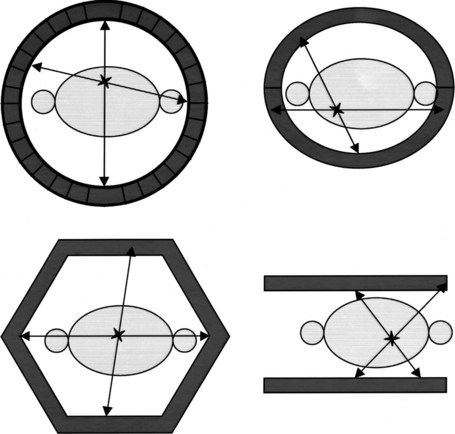
PET machines are constructed using multiple rings of circularly arranged detectors comprising scintillator crystals, such as bismuth germanium oxide crystals, lutetium oxyorthosilicate, or gadolinium orthosilicate, usually without associated collimators. These cameras all work in coincidence, meaning that a true count is generated only when the two 511 keV γ-rays emitted during positron decay simultaneously strike a set of paired detectors (Fig. 15.1). These types of PET imaging devices have high sensitivity. A large amount of usable data is obtained from a given amount of material injected into a patient so that the camera is able to detect small accumulations of injected tracer. The resolution of these machines is defined as the smallest distance between two sources of radiation, whereby the imaging instrument is able to show two sources of radiation rather than one. This distance is currently around 5 mm for most clinical systems; animal imaging devices are now available that have 1-mm resolution (for 18F).
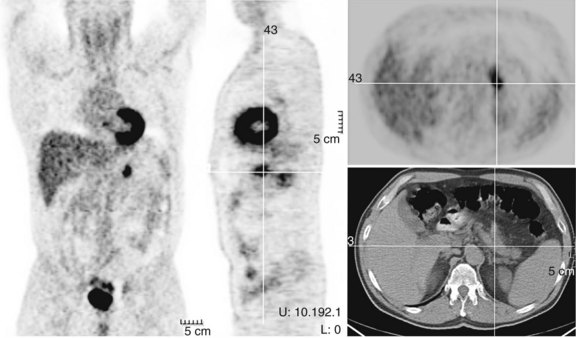
Computed Tomography/Positron Emission Tomography Hybrid Systems
γ-Rays originating in the center of the body have to pass through tissue for a considerable distance to reach the detector, and if one or more of the paired annihilation photons are absorbed, that decay is not recorded as a true count. An anatomically central source would be underrepresented if no attempt were made to correct for differing body tissue density and the depth of the origin of the γ-rays. One of the major advantages of PET imaging is that an accurate correction can be made for this process of attenuation, or loss of counts. Combination machines have been developed (Beyer, 2000) that contain a CT and a PET device in the same imaging gantry. Attenuation correction maps extrapolated from the CT acquisition overcome the attenuation of activity originating in the center of the body. In this way, the PET image becomes quantitative so that the process of computerized data reconstruction ultimately generates a map of the three-dimensional distribution of radioactivity. It is essential that attenuation be performed to obtain quality information from areas such as the porta hepatis, particularly if quantification of radioactivity content in the lesion is to be attempted.
Using PET CT enables coregistration of structural and functional information; this promises near-perfect anatomic localization of areas of functional changes. Some drawbacks with these machines are related to misregistration of the CT data used for attenuation correction in the region of the diaphragm and around the heart, related to cardiorespiratory motion (Beyer et al, 2003). At present there are multiple approaches to this issue but no universally accepted methodology of addressing it.
Biochemistry
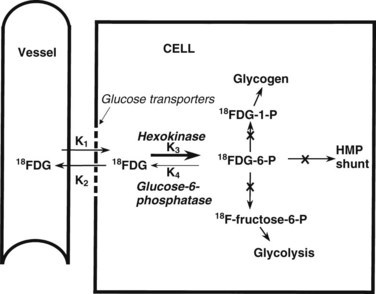
The most common radiopharmaceutical used in PET imaging is FDG, a glucose analogue that crosses cell membranes, sharing the glucose transporter molecules used by glucose. Similar to glucose, it undergoes phosphorylation by the enzyme hexokinase. The resulting molecule, FDG-6-phosphate, is polar; it cannot cross cell membranes and is not a substrate for glucose-6-phosphate isomerase, which converts glucose-6-phosphate to fructose-6-phosphate. FDG-6-phosphate is not a substrate for glucose-6-phosphatase in any tissue except the normal hepatocyte. The net effect is a continuous accumulation and retention of FDG in cells (Fig. 15.2).
Warburg (1930) reported that cancer cells show increased rates of glycolysis compared with normal cells. This discovery has stood the test of time and now underpins the utility of FDG PET imaging in cancer. Glucose metabolism is the most efficient form of energy transfer, and all normal tissues have characteristic glucose metabolic rates. The brain has a high rate of glucose metabolism, and the lung and white fat have low rates. A clump of tumor cells is easier to detect in the lung or in fat than in the brain, because the target-to-background ratio is high in these tissues. The liver has an intermediate glucose metabolic rate. Active inflammatory cells exhibit an increased rate of glycolysis, and sites of active inflammation exhibit increased FDG uptake, although in general the rate of glucose metabolism is lower in inflammatory sites than in most tumors. Sarcoidosis in particular can be quite FDG avid and may have similar patterns and degrees of uptake as some malignancies, such as lymphoma and small cell lung cancer. In such cases, clinical judgment is called into play just as it is in the interpretation of opaque masses in the lung on CT scan.
FDG PET Imaging in Patients with Colorectal Cancer Metastatic to Liver (See Chapter 81A)
Historical Review
The earliest human study of FDG PET in colorectal cancer was performed by Yonekura and colleagues in 1982; this study of large hepatic metastases in three patients with colorectal cancer was successful and showed that these tumors were highly glucose avid. Numerous publications from multiple centers have established that colorectal cancer is readily detected on FDG PET, and colorectal cancer is a common reason for referral of patients for a scan. The value of FDG PET in colorectal cancer patients is based on the consistently accelerated levels of glycolysis seen in colorectal cancer, which results in high FDG uptakes on PET scanning.
Technique
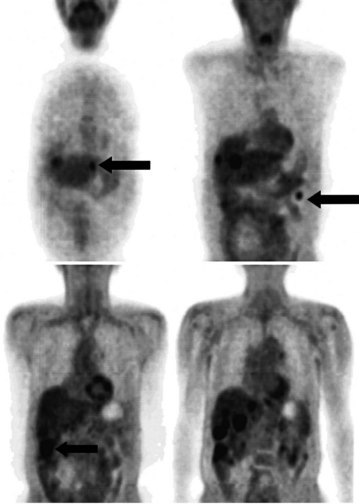
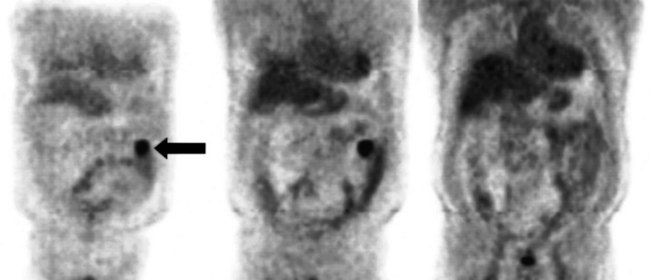
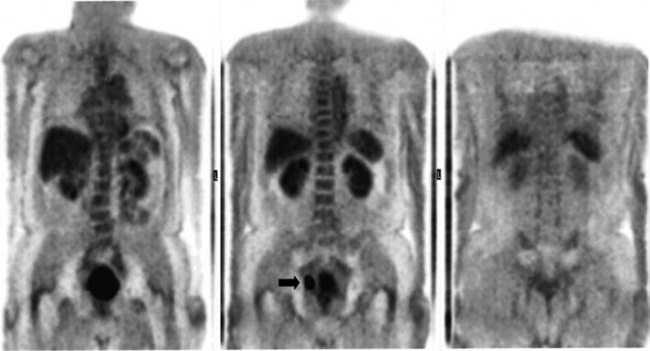
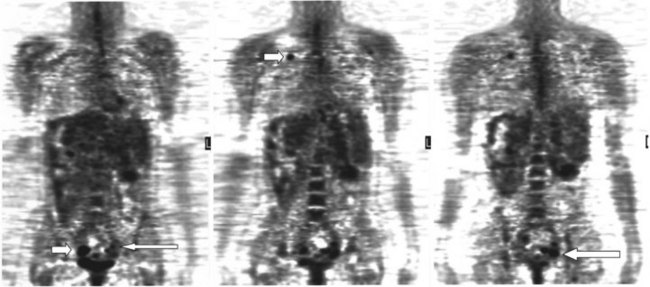
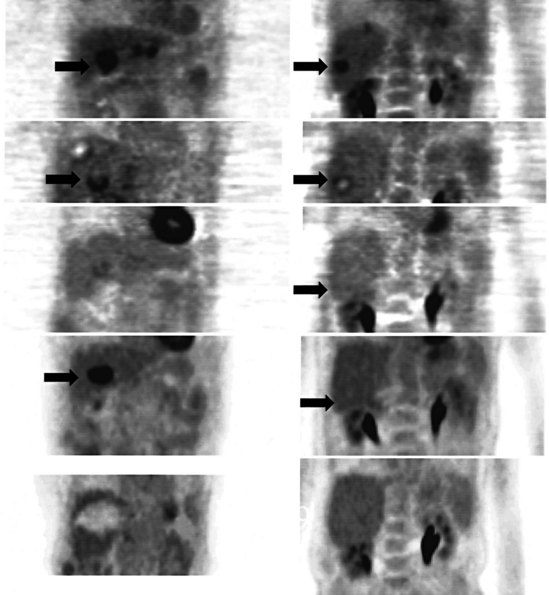
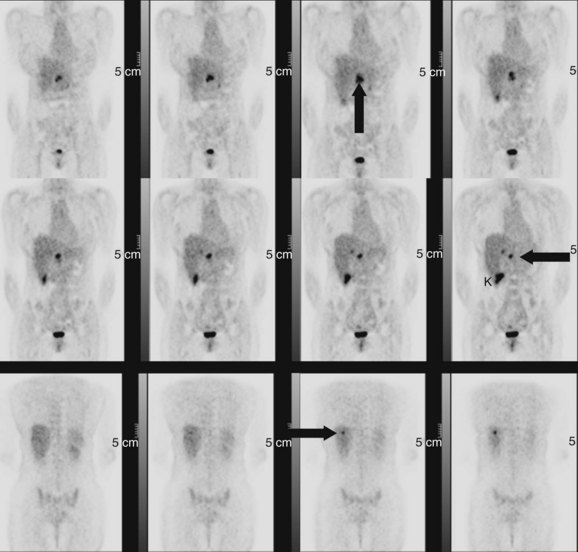
FDG PET studies (Figs. 15.3 to 15.13) are typically performed as a screening procedure that obtains a whole-body image in an attempt to find as many sites of disease as possible. The usual FDG PET CT study of the whole body takes between 7 and 20 minutes, depending on the machine used. The amount of time spent imaging the liver alone is 2 to 4 minutes. If an acquisition of the liver were performed for 1 hour, the accuracy of PET would improve over the values reported in the literature. Nevertheless, FDG PET imaging performs remarkably well with an extraordinary safety profile, with no adverse effects reported in more than 81,000 doses administered over a 4-year period in 22 centers (Silberstein, 1998).
Staging
Preoperative imaging identifies sites of disease in relation to the vascular anatomy of the liver and excludes disease that renders the patient inoperable. Cross-sectional imaging with CT, MRI, and US are the methods of choice to elucidate the vascular anatomy of the liver (see Chapters 13, 16, and 17); nuclear medicine plays no direct role. A secondary role of preoperative imaging is in the demonstration of disease that renders the patient nonresectable. In the best of centers, many patients who are scheduled for hepatic resection are found intraoperatively to have disease that if shown initially would have led to a nonoperative treatment plan (Jarnagin et al, 1999). In a series reported by Scheele and colleagues in 1995, the rates of resection with curative intent steadily increased from 1960 to 1992. Among the many reasons for this increase are improved treatment options and better preoperative imaging that allows more accurate selection of patients with potentially resectable disease. Conventional cross-sectional imaging with helical CT in arterial and portal phases is the standard study for detection of colorectal metastases, and MRI may also be used in conjunction for preoperative evaluation. The previous standard, CT arterial portography, has been supplanted by helical CT, which has equivalent sensitivity for detection of hepatic metastases and results in fewer false positives (Valls et al, 1998).
Fluorodeoxyglucose Positron Emission Tomography for Detection of Hepatic Metastases
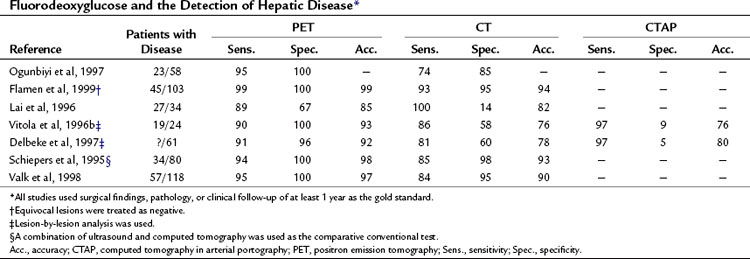
A head-to-head retrospective comparison of CT versus FDG PET clinical readings showed an advantage of FDG PET over CT (Table 15.2). The values reported were 23 with disease (n = 58) and FDG PET sensitivity of 95% and specificity of 100% compared with CT sensitivity of 74% and specificity of 85% (Ogunbiyi et al, 1997). The limitations of this study are its retrospective nature and the lack of information regarding the use of intravenous contrast material; in addition, the FDG PET scans were read with knowledge of the CT, whereas the converse may not have been true.
Another report of 34 patients with colorectal cancer that was potentially resectable, comparing CT with contrast and FDG PET, revealed FDG PET had a sensitivity of 89% and specificity of 67% compared with CT, with a sensitivity of 100% and specificity of 14%, giving an overall accuracy of 85% for FDG PET versus 82% for CT (Lai et al, 1996). A further series of 24 patients, 19 of whom had liver metastases, compared CT, computed tomography in arterial portography (CTAP), and FDG PET on a lesion-by-lesion basis. In terms of accuracy, FDG PET performed better than the radiologic methods: 93% compared with 76% for CT and CTAP. The reason the more sensitive CTAP performed worse than FDG PET is because the specificity of CTAP was only 9%. A separate group reported similar findings; FDG PET accuracy was 92% compared with CT arterial portography (CTAP) and CT accuracy of 80% and 78%, respectively. The low specificity of CTAP (5%) worked to its detriment (Delbeke et al, 1997). Many centers now combine a dedicated CT of the liver as part of the PET CT examination.
Fluorodeoxyglucose Positron Emission Tomography for Detection of Extrahepatic Disease
There has been a remarkable consistency in the rate that FDG PET alters the preoperative stage of a patient after standard-of-care preoperative diagnostic imaging (Table 15.3). In a wide variety of tumors, including colorectal cancers, about 30% of patients conventionally staged have their treatment plans altered as a result of FDG PET. The National Oncology PET Registry (NOPR) study of nearly 23,000 patients revealed a management rate of change of 36% (Hillner et al, 2008). A report of 34 patients with potentially resectable hepatic disease (Lai et al, 1996) found retroperitoneal nodal metastases in six patients, pulmonary metastases in three patients, and locoregional recurrences in two patients. One patient had unexpected disease in two sites, and FDG PET had an influence on clinical management in 10 of 34 patients (29%). The experience at Memorial Sloan-Kettering Cancer Center in the preoperative assessment of patients at high risk of recurrence after hepatic resection of colorectal cancer is similar. We found nine (23%) of 40 patients had their management radically altered owing to FDG PET findings of extensive unresectable disease, with management in another seven patients being influenced by the FDG PET findings confirming isolated, resectable extrahepatic disease, giving a total of 40% of patients in whom management was influenced.
Table 15.3 Influence of FDG PET on Patient Management
| Reference | No. Considered for Surgical Resection | Management Changed as a Result of FDG PET (%) |
|---|---|---|
| Ogunbiyi et al, 1997 | 23 | 43 |
| Flamen et al, 1999 | 37 | 11 |
| Lai et al, 1996 | 34 | 29 |
| Vitola et al, 1996b | 24 | 25 |
| Delbeke et al, 1997* | 61 | 28 |
| Schiepers et al, 1995† | 76 | 26 |
| Valk et al, 1998 | 38 | 32 |
FDG PET; fluorodeoxyglucose positron emission tomography.
* All patients in the study group included as potentially hepatic resection patients were not reported as a separate group.
† 25 unexpected lesions found in 20 patients.
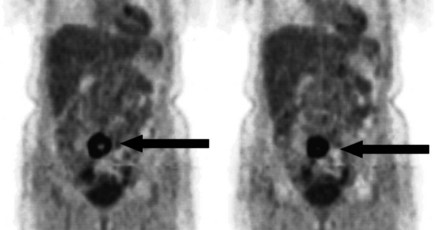
A real strength of FDG PET is its ability to detect extrahepatic disease and alter the surgical plan for the patient. Most if not all lesions detected with FDG PET are within the resolution of conventional imaging modalities and theoretically should be detectable, but lesions either are not recognized as being abnormal (“missed”), or they appear normal. One reason why FDG PET performs so well is that the accelerated glucose metabolism of the tumors makes the tumor stand out against the background of normal tissue, just as the light of a match is easily discerned, even at a distance, on a dark night. The effectiveness of FDG PET is due to its ability to show lesions that mimic a normal structure, particularly intraperitoneal disease (see Figs. 15.4, 15.7, and 15.10), which mimics unopacified loops of bowel and normal-sized lymph nodes replaced by tumor. The influence of a finding of extrahepatic disease depends on the aggressiveness of the approach to disease the treating clinician and the patient wish to undertake. Local pelvic recurrence, if completely resectable, should not prevent a patient from undergoing hepatic resection. FDG PET is not a panacea, however, because an imaging study does not change the biology of a disease, and the fact that disease cannot be detected with FDG PET does not rule out micrometastatic disease. It is important in terms of informed consent that patients appreciate that a workup including FDG PET does not rule out the later appearance of a distant metastasis.
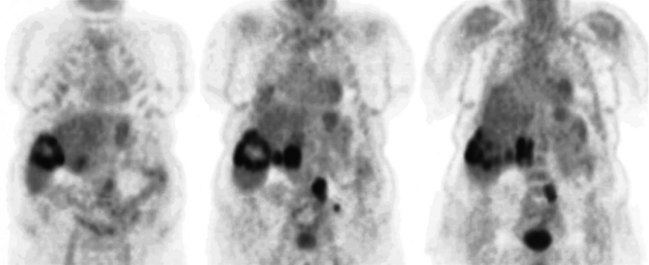
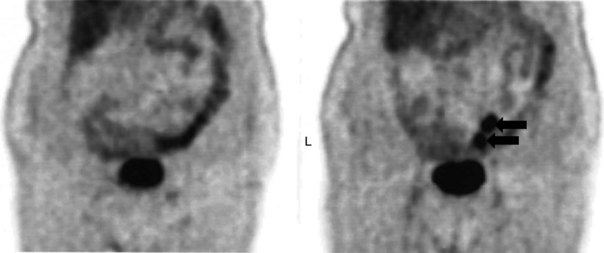
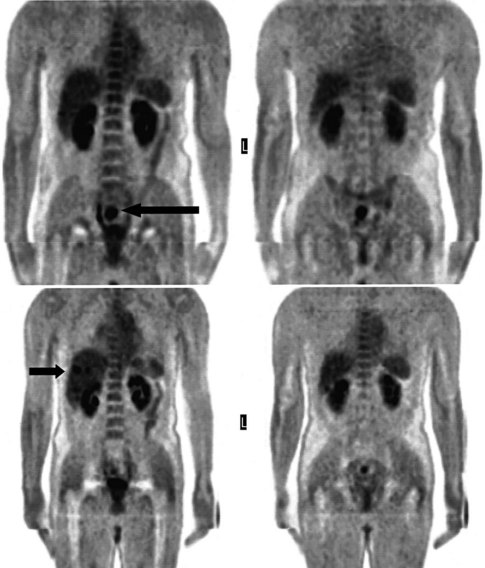
Evaluation of Patients After Treatment
There is a dearth of literature on the relative sensitivities of FDG PET and conventional imaging in the detection of recurrent intrahepatic disease after liver surgery (see Figs. 15.11 to 15.13). Some patients develop subphrenic abscesses after resection, which are difficult to differentiate from recurrent tumor; however, even in this situation, FDG PET seems to perform well. In an initial report of seven patients who had undergone resection previously, PET correctly differentiated recurrent disease from postsurgical change in all; CT misdiagnosed two of six, with one false-positive result and one false-negative result; CTAP misdiagnosed three of five patients, all false-positive results (Vitola et al, 1996b). In the assessment of the effectiveness of chemoembolization (see Chapter 83), FDG PET has been shown to be useful (Vitola et al, 1996a), although an increment over CT and tumor markers has yet to be shown.
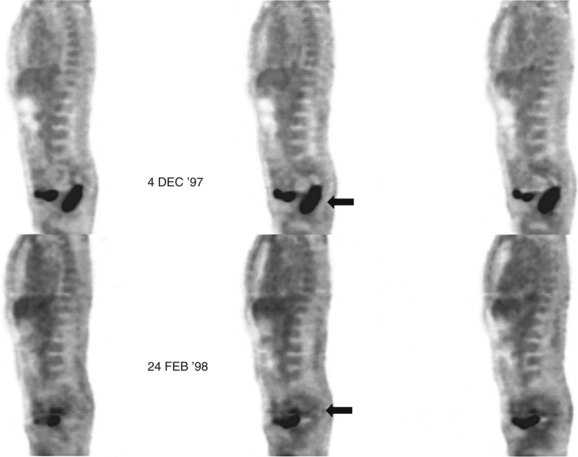
Preliminary investigations suggest FDG PET performed within 24 hours after hepatic cryotherapy (see Chapter 85B) can predict sites of recurrent disease based on the pattern of FDG uptake (Akhurst et al, 1999). This is an exciting development, because it helps clinicians identify patients in whom cryotherapy has been unsuccessful (see Fig. 15.13). The early demonstration of potential treatment failure can assist in further treatment planning. We also have been using FDG PET to follow patients who are being treated with hepatic artery pump therapy (see Chapter 6). In two cases, the information derived from FDG PET would not have been obtainable from conventional imaging, because the effects of cryotherapy persist on CT and US, leading to an inability to differentiate posttreatment change from residual tumor.
Management of Patients with Hepatocellular Carcinoma (See Chapter 80)
Diagnosis
In general, the ease of lesion detection on imaging depends on the target/background ratio. The higher the target-to-background ratio, the easier it is to detect a lesion. A low-grade lesion is likely to have a metabolic profile similar to the surrounding normal tissues. From an imaging standpoint, the liver is a relatively homogeneous solid structure. Because hepatomas are derived from liver tissue, they share many imaging characteristics with a normal liver and are therefore difficult to detect (Schroder et al, 1998). A study aiming to evaluate FDG PET in the diagnosis of liver masses found all primary sarcomas and adenocarcinoma metastases and all cholangiocarcinomas had increased FDG uptake values, but that seven of 23 patients with hepatocellular carcinoma (HCC) had poor FDG uptake (Delbeke et al, 1998). A sound pathophysiologic basis underlies this reduced efficacy, as shown by Torizuka and colleagues (1995) in a study of HCC greater than 3 cm in size. They showed that undifferentiated HCC had a pattern of continual FDG uptake shared by most solid tumors, whereas a moderately differentiated HCC showed a pattern of uptake similar to the normal liver, with an initial rise and then a slow fall. The difference in pattern was due to marked differences in the activity of transporters carrying glucose into the cell and in hexokinase activity, but it may also be due to a similarity between normal liver and HCC in terms of the rate of dephosphorylation of FDG-6-phosphate.
Treatment Planning and Assessment of Prognosis
The survival rate of HCC patients seems to correlate with the degree of FDG uptake into the tumor, with patients with low FDG uptake showing a longer survival than patients with high FDG uptake (Enomoto et al, 1991). FDG uptake may correlate with the degree of expression of p53 (Schroder et al, 1998; Yoon et al, 1998), a known factor in hepatocellular carcinogenesis (Hui et al, 1998). In a similar fashion to other tumors, FDG PET has been shown to be effective in monitoring lipiodol chemoembolization in HCC (Torizuka et al, 1994).
Cholangiocarcinoma (See Chapter 50A, Chapter 50B, Chapter 50C, Chapter 50D )
The detection of cholangiocarcinoma in patients with primary sclerosing cholangitis can be difficult, because imaging findings of the underlying disease may mimic those of tumor. Preliminary reports indicate a potential role of FDG PET, because cholangiocarcinoma seems to be FDG avid (Delbeke et al, 1998; Keiding et al, 1998), although this may be limited to follow-up assessment (Berr et al, 1999). If active cholangitis is present, the mucosal inflammation may obscure small sites of carcinoma in situ. If strictures are stented, the resultant mucosal irritation also may make the diagnosis of malignancy more difficult. Screening for cholangiocarcinoma may require interrogation of a different metabolic pathway, such as that of protein synthesis or proliferation.
In an analysis of data at Memorial Sloan-Kettering Cancer Center, 82 patients with cholangiocarcinoma were studied; 24% of the 62 newly diagnosed patients had their management changed as a result of the detection of occult metastases. FDG PET detected 95% of the intrahepatic tumors and 69% of the extrahepatic tumors; this is not surprising, because central cholangiocarcinomas are more often clinically silent and present later in terms of size than extrahepatic tumors. In terms of the detection of metastases, 100% of metastases from intrahepatic tumors and 93% from the extrahepatic group were detected (Corvera et al, 2004). An example of a cholangiocarcinoma detected with FDG PET is shown in Figure 15.14.
Focal Liver Lesions
A focal liver lesion in a patient with a recent history of colorectal cancer and increasing carcinoembryonic antigen (CEA) is likely due to a metastasis; this partly explains the high success rates in detecting malignant disease reported by some groups (Delbeke et al, 1998). In a separate group, FDG PET was not found to be useful in the characterization of liver masses in patients with chronic hepatitis C infection (Schroder et al, 1998).
Diagnosis and Follow-up of Pancreatic Diseases
Pancreatic Cancer (See Chapter 58A, Chapter 58B )
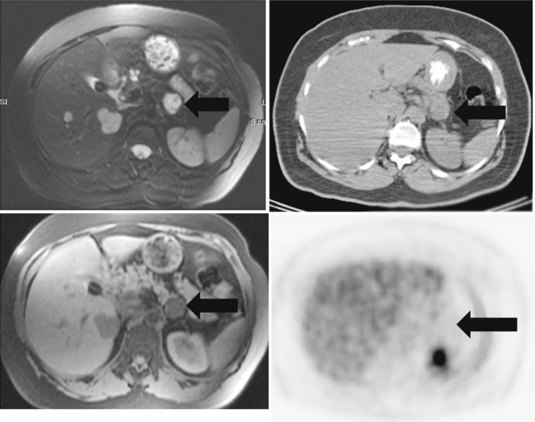
The clinical presentation of painless jaundice in a middle-aged individual should immediately raise the clinical suspicion of the presence of a cancer obstructing the common bile duct; this is most commonly due to a cancer of the head of the pancreas. Classic approaches to imaging of masses of the head of the pancreas still have validity, with US being the least invasive test available. If surgical resection is to be considered, MRI is likely to give the best possible local soft-tissue discrimination, allowing for planning of a surgical approach and the best assessment of the pancreatic and biliary ducts. Most solid pancreatic adenocarcinomas are FDG avid (Fig. 15.15), allowing for the screening of patients for unexpected distant disease and for the possibility of assessment of the response of the pancreatic mass to induction therapy, if that is considered appropriate. The implementation of PET CT allows much greater confidence in the localization of focal epigastric FDG uptake to a particular anatomic structure; previously epigastric FDG uptake was described as a regional, rather than an organ-specific, phenomenon.
The mechanism of FDG uptake into cells is exactly the same as for unlabeled glucose, so according to the laws of mass action, a high serum concentration of unlabeled glucose (as seen in diabetics with insulin resistance) reduces the amount of FDG uptake into cancer cells, leading to a reduction in sensitivity. In a study of 106 patients with pancreatic masses, of which 32 were benign, PET showed an overall sensitivity of 85%, a specificity of 84%, a negative predictive value of 71%, and a positive predictive value of 93%. In a subgroup of patients with normal serum glucose levels (n = 72), the results were 98%, 84%, 96%, and 93%, respectively (Zimny et al, 1997). Insulin-sensitive patients also present an interesting problem because incorrect timing of the FDG injection in relation to the insulin injection may lead to much of the injected FDG being driven into muscle, reducing tumor sensitivity.
Cystic pancreatic masses (see Chapter 57) present a difficult imaging problem, because they consist of a thin layer of cells surrounding a large void (Fig. 15.16). A large report of 599 patients with cystic masses of the pancreas found 280 (46.8%) were pseudocysts, 102 (17%) were intraductal papillary mucinous tumors, 100 (16.7%) were serous tumors, 62 (10.4%) were mucinous tumors, 39 (6.5%) were mucinous cystadenocarcinoma, and 16 (2.7%) were solid papillary cystic tumors (Bassi et al, 2003). Clues that a cystic mass of the pancreas may be neoplastic, rather than due to a pseudocyst, include the absence of symptoms (Fernandez-del Castillo et al, 2003) and the presence of calcification in the wall of the cyst, rather than the entire pancreas, as is seen in chronic pancreatitis. Multiloculated cystic lesions favor a neoplastic origin, rather than the single cyst seen in a pseudocyst.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree