Chapter 29 Bile duct exploration and biliary-enteric anastomosis
Anatomy
Safe operative planning and technique demand a comprehensive understanding of the extrahepatic biliary anatomy and a thorough appreciation for the common anatomic variants that may be encountered. Hepatobiliary anatomy is discussed at length in Chapter 1B; in this section, we will highlight specific aspects deserving of additional emphasis.
The typically short extrahepatic course of the right hepatic duct makes operative access to the segmental or sectional drainage of the right hemiliver rather difficult. However, the biliary anatomy of the right hemiliver is rather prone to variation, and aberrant drainage from the right anterior or posterior section may assume a long extrahepatic course before joining with the left hepatic ductal system. In comparison, the left biliary system is relatively consistent. Also in contrast to the right, the left hepatic duct invariably has a longer extrahepatic course as it runs along the undersurface of segment IVb (Fig. 29.1). In cases where the base of segment IVb is broad, the left hepatic duct assumes a longer and more transverse course; in cases where the base of segment IVb has a narrower and pyramidal configuration, the course of the left hepatic duct is shorter and more oblique. Drainage from most of segment I enters into the left hepatic duct just before its convergence with the right hepatic duct; drainage from the right portion of segment I typically enters into the right posterior sectoral duct. The left hepatic duct runs along the left portal vein within a peritoneal reflection of the gastrohepatic ligament, and it is best exposed by lowering the hilar plate along the base of segment IVb (Fig. 29.2). These structures are joined by the left hepatic artery as they enter the umbilical fissure, where arterial and venous branches to and biliary ducts from segments II, III, and IV are found. The ligamentum teres along the lower edge of the falciform ligament runs across the umbilical fissure, which is often covered by a bridge of hepatic tissue that crosses from the left lateral section to the base of segment IV. This bridge of tissue must often be divided to permit full exposure of and access to the biliary and vascular structures to and from segments II, III, and IV (Fig. 29.3).
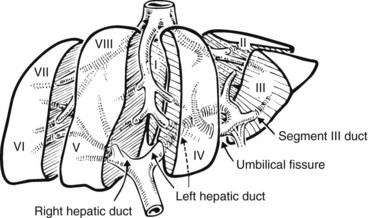
FIGURE 29.1 Diagrammatic expanded view of the liver showing its segmental structure. Elements of the portal triad are distributed to the right and left liver on a segmental basis. The left hepatic duct always pursues an extrahepatic course beneath the base of the quadrate lobe (segment IV) in the groove separating the quadrate from the caudate lobe (segment I; see Fig. 29.2). The ligamentum teres marks the umbilical fissure and runs to join the umbilical portion of the left branch of the portal vein. Each portal triad is composed of hepatic artery, portal vein, and biliary duct. Note the distribution of the left portal triad in the umbilical fissure; major branches recurve to the quadrate lobe medially, and two major branches pursue a lateral course to segments II and III of the left lobe.
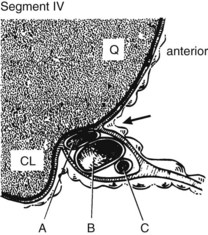
FIGURE 29.2 Sagittal section showing the relationship of the quadrate (Q) and caudate lobe (CL) to the left portal triad, which is encased within a reflection of the lesser omentum that fuses with the Glisson capsule at the base of the quadrate lobe. The arrow indicates the point of incision for the dissection to lower the hilar plate (see also Fig. 29.5). A, Left hepatic duct. B, Left branch, portal vein. Note the left hepatic artery (C) joins the left duct and left branch of the portal vein at the umbilical fissure.
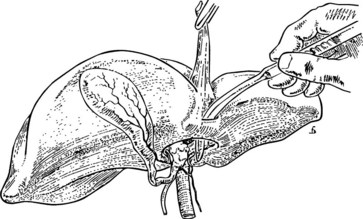
FIGURE 29.3 The bridge of liver tissue frequently present between the base of the quadrate lobe (segment IV) and the left lobe of the liver can be divided. This is conveniently done by passing a curved director beneath it and cutting it with diathermy. Such division can be useful in aiding an approach to the left hepatic duct, particularly if the course of the duct is vertical and the base of the quadrate lobe is short. If the bridge of tissue is present, the maneuver is always necessary to allow dissection of the segment III duct (see Fig. 29.8).
Bile Duct Exploration
Overview
The most common indication for exploration of the biliary system is the presence of common bile duct stones. Contemporary percutaneous and endoscopic techniques have largely replaced operative interventions for this indication, and nonoperative, laparoscopic, and open operative strategies are addressed in greater detail in Chapters 34, 35, and 36, respectively. In this chapter, we highlight the various operative approaches for open exploration of the bile ducts.
Incision and Exposure
A right subcostal incision generally affords satisfactory exposure of the extrahepatic biliary system. The hepatic flexure of the right hemicolon is mobilized, and the proximal transverse colon is mobilized off the duodenum. Downward retraction of the proximal transverse colon facilitates exposure of the duodenum, whose retroperitoneal attachments are freed with a generous Kocher maneuver. A cholecystectomy is often performed in conjunction with bile duct exploration for patients with calculous disease, and removal of the gallbladder greatly enhances exposure of and access to the porta hepatis. Alternatively, retraction of the mobilized gallbladder can be useful for exposing the junction of the cystic duct and common bile duct. Cephalad retraction of the undersurface of the liver along the base of segment IVb also enhances optimal visualization of the extrahepatic biliary system (Fig. 29.4).
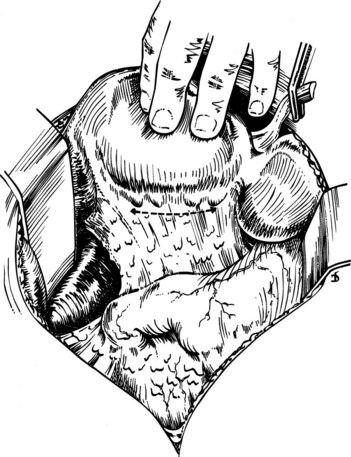
FIGURE 29.4 The initial line of incision for an approach to the left hepatic duct by lowering of the hilar plate. The liver is elevated, and the quadrate lobe is retracted upward. The incision is made at precisely the point at which the Glisson capsule reflects to the lesser omentum (see Fig. 29.2).
Supraduodenal Exploration (See Chapter 35)
Choledochotomy
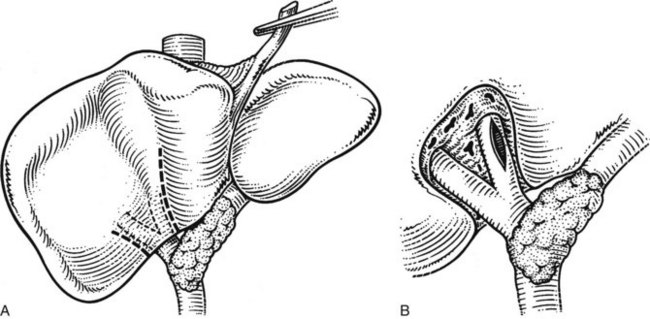
Open exploration of the extrahepatic biliary system is best undertaken through a longitudinal distal choledochotomy. Opening the common bile duct distally toward the duodenum facilitates exploration of the distal biliary system and permits easy construction of a choleodochoduodenostomy, if necessary. Care must be taken to verify the anatomic relationship between the cystic duct and common bile duct, as low or anterior insertion of the cystic duct can result in unintended injury to this structure (Fig. 29.5). Placement of the incision in an anterior location minimizes the risk of injury to the periductal vasculature, which typically runs along the medial and lateral aspects of the common hepatic and common bile ducts. The length of the choledochotomy is dictated by the diameter of the duct and the size of the stones present within its lumen, but length typically ranges between 1 to 2 cm.
A number of options exist for bile duct exploration, and these are discussed in further detail in Chapters 34 and 35; regardless of the method used, care must be taken to be as atraumatic as possible (Orloff, 1978). Iatrogenic injury to the duct mucosa can result in delayed stricture formation, and inaccurate delivery of rigid instrumentation can create false passages into the duodenum or pancreas. Fiberoptic choledochoscopy permits excellent visualization when saline is infused at a low rate through the endoscope. This is particularly effective for exploring the smaller intrahepatic radicles of the proximal biliary system.
Transduodenal Exploration
In unusual cases in which gallstones are impacted at or near the ampulla of Vater, or in patients whose surgically altered anatomy makes endoscopic techniques difficult (e.g., after Roux-en-Y gastrojejunostomy), transduodenal exploration may be warranted. Transduodenal access to the distal biliary system requires operative sphincterotomy, which in turn requires operative sphincteroplasty to avoid postoperative papillary stenosis. Chapter 62C discusses transduodenal resections for neoplastic disease, the details of which are not dissimilar to the approach used for calculous disease (see Chapter 35).
Outcomes After Bile Duct Exploration
Advances in endoscopic and percutaneous approaches have vastly limited the indications for operative bile duct exploration. Nevertheless, it is important to recognize that historical analyses have largely substantiated the safety and efficacy of operative bile duct exploration. In a representative single-center North American series of 100 consecutive, open, supraduodenal common bile duct explorations, no operative mortalities were encountered, and the overall morbidity rate was 15.7%, including a 5.3% rate of retained common duct stones (Pappas et al, 1990). Similar observations have been reported in retrospective analyses of transduodenal sphincteroplasties and common bile duct explorations (Kibria & Hall, 2002; Morgan et al, 2008; Sellner et al, 1988), highlighting low rates of morbidity and recurrent choledocholithiasis.