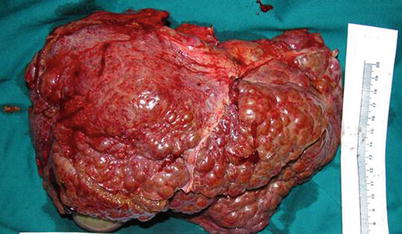
Fig. 33.1
The great saphenous vein of the recipient
Figs. 33.2 and 33.3
Incision of receptor
33.1.3 Exposure
A retractor is used to expose the operating field, especially secondary porta of liver and the right liver, for ease of reconstruction and improved surgical access to the suprahepatic vena cava.
33.1.3.1 Abdominal Exploration
In recipients with liver cancer, the presence of extrahepatic metastases and portal vein tumor thrombus should be carefully evaluated. Splenectomy is preferred in patients with splenomegaly and hypersplenism in order to improve blood clotting function.
33.1.3.2 Dissection of the First Porta Hepatis
Expose the junction of the cystic duct and the common bile duct, and then cut the peritoneum on the surface of the hepatoduodenal ligament. After that, separate the cystic duct from the cystic artery and cut cystic duct and cystic artery off.
Dissect the hepatic artery to the left of the hepatoduodenal ligament and dissect the right and left hepatic arteries from the bottom of the proper hepatic artery. Do not pull on the hepatic artery in order to avoid endothelial disruption.
Dissect the common bile duct up to the junction of the left and right hepatic ducts. Preserve a sufficient length of the bile duct, and then cut the common bile duct, protecting the surrounding tissue and the blood supply.
Dissect the portal vein up to the right and left portal veins and down to the head of the pancreas in order to prepare the abscission (Fig. 33.4).
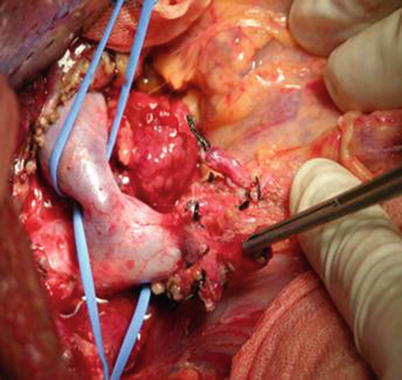
Fig. 33.4
Dissection of the first porta hepatis
In patients with HCC, lymph nodes must be removed.
33.1.3.3 Dissection of the Ligaments around the Liver
Extensive tissue adhesions and abundant collateral circulation are generally found in patients with portal hypertension. To prevent bleeding, the ligaments around the liver should be dissected after dissecting the first porta hepatis. The procedure is performed as follows. An electrotome is used to remove the falciform ligament of the liver, and then the left triangular ligament must be ligated or transfixed because of collateral circulation. The left coronary ligaments are removed, the left lobe is turned outward, and the hepatogastric ligament is ligated and removed in order to reveal whether an aberrant left hepatic artery originates from the left gastric artery. Then the right triangular ligament and the coronary ligament are exposed and removed. The right lobe is pushed to the left, and the hepatocolic ligament is removed. The liver is turned to the left, the peritoneum posterior to the right lobe is opened, and the suprahepatic vena cava is dissected. The left and caudate lobes are turned to the right, and the peritoneum is cut lengthwise along the retrohepatic inferior vena cava to expose the left branch of the posterior cava; the retrohepatic inferior vena cava is then dissected. The posterior peritoneum is cut at the level of the renal veins, and the infrahepatic vena cava is dissected.
It is important to note that the dissection of the ligaments around the liver should follow the liver closely. There is no need to dissect the retrohepatic inferior vena cava completely in patients with severe portal hypertension, except in cases of retroperitoneal hemorrhage. The liver should be manipulated less extensively in recipients with cancer especially when the tumor is next to the secondary porta of liver. In such situations, the dissection of the retrohepatic inferior vena cava should be done in preparation for clipping, instead of dissecting the ligaments around the liver, which can be handled when the hepatectomy begins.
33.1.4 Hepatectomy
The bile duct, hepatic artery, and portal vein are transected; then the suprahepatic vena cava is clipped with vessel forceps. The anatomical position of liver should be noted, and the vessel forceps should be kept in a horizontal position. To prevent slippage, the forceps can clamp the diaphragm and be fastened by ligation. The suprahepatic and infrahepatic vena cava is transected close to the surface of the liver. Cutting the liver near the back of the suprahepatic vena cava can reduce the surface area of the wound and decrease bleeding (Fig. 33.5).