This review covers minimally invasive treatments for ureteropelvic junction obstruction in the adult, including endopyelotomy (antegrade and retrograde), endopyeloplasty, laparoscopic pyeloplasty, and robotic pyeloplasty. The relevant literature is summarized, and a rational algorithm for management is proposed.
Ureteropelvic junction obstruction (UPJO) is the most common congenital abnormality of the ureter, with an annual incidence of 5 per 100,000 population. For many years, open pyeloplasty remained the ‘gold-standard’ treatment, with success rates greater than 90%. During the last 2 decades, multiple minimally invasive methods have been used for the surgical management of UPJO, including endopyelotomy, endopyeloplasty, and laparoscopic and robotic pyeloplasty. The choice of initial surgical intervention is important because it is likely to influence the final outcome.
This review covers minimally invasive treatments for UPJO in the adult, including endopyelotomy (antegrade and retrograde), endopyeloplasty, laparoscopic pyeloplasty (LP), and robotic pyeloplasty. The relevant literature is summarized, and a rational algorithm for management is proposed.
Diagnostic workup
The goals of diagnostic evaluation in a patient suspected of having a UPJO are to confirm functional obstruction, determine differential renal function, and assess the anatomy at the uteropelvic junction (UPJ). Mercaptoacetyl-Tri-Glycine (MAG3) diuretic renal scan typically achieves the first two goals. A retrograde pyelogram (usually at the time of surgical procedure) confirms the length of stricture and degree of hydronephrosis. A spiral CT angiogram may be useful in preoperative detection of a crossing vessel in a patient in whom endopyelotomy is being considered as a treatment option.
Endopyelotomy
In 1903, Albarran first described full-thickness incision of a narrow ureteral segment followed by prolonged stenting. Endoscopic pyelolysis was first described by Wickham and Kellett and popularized by Badlani and colleagues as endopyelotomy. The key concept of endopyelotomy is based on the principle of intubated ureterostomy developed by Davis : regeneration of the ureter over a stent for 6 weeks after a full-thickness incision, causing a durable increase in the caliber of the strictured segment. The exact mechanism of ureteral healing, however, remains unclear. A combination of wound contracture and smooth muscle regeneration likely contributes to healing of the endopyelotomy defect.
Many variables have been suggested as predictors of poor prognosis after endopyelotomy, including the presence of crossing vessels, severe hydronephrosis, long (>1.5 cm) stricture length, poor ipsilateral renal function, and previous failed endopyelotomy. The discussion of the impact of crossing vessels on the outcome after endopyelotomy continues to be debated. Van Cangh and colleagues reported 46% success in patients with crossing vessels and 86% without. Evaluating the Acucise technique, Nakada and colleagues reported lower success in patients with crossing vessels (96% versus 64%). One would expect a higher incidence of crossing vessels found at secondary pyeloplasty after failed endopyelotomy, but results are inconsistent. Knudsen and colleagues and Van Cangh and colleagues found crossing vessels in 83% and 87% of their cases, respectively. In contrast, Gupta and colleagues attributed only 4% cases of endopyelotomy failure to crossing vessels.
Poor renal function and significant hydronephrosis seem to predict a higher failure rate after endopyelotomy. In patients with poor renal function, the success rate was 54% compared with 94% in patients with normal renal function . Danuser and colleagues described a success rate of 87% in patients with a pyelocalyceal volume less than 50 cm 3 , 81% with a volume from 50 to 100 cm 3 , and 69% with a volume greater than 100 cm 3 .
Antegrade (percutaneous) endopyelotomy
Initially reported by Ramsay and colleagues in 1984, the technique has several variations: cutting between two wires, cutting over a stent , invagination of the UPJ , and external incision of the UPJ through a transpelvic route . Cold knife, electrocautery, and laser have each been reported, with none conclusively demonstrated to be superior over the others. Antegrade endopyelotomy is particularly suitable in patients who have concomitant large-volume stone disease. Success rates with antegrade endopyelotomy range between 67% and 88% ( Table 1 ).
| First author | Senior author | Year | Cases | Technique | Primary UPJO (n) | Crossing vessels (%) | Open conversion (%) | OR time (minutes) | Hospital stay (days) | Follow-up (months) | Symptomatic success (%) | Radiographic success (%) | Complications (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Motola | Smith | 1993 | 212 | Cold knife | 110 | 79 | 1.5 | 119 | 4.1 | 25 | 85 | 86 | 16% |
| Van Cangh | Lorge | 1994 | 102 | Cold knife | 81 | 57 | 0 | 252 | 3.3 | 26 | Not stated | 73 | Not stated |
| Kletscher | Patterson | 1995 | 50 | Cold knife | 49 | 42 | 5.4 | 185 | 4.5 | 14 | 92 | 88 | Not stated |
| Gupta | Smith | 1997 | 401 | Cold knife | 235 | 42 | 5.5 | 164 | 2.6 | 19 | Not stated | 85 | Not stated |
| Danuser | Studer | 1998 | 80 | Cold knife | 80 | 57 | 0 | 165 | 3.7 | 23 | Not stated | 81 | 13 |
| Shalhav | Clayman | 1998 | 63 | Electrocautery | 40 | 16 | 6.4 | 179 | 4 | 12 | 89 | 85 | 27 |
| Knudsen | Denstedt | 2004 | 80 | Electrocautery (77), laser (3) | 61 | 54 | Not reported | 246 | 3.1 | 24 | Not stated | 67 | Not stated |
Endopyelotomy
In 1903, Albarran first described full-thickness incision of a narrow ureteral segment followed by prolonged stenting. Endoscopic pyelolysis was first described by Wickham and Kellett and popularized by Badlani and colleagues as endopyelotomy. The key concept of endopyelotomy is based on the principle of intubated ureterostomy developed by Davis : regeneration of the ureter over a stent for 6 weeks after a full-thickness incision, causing a durable increase in the caliber of the strictured segment. The exact mechanism of ureteral healing, however, remains unclear. A combination of wound contracture and smooth muscle regeneration likely contributes to healing of the endopyelotomy defect.
Many variables have been suggested as predictors of poor prognosis after endopyelotomy, including the presence of crossing vessels, severe hydronephrosis, long (>1.5 cm) stricture length, poor ipsilateral renal function, and previous failed endopyelotomy. The discussion of the impact of crossing vessels on the outcome after endopyelotomy continues to be debated. Van Cangh and colleagues reported 46% success in patients with crossing vessels and 86% without. Evaluating the Acucise technique, Nakada and colleagues reported lower success in patients with crossing vessels (96% versus 64%). One would expect a higher incidence of crossing vessels found at secondary pyeloplasty after failed endopyelotomy, but results are inconsistent. Knudsen and colleagues and Van Cangh and colleagues found crossing vessels in 83% and 87% of their cases, respectively. In contrast, Gupta and colleagues attributed only 4% cases of endopyelotomy failure to crossing vessels.
Poor renal function and significant hydronephrosis seem to predict a higher failure rate after endopyelotomy. In patients with poor renal function, the success rate was 54% compared with 94% in patients with normal renal function . Danuser and colleagues described a success rate of 87% in patients with a pyelocalyceal volume less than 50 cm 3 , 81% with a volume from 50 to 100 cm 3 , and 69% with a volume greater than 100 cm 3 .
Antegrade (percutaneous) endopyelotomy
Initially reported by Ramsay and colleagues in 1984, the technique has several variations: cutting between two wires, cutting over a stent , invagination of the UPJ , and external incision of the UPJ through a transpelvic route . Cold knife, electrocautery, and laser have each been reported, with none conclusively demonstrated to be superior over the others. Antegrade endopyelotomy is particularly suitable in patients who have concomitant large-volume stone disease. Success rates with antegrade endopyelotomy range between 67% and 88% ( Table 1 ).
| First author | Senior author | Year | Cases | Technique | Primary UPJO (n) | Crossing vessels (%) | Open conversion (%) | OR time (minutes) | Hospital stay (days) | Follow-up (months) | Symptomatic success (%) | Radiographic success (%) | Complications (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Motola | Smith | 1993 | 212 | Cold knife | 110 | 79 | 1.5 | 119 | 4.1 | 25 | 85 | 86 | 16% |
| Van Cangh | Lorge | 1994 | 102 | Cold knife | 81 | 57 | 0 | 252 | 3.3 | 26 | Not stated | 73 | Not stated |
| Kletscher | Patterson | 1995 | 50 | Cold knife | 49 | 42 | 5.4 | 185 | 4.5 | 14 | 92 | 88 | Not stated |
| Gupta | Smith | 1997 | 401 | Cold knife | 235 | 42 | 5.5 | 164 | 2.6 | 19 | Not stated | 85 | Not stated |
| Danuser | Studer | 1998 | 80 | Cold knife | 80 | 57 | 0 | 165 | 3.7 | 23 | Not stated | 81 | 13 |
| Shalhav | Clayman | 1998 | 63 | Electrocautery | 40 | 16 | 6.4 | 179 | 4 | 12 | 89 | 85 | 27 |
| Knudsen | Denstedt | 2004 | 80 | Electrocautery (77), laser (3) | 61 | 54 | Not reported | 246 | 3.1 | 24 | Not stated | 67 | Not stated |
Retrograde endopyelotomy
Ureteroscopic approach
Ureteroscopic retrograde endopyelotomy was initially reported by Inglis and Tolley in 1986. The most attractive feature of the ureteroscopic approach is the potentially reduced morbidity when compared with the percutaneous approach. The risk for subsequent ureteral stricture was historically higher with the use of large-diameter ureteroscopes and electrocautery . Whereas preemptive stenting was previously necessary to achieve passive ureteral dilatation, current small profile semirigid ureteroscopes and flexible ureteroscopes have practically abolished this need and significantly reduced ureteral complications with this procedure. The incision is performed using the holmium:yttrium-aluminum-garnet (YAG) laser at 10 W through a 200- to 365-μ laser fiber. Symptomatic and radiographic success range from 65% to 91% and from 73% to 85%, respectively . Geavlete and colleagues reported a success rate of 83.3% (18 months of follow-up) in 30 patients who had secondary UPJO (failed pyeloplasty [17 cases], failed endopyelotomy [13 cases]) ( Table 2 ).
| First author | Senior author | Cases | Technique (n) | Primary UPJ (n) | Crossing vessels (%) | Follow-up (months) | Symptomatic success (%) | Radiographic success (%) |
|---|---|---|---|---|---|---|---|---|
| Conlin | Bagley | 21 | Electrocautery (14), laser (6), cold knife (1) | 15 | 57% | 23 | Not stated | 81 |
| Renner | Rassweiler | 34 | Laser | 27 | Not stated | 18 | 92 | 85 |
| Giddens | Grasso | 23 | Laser | 18 | 17 | 10 | Not stated | 83 |
| Gerber | Kim | 22 | Electrocautery (16), laser (6) | 18 | Not stated | 20.5 | 91 | 82 |
| Matin | Streem | 45 | Laser | 40 | Not stated | 23.2 | 65 | 73 |
Acucise endopyelotomy
Acucise endopyelotomy consists of a balloon electrocautery incision performed under fluoroscopic control and was first proposed by Chandhoke and colleagues in 1993. Drawbacks of cutting-wire endopyelotomy include difficulty in controlling the rate and depth of the incision and the risk for hemorrhage because of the lack of direct visual control. Bleeding complications have been reported in 3% to 10% of cases . Results from select series of cutting-wire balloon endopyelotomy are summarized in Table 3 .
| First author | Senior author | Year | Cases (n) | Primary UPJO (n) | Follow-up (months) | Symptomatic success (%) | Radiographic success (%) | Complications |
|---|---|---|---|---|---|---|---|---|
| Nadler | Clayman | 1996 | 26 | 17 | 33 | 89 | 81 | 0 |
| Preminger | Smith | 1997 | 66 | 52 | 8 | Not stated | 77 | 4.5 |
| Faerber | Ohl | 1997 | 32 | 27 | 14 | Not stated | 81 | 15.6 |
| Gelet | Dubernard | 1997 | 44 | 21 | 12 | Not stated | 78 | 4.6 |
| Kim | Albala | 1998 | 77 | 61 | 12 | Not stated | 78 | 4 |
| Lechevalier | Coulange | 1999 | 36 | 23 | 24 | Not stated | 75 | Not stated |
| Biyani | Hetherington | 2002 | 42 | 34 | 27 | 64 | 52 | 10 |
| Weikert | Schrader | 2005 | 24 | 24 | 32 | 58 (overall) | 58 (overall) | 12.5 |
El-Nahas and colleagues compared Acucise with ureteroscopic endopyelotomy in 40 patients who had UPJO in a prospective randomized trial (follow-up of 30 months). Exclusion criteria included the presence of crossing vessels, renal function less than 20%, or hydronephrosis of grade 3 or greater. Success rates were 85% for the ureteroscopic group and 65% for the Acucise group. There was no difference in the complication rate.
Preference of the surgeon, anatomic factors, and concomitant calculi are the main factors considered in the choice between the percutaneous and ureteroscopic approaches for endopyelotomy. The main advantage of percutaneous approaches is the ability to treat concomitant calculi. Body habitus or anatomic issues that may have previously limited retrograde access have decreased with modern ureteroscope technology, and decreased morbidity makes retrograde endopyelotomy an attractive option for the appropriate short-segment stricture.
Stenting after endopyelotomy
Stenting after endopyelotomy is still debated. No consensus exists regarding optimal stent size or duration of stenting. The assumption that a larger stent would result in a larger final caliber if healing occurs around the stent has been analyzed. Danuser and colleagues evaluated the influence of stent size in two consecutive series of patients who had UPJO managed by antegrade endopyelotomy. In group 1 (77 patients), a 14/8.2-French graduated stent was used. In group 2 (55 patients), a 27-French catheter was used for 3 weeks, followed by the same 14/8.2-French graduated stent for 3 weeks. The early success rates after 6 to 8 weeks in groups 1 and 2 were 83% and 94%, respectively. The long-term success rates after 2 years were 71% and 93%, respectively, suggesting that the benefit in the group with larger stents was durable. Similarly, Wolf and colleagues evaluated 69 patients undergoing 77 endoureterotomies for ureteral strictures and found that for strictures longer than 1 cm, use of a stent sized 12 French or greater seems to be beneficial.
Series of retrospectives nonrandomized studies did not support any benefits from using larger stents. Comparing 14/7-French versus 8-French stents after endopyelotomy, Kletscher and colleagues found no statistically significant difference. Hwang and colleagues evaluated 40 patients after percutaneous endopyelotomy, and the difference between 6-French and 14/7-French stents was not statistically significant.
What about duration of stenting? The classic study of Davis still drives the empiric 6-week stenting time. In contrast, Mandhani and colleagues compared 57 consecutive patients who had primary UPJO randomized to undergo 7/14-French internal endopyelotomy stent placement for 2 weeks (group 1) and 4 weeks (group 2), and no difference was found in drainage pattern stent-related symptoms, suggesting that 6 weeks may not be required. Properly conducted studies are required to establish evidence-based guidelines for stenting practice after endopyelotomy.
Endopyelotomy for secondary ureteropelvic junction obstruction
Ng and colleagues evaluated 42 patients (mean follow-up of 47.7 months) who underwent management of failed primary intervention for UPJO. Secondary intervention included open operative repair (n = 20) or percutaneous (n = 11), ureteroscopic (n = 5), or retrograde cautery wire balloon endopyelotomy (n = 6). Long-term success rate of endoscopic treatment of secondary UPJO was 59.1% overall, including a 71.4% success rate after a failed open operative procedure and a 37.5% success rate after a failed endourologic procedure. Success of open operative salvage was 95% overall, including 94.1% after failed endourologic intervention and 100% after failed open operative intervention. In summary, endopyelotomy may be the optimal initial intervention after failed pyeloplasty but has a poor outcome after failed endopyelotomy.
Endopyeloplasty
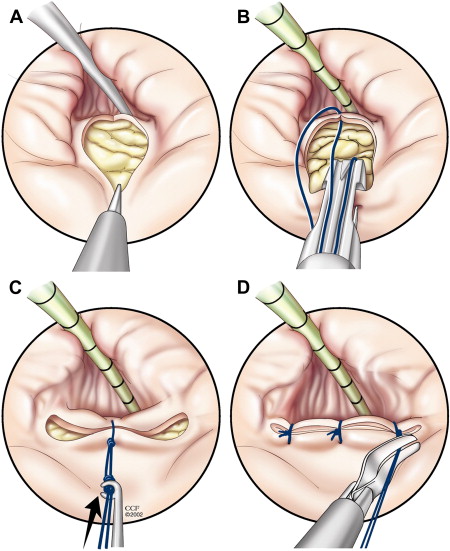
Endopyeloplasty consists of a Heineke-Mikulicz repair accomplished entirely through a percutaneous tract ( Fig. 1 ). In 1996, Oshinsky and colleagues reported percutaneous intrarenal suturing for the first time. Desai and colleagues reported the use of a laparoscopic suturing device through a 26-French nephroscope to perform endopyeloplasty (Fenger) in a porcine model. Technical feasibility was established, with a wider caliber of the UPJ after endopyeloplasty compared with endopyelotomy. Presumably, healing by primary rather than secondary intention accounts for this finding.