Vesicoureteral reflux (VUR) is a common problem in childhood, affecting approximately 1% to 2% of the pediatric population. Mild cases of VUR are likely to resolve spontaneously, but high-grade VUR may require surgical correction. Pediatric urologists are familiar with open antireflux operations, which can be accomplished with minimal operative morbidity. Minimally invasive endoscopic and laparoscopic techniques that now exist may serve to reduce morbidity further. This article reviews the endoscopic materials, techniques, and outcomes in the treatment of VUR in addition to the techniques and outcomes of laparoscopic and robotic ureteroneocystotomy.
Vesicoureteral reflux (VUR) is a common problem in childhood, affecting approximately 1% to 2% of the pediatric population . Mild cases of VUR are likely to resolve spontaneously, but high-grade VUR may require surgical correction. Pediatric urologists are familiar with open antireflux operations, which can be accomplished with minimal operative morbidity. Minimally invasive endoscopic and laparoscopic techniques now exist that may serve to reduce morbidity further. This article reviews the endoscopic materials, techniques, and outcomes in the treatment of VUR in addition to the techniques and outcomes of laparoscopic and robotic ureteroneocystotomy.
Endoscopic correction of vesicoureteral reflux
Materials used
Many injectable biomaterials have been produced as bulking agents for use in the endoscopic correction of VUR. For an injectable biomaterial to be ideal, it must be nontoxic and stable without migration to vital organs and cause minimal local inflammation while being well encapsulated by normal fibrous tissue and fibrocytes. It should be easy to inject through a rigid or flexible needle that passes easily through standard pediatric endoscopic equipment.
Polytetrafluoroethylene paste
Polytetrafluoroethylene (PTFE) paste is one of the most commonly used biomaterials in medicine. It is considered to be relatively inert chemically and biologically and has not been found to cause malignancy in humans. PTFE paste has been used as an injectable agent for the embolization of blood vessels and injection of vocal cords , and as a bulking agent for stress urinary incontinence (SUI) .
PTFE paste was first reported as a bulking agent for treatment of VUR in 1981 by Matouschek . This technique was popularized as the STING (subureteric transurethral injection) procedure by O’Donnell and Puri . Puri later reported on a large series of patients treated for VUR who demonstrated a 76% overall success rate after a single injection, which subsequently increased to 84.9% with repeat injection. PTFE paste was also used in a large European multicenter survey reporting on 6216 ureters in 4166 children with 10 years of follow-up. This survey reported a cure rate of 86% after one to four injections .
Despite its clinical effectiveness and widespread use in Europe, PTFE paste has never gained US Food and Drug Administration (FDA) approval because of concerns of distant particle migration. The rigid PTFE spheres have been found to migrate into the lymph nodes, lungs, liver, spleen, and brain in experimental studies . Subsequent clinical reports confirming particle migration have been reported, including a case with clinically significant particle migration to the lungs and another with migration to the lungs and brain . Because of these concerns and the availability of other injectable agents, the use of PTFE has been largely abandoned.
Polydimethylsiloxane
Polydimethylsiloxane (PDS) is a solid, silicone, elastomer, soft tissue bulking agent that has been incorporated into a patented medical device. It is made of 40% solid-textured highly cross-linked PDS elastomer spheres suspended in a 60% low-molecular-weight polyvinylpyrrolidone gel. It has been used clinically in treating SUI in women and men . The efficacy of this device for the correction of VUR has been well documented. Dodat and colleagues reported a success rate of 79.4% at 5 years of follow-up in 590 refluxing ureters in 389 patients. Herz and colleagues reported a success rate of 81% after a single injection and 90% after a repeat injection in 112 refluxing ureters. In a similar fashion, van Capelle and colleagues showed an 82.3% success rate in 311 ureters over a 10-year period from two European centers. Oswald and colleagues compared this PDS device versus dextranomer and hyaluronic acid copolymer and found similar results after a single endoscopic injection. Although the PDS device has demonstrated good long-term results, it has not received FDA approval for correction of VUR because of concerns about the potential for particulate migration, which has been demonstrated in one animal model study .
Collagen
Medical collagen is made of bovine collagen, which is a natural matrix protein commonly found in bone and connective tissue. It is commercially available in the injectable form as a solution of 95% type I collagen mixed with 5% type III collagen. Frey and colleagues reported a success rate of 63% after one injection in 204 ureters of 100 girls and 32 boys with varying grades of reflux. The success rate increased to 79.4% at 3 months after treatment after subsequent reinjection. Reunanen showed similar results, with a success rate of 82% in nonduplicated systems at 4 years of follow-up. Collagen, however, has been shown to lose volume over time, which has been correlated clinically with poor long-term results. Haferkamp and colleagues showed that only 9% of 57 treated units remained reflux free at 37 months of follow-up. There have also been reports of development of serum antibodies to bovine collagen . For these reasons, collagen has not been approved by the FDA for the treatment of VUR.
Calcium hydroxyapatite (coaptite)
Calcium hydroxyapatite has been used as a biocompatible implant for orthopedic and dental procedures in humans for more than 25 years . It was approved by the FDA for use in the treatment of SUI in women and girls in 2005. Mora Durban and colleagues showed resolution of reflux in 75% of cases with a single injection of calcium hydroxyapatite, with 85% resolution after a second injection. A recent prospective multicenter trial demonstrated ureteral cure rates of 46% and 40% at 1 and 2 years, respectively. At the primary center, however, the 2-year cure rate was 66% of patients and 72% of ureters . Merrot and colleagues compared dextranomer and hyaluronic acid copolymer and calcium hydroxyapatite in the treatment of VUR and found no significant difference in terms of cure rate, regardless of grade, in a total of 44 refluxing units. To date, however, calcium hydroxyapatite has not received FDA approval for the treatment of VUR.
Dextranomer/hyaluronic acid copolymer
The need for a nonimmunogenic, biodegradable, injectable bulking agent for the treatment of reflux prompted Stenberg and Lackgren to develop a system based on dextranomer microspheres suspended in a sodium hyaluronan solution in a 1:1 ratio. Dextranomer microspheres are made up of a network of cross-linked dextran polysaccharide molecules. After injection, the microspheres induce fibroblast and collagen deposition, leading to endogenous tissue augmentation. After 1 week, the microspheres disappear but the fibroblast and collagen ingrowth remains stable . They are nonimmunogenic because of the lack of free circulating dextran molecules and nonmigratory because of their spherical shape and larger particle size (80–120 μm) . After successful animal studies, these investigators injected 101 ureters in 75 consecutive patients and reported reduction or resolution of reflux in 81% of ureters at 3 months of follow-up. They followed 18 ureters for 1 year after treatment, and of these, 16 remained free of reflux . Dextranomer and hyaluronic acid copolymer was approved by the FDA in 2001 for the treatment of VUR in children and is now approved for treatment of VUR grades 2 through 4 .
Technique of injection
O’Donnell and Puri popularized the classic subureteric transurethral injection (STING) technique in 1984. General anesthesia is administered, a urine culture is obtained, and prophylactic antibiotics are given. Cystoscopy is performed before opening any injection materials in case the procedure is cancelled because of bladder inflammation or infection. Their original description suggested entering the bladder mucosa 2 to 3 mm distal to the ureterovesical junction (UVJ) and advancing the needle in the submucosal plane for a distance of 4 to 5 mm . To treat high-grade reflux and ureters without a submucosal tunnel, Chertin and colleagues suggested inserting the needle directly into the affected ureteral orifice to increase the length of the intravesical ureter and create a slit-like orifice. This modified STING procedure was popularized by Kirsch and colleagues , for which they described ureteral success rates significantly greater for the modified STING (92%) versus the standard STING (79%). They describe inserting the needle approximately 4 mm in the submucosa of the mid- to distal ureteral tunnel at the 6 o’clock position, all under the aid of hydrodistention.
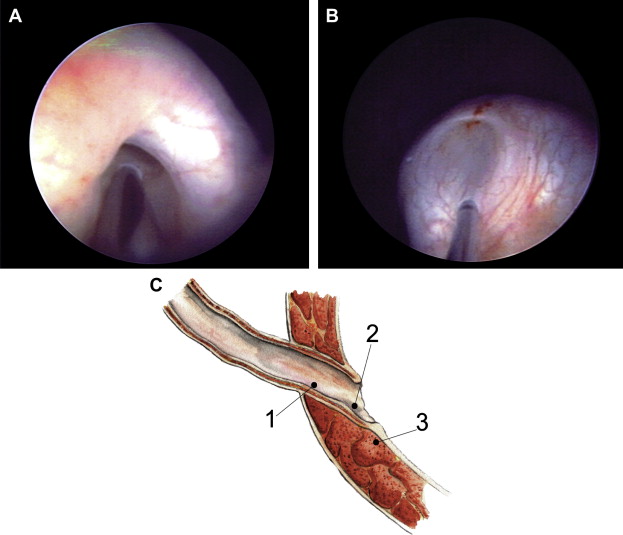
The hydrodistention-implantation technique (HIT) has evolved to now include two intraureteral submucosal injections proximal and distal HITs, or “double HIT,” until total ureteral tunnel coaptation occurs . The proximal HIT (site 1) should lead to coaptation of the proximal ureteral tunnel ( Fig. 1 A ). The distal HIT (site 2) is performed by placing the needle to the same depth just within the ureteral orifice and injecting until the ureteral orifice is coapted and elevated to the height of the ureteral tunnel (see Fig. 1 B). The end result should look like a mountain range appearance of the tunnel and orifice. If the ureteral orifice does not completely coapt with intraureteric injection, Kirsch recommends that a classic subureteric implantation (STING; see Fig. 1 C) be performed. In addition, he recommends that after each injection, an attempt at ureteral hydrodistention be done to ensure proper technique, because the ureter should remain coapted with irrigation.
Independent of the technique used, there exists a significant learning curve with endoscopic correction of VUR . Kirsch noted a lower success rate (60%) in his first 20 patients compared with an 80% success rate in his last 20 patients. Herz and colleagues reported a success rate of 46% in 28 refluxing ureters during the first 6 months of their study. In the remaining 18 months, the correction rate was 93% in 84 refluxing ureters. Lorenzo and colleagues reported that physician experience was predictive of VUR correction after endoscopic injection on multivariate analysis. This finding was confirmed by Routh and colleagues in their study of 301 patients.
Clinical results
At the present time, dextranomer and hyaluronic acid copolymer is the only FDA-approved material for use in endoscopic correction of VUR. The authors, therefore, limit their review to series using dextranomer and hyaluronic acid copolymer . Lackgren and colleagues published the first series using dextranomer and hyaluronic acid copolymer in 2001. A total of 221 patients (335 ureters, grades II–V) were followed 2 to 7.5 years. A voiding cystourethrogram (VCUG) was performed at 3 and 12 months after injections. They reported a 75% success rate (defined as grade I or less) at 1 year of follow-up. Puri and colleagues reported on 113 children (166 ureters) and found that reflux was corrected in 86% of ureters after a single injection, which increased to 99% after a second injection. Follow-up VCUG was performed at 3 months. Of the 113 patients, only 11 completed 1 year, and none had evidence of reflux on VCUG. This was followed up by a larger series in 2006, in which Puri and colleagues treated 692 children (1101 ureters) and reported success rates of 86.5% and 98% after first and second injections, respectively. In 2003, Kirsch and colleagues reported a 72% success rate after a single treatment at 3 months of follow-up. In a large series, Capozza and colleagues used dextranomer and hyaluronic acid copolymer to treat 788 patients (1050 ureters) endoscopically, and reported a success rate of 82% after a single injection. Kirsch and colleagues reported improved success rates in 459 ureters using a modified STING approach, with ureteral success rates greater for the modified STING (92%) compared with the standard STING (79%). Of the 8% who failed using the modified STING technique, a second injection resolved reflux in 88% of ureters that had grade I to III reflux . Please refer to Table 1 for a summary of results.
| Published report | No. children/ No. ureters | VUR grade | Technique | Longest clinical follow-up (years) | Success rate (%) | Long-term follow-up (months) |
|---|---|---|---|---|---|---|
| Lackgren et al | 221/335 | II–V | STING | 7 | 75 | 72 |
| Puri et al | 113/166 | II–V | STING | 1 | 86, 99 a | N/A |
| Kirsch et al | 180/292 | I–IV | STING | 1 | 72 | N/A |
| Capozza et al | 788/1050 | II–V | STING | 1 | 82 | N/A |
| Kirsch et al | 70/119 | I–IV | HIT | 1 | 92 | N/A |
| Puri et al | 692/1101 | II–V | STING | 3 | 86.5, 98 a | N/A |
Complex cases
Endoscopic injection of dextranomer and hyaluronic acid copolymer after failed ureteroneocystotomy has been reported. Kitchens and colleagues reported on 18 patients who had persistent VUR or de novo ipsilateral VUR after attempted VUR correction and primary nonrefluxing megaureter or renal transplantation, respectively. Of the 20 renal units, 16 (80%) had complete resolution of VUR after a single injection. Similarly, Jung and colleagues reported on dextranomer and hyaluronic acid copolymer injection for persistent VUR after ureteroneocystotomy, with a success rate of 70% and 90% after first and second injections, respectively. Chertin and colleagues reported on endoscopic treatment of reflux in patients who had undergone ureterocele puncture. Of the patients with reflux into the lower moiety, 31 (70%) of 44 and 40 (91%) of 44 had resolution of reflux after one and two injections, respectively.
In a multi-institutional study, Perez-Brayfield and colleagues reported on 72 patients (93 ureters) that they considered to be complex cases. Cases included persistent reflux after open surgery (n = 17), persistent reflux and neurogenic bladder (n = 11), ectopic ureters to bladder neck (n = 7), bilateral Hutch diverticulum (n = 6), stump reflux (n = 6), ureterocele after puncture or incision (n = 5), and ureteral duplication (n = 15). The overall success rate in their series was 68% after one endoscopic injection. Özok and colleagues performed endoscopic injection of dextranomer and hyaluronic acid copolymer in 21 renal transplant candidates (29 ureters) with reflux grades I through IV and reported success rates of 79.3% and 82.7% after one and two injections, respectively. They did not report any adverse effects.
Factors predicting success
It seems reasonable to state that dextranomer and hyaluronic acid copolymer injection is a safe and efficacious procedure, at least in the short term. What is less obvious, however, are what factors predispose patients to success or failure. Capozza and colleagues noted that uncontrolled voiding dysfunction contributed to endoscopic failure with dextranomer and hyaluronic acid copolymer in their series of 320 children. In contrast, Lackgren and colleagues reported that endoscopic treatment with dextranomer and hyaluronic acid copolymer was similarly effective in patients with and without bladder dysfunction (urge syndrome and dysfunctional voiding). The data demonstrating any affect of voiding dysfunction dextranomer and hyaluronic acid copolymer results, however, are weakened by the lack of standard assessment for voiding dysfunction. Lavelle and colleagues examined 52 patients (80 ureters) and found that mound morphology was the only statistically significant factor predictive of a successful outcome, using Fisher’s exact test. No difference was found in terms of volume injected or the presence or absence of voiding dysfunction. In a multivariate analysis on 168 patients (259 ureters), Yucel and colleagues found that reflux grade, volume of dextranomer/hyaluronic acid injected, and mound appearance correlated with outcomes. Factors not correlated with outcomes included gender, age, unilateral versus bilateral, ureteral duplication, subureteral versus intraureteral, and presence of voiding dysfunction. Further prospective studies are required to elucidate fully what determines outcomes in patients who undergo endoscopic correction of their VUR. Lackgren and colleagues retrospectively reviewed 68 children with duplex ureters and 40 children with a small kidney (contributing 10%–35% of total renal function) and found similar results when compared with their main study population.
Complications of endoscopic injection
Recently, Elmore and colleagues reported on new contralateral reflux after dextranomer and hyaluronic acid copolymer injection. Of 126 patients who underwent unilateral dextranomer and hyaluronic acid copolymer injection, 17 (13.5%) developed contralateral reflux on follow-up VCUG. They found that girls younger than 5 years of age had the highest incidence of new reflux. Similarly, in another series, de novo contralateral reflux was reported in 10 (8.3%) of 120 patients who had unilateral VUR . Menezes and colleagues reported that 10.1% of children developed new contralateral reflux after dextranomer and hyaluronic acid copolymer injection. They were unable to identify any risk factors and did not recommend prophylactic treatment of nonrefluxing contralateral ureters. As of yet, the natural history and clinical sequelae of new contralateral reflux have not been fully elucidated. In the future, high-risk groups may benefit from prophylactic injection of the contralateral side.
Ureteral obstruction after dextranomer and hyaluronic acid copolymer injection is a rare event. Snodgrass reported persistent asymptomatic obstruction of a dysmorphic ureter after dextranomer and hyaluronic acid copolymer injection that required open reimplantation. A recent multi-institutional review reported on 745 patients (1155 ureters) and found postoperative obstruction in 7 ureters (0.6%) in 5 patients (0.7%). Four of the 5 patients were immediately symptomatic with nausea or vomiting in 2 patients and anuria within 24 hours in 2 patients. All patients had resolution of symptoms with stent placement, with no recurrence after stent removal .
Cost-effectiveness
Costs are assuming increasing importance in health care, and costs of new interventions must be considered. Benoit and colleagues examined the cost-effectiveness of dextranomer/hyaluronic acid copolymer injection as a substitution to surgical management. They found that dextranomer and hyaluronic acid copolymer injection injection may be more cost-effective than ureteral reimplantation for children who meet standard criteria for surgical therapy, especially for lower grades of reflux. If an increased volume of dextranomer and hyaluronic acid copolymer injection is needed for higher grades of reflux, injection would then only be cost-effective for grades I and II unilateral and bilateral reflux, and possibly unilateral grade III reflux. Benoit and colleagues also compared the cost-effectiveness of performing dextranomer and hyaluronic acid copolymer injection at the time of diagnosis with that of traditional management. Two models were used: injection at diagnosis proceeding to traditional management if injection failed (scenario 1) and injection at diagnosis proceeding to ureteral reimplantation if injection failed (scenario 2). They found that in both scenarios, dextranomer and hyaluronic acid copolymer injection can never achieve cost-effectiveness for grades I and II unilateral and bilateral reflux and that high success rates of dextranomer and hyaluronic acid copolymer injection are needed to achieve cost-effectiveness for higher grades of VUR.
Follow-up
The current follow-up paradigm for endoscopic injection of dextranomer and hyaluronic acid copolymer injection is variable. Most clinical studies recommend renal and bladder ultrasound 2 to 4 weeks after surgery and VCUG at 3 months . Yu and colleagues believe that routine renal ultrasound scans are unnecessary after endoscopic injection of dextranomer and hyaluronic acid copolymer in uncomplicated cases of VUR. Because of the known risk for late recurrence, some advocate follow-up VCUG at 1 year, although few series document this type of long-term follow-up.
Laparoscopic and robotic ureteroneocystotomy
Ureteral reimplantation has proved to be the “gold standard” therapy for VUR. Traditional open ureterovesical reimplantation procedures have been extremely successful in children with success rates approaching 95% to 98% . Recent efforts have been directed toward reducing the perioperative morbidity of open reimplantation, however, including hematuria, irritative bladder symptoms, and postoperative pain. Initially described in the mid-1990s , laparoscopic antireflux surgery has never achieved popular consensus because of the technical difficulty in dissection and suturing required. Proposed advantages of the laparoscopic approach include better cosmetic results, shorter hospitalization, decreased analgesic requirement, faster recovery, and improved visualization. These theoretic advantages are not always easy to demonstrate in the pediatric population, however, and early outcomes have not demonstrated the laparoscopic approach to be as efficacious as the open ureteral reimplant.
Percutaneous trigonoplasty
An alternative to open and endoscopic injection procedures, the percutaneous endoscopic trigonoplasty was introduced in the early 1990s. A combination of intravesical cystoscopy and laparoscopy, the bladder is filled with carbon dioxide through percutaneously placed ports to improve visibility and the reimplant is performed using a Gil-Vernet or Cohen technique. First described by Okamura and colleagues in 6 children (mean age of 7 years) with grade II through V (bilateral reflux in 5 children), they reported a 100% reflux correction rate, a mean operative time of 149 minutes, and a mean postoperative catheterization time of 4.6 days. No major complications were observed at a median follow-up of 8.5 months. In a larger series of 22 children (mean age of 7 years) and 32 refluxing units (grades II–V), Cartwright and colleagues reported a reflux correction rate of 62.5%, with follow-up ranging from 4 to 11 months. Operative time ranged between 60 and 240 minutes, and complications included a vesicovaginal fistula, hyponatremia, and perivesical fluid collection. In an extension of this series, Gatti and colleagues reported outcomes in 29 children with 46 refluxing ureters using the Gil-Vernet and Cohen reimplantation techniques. Success rates improved from 63% to 83% with the Cohen technique, but the operative time nearly doubled as well. In a comparison of children and adults with reflux, Okamura and colleagues reported a 59% success rate in 15 children and trigonal splitting in 13%, causing recurrence of reflux greater than grade II. To improve success rates, this technique was modified to elongate the intramural ureter with reliable muscular backing. The initial success rate in 8 female children with 14 refluxing ureters was 86%, with a mean operative time of 245 minutes . Despite the proposed advantages of a reduction of postoperative urgency and a shorter recovery time, reduced success rates and increased operative times in these early series are clearly inferior to those of traditional open techniques and this procedure has largely been abandoned.
Pneumovesicoscopic cross-trigonal ureteroneocystotomy
In a more recent application of the pneumovesiscopic approach, the laparoscope is placed transabdominally instead of per urethra, which had previously limited mobility. First successfully described using a pig model , the increase in maneuverability facilitates a Cohen type cross-trigonal ureteral implantation using standard laparoscopic instruments ( Table 2 ). In 2001, Gill and colleagues described the use of this approach in 2 children and one adult demonstrating that this procedure was effective and technically feasible. Yeung and colleagues reported their initial experience with this technique in 16 children (mean age of 4.1 years) with 23 refluxing ureters. They reported a mean operative time of 136 minutes (112 minutes unilateral, 178 minutes bilateral), and an overall success rate of 96% with one conversion to an open procedure after displacement of a port into the extravesical space . In 32 children (mean age of 5 years), Kutikov and colleagues reported 93% and 80% success rates in ureters treated for primary VUR with the Cohen cross-trigonal technique and primary megaureter obstruction treated with the Glenn-Anderson technique, respectively. Complications included urine leak in 12.5% of patients and ureteral stricture in 6.3% of patients, with most occurring in children 2 years of age or younger with a bladder capacity less than 130 mL. In the most recent series, Canon and colleagues compared 52 children undergoing vesicoscopic ureteral reimplantation with 40 children undergoing open reimplantation. They reported a significantly decreased postoperative analgesic requirement in the vesicoscopic group and a similar hospital length of stay when compared with the open management group. The mean operative time was significantly elevated (199 versus 92 minutes; P = .001), however, with a higher complication rate (6% versus none), including 1 child with bilateral ureteral obstruction in the vesicoscopic group.
| Report | No. children No. ureters | VUR grade | Technique | Mean OR time (minutes) | Success (%) | Complications (%) |
|---|---|---|---|---|---|---|
| Okamura et al | 6/11 | II–V | G-V | 149 | 100 | Hematuria (16.7) Mechanical failure (16.7) |
| Cartwright et al | 22/32 | II–V | G-V | 60–240 | 62.5 | Vesicovaginal fistula (4.5) Hyponatremia (4.5) Perivesical fluid collection (4.5) |
| Okamura et al | 15/27 | II–V | G-V | 201 | 59 | Trigonal splitting (13.3) |
| Gatti et al | 29/42 | I–V | G-V, C | 60–240 (G-V) 197 (C) | 47 (G-V), 83 (C) | Vesicovaginal fistula (3.4) Hyponatremia (3.4) Perivesical fluid collection (3.4) Hydronephrosis (6.8) Bilateral pneumothoraces (3.4) |
| Tsuji et al | 8/14 | I–IV | G-V | 245 | 86 | Ureteral injury (14) |
| Yeung et al | 16/23 | II–V | C | 136 | 96 | Scrotal and suprapubic emphysema (12.5) Port displacement (18.8) |
| Peters et al | 6/12 | 2.3 | C a | 210 | 91.7 | Urine leak (16.7) |
| Kutikov et al | 27/54 | II–V | C | 168 | 92.6 | Urine leak (7.4) Ureteral stricture (3.7) |
| Canon et al | 52/87 | I–V | C | 199 | 91 | Urine leak (1.9) Bladder stones (1.9) Bilateral ureteral obstruction (1.9) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







