The surgical management of urolithiasis is an ever-changing discipline that presents unique challenges to the urologist. This article reviews the current minimally invasive treatment options for upper urinary tract urolithiasis. First it examines several factors that influence stone-free rates, including Hounsfield units of calculi, obesity, and lower pole factors. Surgical management of ureteral calculi is reviewed along with a discussion of stone management in high-risk patients including those who are pregnant. Surgical technique of shockwave lithotripsy, ureteroscopy, percutaneous nephrolithotomy, and laparoscopy is discussed in depth, with attention paid to possible variations in technique.
Since the first reported successful shock wave lithotripsy (SWL) treatment of a patient who had a renal stone in 1980 , urologists increasingly have employed minimally invasive techniques to treat patients who have ureteral or renal calculi. With over 25 years of experience in the techniques of SWL, percutaneous nephrolithotomy (PCNL), and ureteroscopy (URS), the amount of information available to objectively counsel a stone former on his/her treatment options can be overwhelming. This article reviews the recent literature that may affect surgical decision making for renal and ureteral calculi, including imaging and patient selection, and a step-by-step review of surgical minimally invasive approaches.
Factors influencing surgical stone-free rates
Hounsfield units—in vitro
Noncontrast, spiral CT has become the imaging modality of choice for assessing urinary stone disease, offering highly specific information such as stone location, size, number, density, and renal anatomy . Because larger cystine, brushite, and calcium oxalate monohydrate stones are known to be more resistant to SWL fragmentation , CT attenuation values of urinary calculi in Hounsfield units (HU) have been used to differentiate stone composition with some degree of success. In vitro studies have demonstrated that uric acid stones consistently have attenuation levels below 1000 HU, whereas calcium oxalate and phosphate stones usually exceed 1000 HU . Unfortunately, the range of HU values for calcium oxalate monohydrate and struvite stones overlap, suggesting that some stone compositions cannot be predicted reliably by CT . In addition, several studies have shown that stone size plays a role in HU density calculations. In the early 1980s, Parienty and colleagues found that stones of the same composition less than 5 mm in diameter had lower attenuation value than sized at 5 to 9 mm and proposed that the use of low-resolution beam collimation (5 mm) can yield artificially low attenuation values because of volume averaging . More recently, Saw and colleagues scanned 127 human calculi (ex vivo) and used a model, based on the physics of helical CT, to predict the effect of scan collimation width and stone size. As stone size decreased, HU for the same stone types also decreased, implying that smaller stones may decrease attenuation readings falsely and produce misleading results.
Hounsfield units—in vivo
Recently, correlating SWL success rates with in vivo CT HU attenuation levels has gained popularity. Joseph and associates studied 30 patients who had renal calculi undergoing SWL therapy using an electromagnetic lithotripter . Patients who had calculi less than 500 HU (n = 12) had 100% stone clearance and required a median of 2500 shocks. Those who had calculi of 500 to 1000 HU (n = 7) had a clearance rate of 86% and required a median of 3390 shocks. Patients who had calculi HU greater than 1000 (n = 11) had a clearance rate of 56% and required a median of 7300 shocks . Similarly, Gupta and colleagues used high-resolution CT protocols to report a linear relationship between calculus density and number of SWL sessions in patients who had renal and proximal ureteral stones. For stones less than 1.1 cm with HU less than 750, they reported that 34 patients had three or fewer SWL sessions and a stone-free rate of 90%. In patients who had HU greater than 750 and stone size greater than 1.1 cm, almost 80% required three or more SWL treatments with stone-free rates of only 60% . Two prospective trials have been published in this area. The first, Wang and colleagues in 2005, described three important patient factors on SWL multivariate analysis: stone burden greater than 700 mm 3 , stone density greater than 900 HU, and presence of nonoval (branched, irregular) stones. The second study, by El-Nahas and colleagues , found that stone density greater than 1000 HU and body mass index (BMI) were the only variables that predicted failure of renal stone disintegration using multivariate analysis. Leveraging the concept that stone morphology may be predictive of SWL fragility , this study is unique in that the authors use high-resolution bone windows to report stone size and narrow slide width protocols (1.2 mm versus 3.75 mm sections; stone HU calculated at lower, middle, and upper portion of stone versus one calculation) to predict a high-risk SWL failure group . In contrast, Pareek and colleagues analyzed 64 patients who had lower pole renal calculi sized 5 to 15 mm undergoing SWL and did not find HU to be an independent risk factor for stone clearance. Because their stone-free group had significantly smaller lower pole stone sizes before SWL ( P <.01), it is likely that stone size, stone density, and stone location, along with other patient factors are linked in the context of lower pole clearance rates. Further studies in the clinical area of HU and stone density, in particular lower pole stones, undoubtedly will aid in stratifying SWL outcomes.
Obesity—technical concerns
As the epidemic of obesity continues to grow in underdeveloped and developed countries, urologists increasingly will be presented with the therapeutic challenge of stone disease in patients who are obese and morbidly obese . Technically speaking, each different minimally invasive approach in obese patients who have stone disease brings about its own unique set of nuances. SWL may be limited in these patients, as their weight may exceed gantry or table limits; their size may exceed lithotripter focal length, or body habitus may prevent adequate stone visualization at the time of SWL . Proven to be just as safe and effective as in the nonobese population, PCNL in patients who are obese requires modifications in technique, specialized long equipment, and the ability of the patient to tolerate the prone position . Although no new equipment or techniques are required for the ureteroscopic approach, the patient must be able to tolerate general anesthesia and must be able to fit on the operating table without interfering with fluoroscopy . In addition, special attention to thromboembolic prophylaxis and prevention of pressure-induced iatrogenic injuries during prolonged dorsal lithotomy positioning may be warranted in the morbidly obese.
Obesity—shockwave lithotripsy concerns
Excluding positioning and technical concerns, the obese patient still may receive a suboptimal outcome after SWL. In 1994, Ackermann and colleagues first described BMI as an independent predictor of SWL failure using a Dornier HM-3 lithotriptor (Dornier MedTech, Kennesaw, Georgia). Their data suggested that patients who had BMI less than or equal to 28 had the best chance at successful SWL and implied that SWL failure in obese patients may be because of hampered stone targeting or dampened shock wave blast path. In two more recent studies using second-generation electrohydraulic lithotriptors, Portis and colleagues and Pareek and colleagues both reported a causal relationship between SWL failures and BMI. Because fat is distributed in different areas for different patients who have the same BMI, a quantitative measurement of the distance from the shockhead to the kidney was introduced in 2005, termed SSD or “skin to stone distance.” SSD is calculated by measuring three distances from the renal stone to the skin at the 0°, 45°, and 90° using radiographic calipers or a computational measuring device . The average of these values represents the SSD for a given stone. In a series of 64 lower pole stone patients undergoing SWL, Pareek and colleagues found that SSD greater than 10 cm was a more reliable predictor than either BMI or HU measurements alone for SWL failure. Conversely, El-Nahas and colleagues published their series of 120 patients who underwent SWL for solitary renal stones 5 to 25 mm in size. Although it was shown to be predictive of SWL stone disintegration failure by univariate analysis ( P = .033), SSD did not reach significance on multivariate analysis . Interestingly, BMI predicted need for more than three SWL sessions and disintegration failure reliably. Overall, as both imaging technology and patients’ abdominal girths expand, predicting SWL success by using surrogate markers, such as BMI, HU, or SSD, may lead to alternative stratification protocols.
Lower pole factors—shockwave lithotripsy
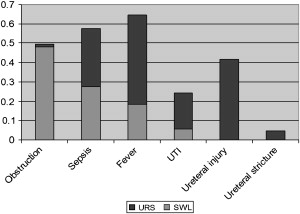
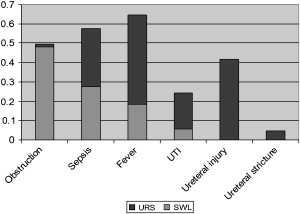
Although many different stone and patient factors play roles in the successful surgical management of upper tract urolithiasis, stones located in the lower pole of the kidney continue to be a challenge. In their meta-analysis, Lingeman and colleagues noted that between 1984 and 1991, the incidence of lower pole stones treated with SWL increased from 2% to 48% of all SWL cases. The authors investigated the outcomes of SWL for lower pole calculi and found that stone-free rates ranged from 25% to 84.6%, with a mean stone-free rate of 59.2%. This falls well short of the expected stone-free rates for middle and upper pole stones, which are estimated to be 70% to 90% . Outcomes were more favorable for patients who had stones less than 1 cm, with an overall stone-free rate of 74% for a single treatment as compared with patients who had stones 1 to 2 cm or greater than 2 cm (stone-free rates of 56% and 33%, respectively). These findings questioned the role of SWL in the management of larger, lower pole stones, and opened the door for numerous retrospective and prospective studies concerning the management of these calculi . A summary of the most recent lower pole stone-free success rates stratified by procedure type and stone size is listed in Fig. 1 . Where at all possible, stone-free rates are provided for single treatments, with the longest recorded follow-up based on strict CT criteria. Occasionally, mean stone size was used because of lack of individual stone size reporting. Multiple explanations have been offered for the poor stone-free rates in lower pole stones, including anatomic factors and the dependent position of the calculi limiting the passage of fragments from the kidney. The explanation to this mystery, however, is likely multifactorial.
In 2001, the Lower Pole Study Group published a prospective, randomized trial comparing SWL and PCNL for treating lower pole stones . One hundred twenty-eight patients who had symptomatic lower pole calculi were randomized to receive either PCNL or SWL. Overall, stone-free rates at 3 months were 95% for PCNL as opposed to only 37% for the SWL group ( P <.001). When stratified by stone size, it became evident that SWL success rates declined as stone size increased. The stone-free rates following SWL for stones 11 to 20 mm and 21 to 30 mm were 23% and 14%, respectively, as compared with 93% and 86% for PCNL. Retreatment and the need for auxiliary procedures were more common in the SWL group, while hospital stay was significantly longer in the PCNL group. Overall morbidity was not significantly different between the two groups. The authors concluded that stones greater than 10 mm in diameter are managed better initially with PCNL because of the higher stone-free rates and acceptable rate of morbidity. An advantage of this multicenter trial was the fact that eight different lithotriptors were represented, minimizing the machine-specific effect on the success and complication rates.
In 2005, Pearle and colleagues conducted a multicenter trial comparing SWL and URS for treating lower pole calculi less than or equal to 1 cm in diameter . There was no significant difference in stone-free rates for SWL and URS (35% versus 50%, P = .92). Additionally there was no difference in the number of patients requiring retreatment or ancillary treatments. Significant differences were found, however, regarding quality-of-life measures, with a more rapid return to driving, work, and overall shorter recovery time with SWL as compared with URS. In total, 90% of patients who underwent SWL would choose the procedure again as opposed to 63% in the URS group ( P <.05). Complication rates were not significantly different between groups. The results of this study seem to support SWL treatment over URS for stones 1 cm or less in diameter because of superior patient acceptance; however, the authors point out that many of the symptoms encountered by the URS group could be accounted for by the ureteral stent.
In an effort to improve poor outcomes, Pace and associates investigated the effect of mechanical percussion inversion (MPI) and diuresis on residual lower pole fragments following SWL . In total, 69 patients who had residual lower pole fragments 3 months following SWL were randomized to receive either MPI or observation for 1 month. The group receiving MPI had a significantly better stone-free rate than the observed group (40% versus 3%) and a greater reduction in total stone area (−63.3% versus +2.7%) in patients who were not free of stones. The authors concluded that MPI is a safe and effective adjunct to SWL in patients who have lower pole calculi, significantly improving success rates and reducing stone burden in SWL failures.
Lower pole factors—ureteroscopy
As with SWL, ureteroscopic management of lower pole stones is frequently challenging, with lower success rates than for stones located elsewhere in the kidney. Grasso and Ficazzola reported overall stone-free rates of 82%, 71%, and 65% in patients with lower pole stones measuring 10 mm or less, 11 to 20 mm, and greater than 20 mm, respectively, managed with retrograde ureteropyeloscopy . Several factors contribute to these poor success rates, including the difficulty of accessing the stone because of acute infundibular angles and reduced deflection in ureteroscopes associated with the passage of even small laser fibers. With the advent of small, flexible endoscopes and tipless nitinol stone baskets, many urologists have taken to relocating lower pole stones into a more favorable location before fragmentation. Kourambas and colleagues described the use of either a 3.2F nitinol basket or 2.6F nitinol grasper in 10 cases where access to the lower pole was inhibited by decreased ureteroscopic deflection. Fragmentation was achieved in all 10 cases after stones were manipulated into a more favorable location. Schuster and colleagues reviewed their experience in 78 patients undergoing ureteroscopy for lower pole stones . Success rates were significantly better in cases where stones were displaced into a more favorable location than in those where lithotripsy was performed in situ. This was statistically significant for stones measuring 1 to 2 cm, where only 29% of cases in the in situ group were successful compared with 100% success in the displacement group.
Although lower pole calculi continue to present challenges for the urologist, new technologies and improved techniques offer the promise of better success rates in these cases. As a general rule, lower pole calculi 1 cm or less are managed best initially with SWL when feasible, while most stones between 1 and 2 cm may be well managed with either URS or PCNL as primary therapy. Large calculi, especially those greater than 2 cm, have profoundly lower success rates in the lower pole and are managed best with PCNL when possible as this modality is influenced least by a lower calyceal location. As always, patient and stone factors, including comorbidities, anatomic factors, and stone composition, should be taken into account when choosing the treatment with the best chance of success.
Surgical management of ureteral calculi
Efficacy
The management of ureteral calculi has changed dramatically over the last 10 years because of an increased awareness and implementation of medical expulsive therapy (to facilitate ureteral stone passage) and advances in ureteroscope design and accessory instrumentation. In general, SWL remains the mainstay treatment for small (less than 1 cm) proximal stones. As stone size increases and as a stone moves distally, most authors agree that ureteroscopy is the more effective surgical approach. In early 2007, Nabi and colleagues summarized results from six published prospective, randomized controlled trials (PRCT) comparing URS head-to-head with SWL therapy for ureteral stones. Overall, stone-free rates were found to be lower in the SWL group (RR 0.84, 95% CI 0.73 to 0.96) with a trend toward lower retreatment rates in the ureteroscopy group (RR 3.34, 95% CI 0.82 to 13.62). Tables 1 and 2 summarize the results from the six PRCTs and several other recent publications in an attempt to stratify stone free rates (SWL and URS) based on stone size and ureteral stone location. If available, the stone-free rates are reported for single SWL or URS treatments. Retreatment rates and the time to complete stone clearance must be entertained when considering the value of SWL or URS.
| Therapy | <1 cm | >1 cm |
|---|---|---|
| Extracorporeal shockwave lithotripsy | 51% ; 91% ; 78% ; 85% ; 79% | 95% ; 54% |
| Ureteroscopy | 99% ; 91% ; 91% ; 93% ; 100% ; 97% ; 98% ; 88% | 100% ; 94% ; 89% ; 89% |
| Therapy | <1 cm | >1 cm |
|---|---|---|
| Extracorporeal shockwave lithotripsy | 78% ; 80% ; 60% ; 85% ; 70% | 32% ; 50% ; 45% ; 35% ; 43% |
| Ureteroscopy | 90% ; 100% ; 90% ; 91% ; 80% ; 91% ; 75% | 35% ; 93% ; 93% ; 77% ; 65% ; 71% ; 76% |
| Percutaneous nephrolithotomy | N/A (Most studies examine large stone burden) | 98% ; 86% ; 79% ; 94% ; |
Complications
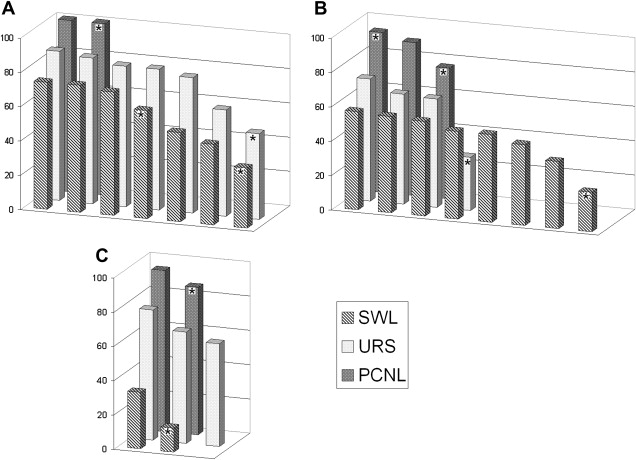
Perhaps the more difficult consideration for patients and urologists is the spectrum of potential complications that may accompany a given ureteral stone treatment. The rate of reported complications in the six PRCTs was lower in the SWL group (RR 0.48, CI 0.26 to 0.91) with a significantly lower rate of hospital stay , but no specific details on the exact type of complications were given, except to say that most were minor. This review reported that pain symptoms were higher, but not significantly so, in the stented ureteroscopy group . In a recent review of over 3000 procedures for ureteral stones (predominantly retrospective), significant complications for SWL and URS were 7% for each group . Eighty-seven SWL complications were recognized ( Fig. 2 ), with the most significant difference between URS coming in rates of acute ureteral obstruction (48% [42 oif 87] versus less than 1% 1 of 151]). Notably, the lack of ureteral obstruction in URS patients was likely because of stenting, but no objective measure of stent discomfort was included in this review. Within the URS group, 151 complications were recognized, with ureteral injury (63 of 151 complications, 41%) and ureteral stricture (7 151 complications) occurring exclusively in the URS (SWL group 0%, see Fig. 2 ) . It comes as no surprise that ureteral injuries occur more frequently during ureteroscopy, and many of the previously mentioned studies were performed with older lithotripsy options (electrohydraulic, pneumatic), large semirigid ureteroscopes, and variability in evaluation for and definitions of complications. Overall, the potential for complications must be balanced with the surgeon’s experience, type of anesthesia used, available equipment, efficacy, and potential for retreatment.
High-risk treatment groups—pregnancy and bleeding diathesis
Ureteral stones in pregnancy and in patients who have bleeding diathesis represent a high-risk group of stone patients in whom SWL or PCNL are absolutely contraindicated, leaving ureteroscopic lithotripsy as the only effective therapeutic alternative that treats the stone rather than temporizes the pain. Most calculi of pregnancy are eliminated with a combination of analgesia, rest, and hydration or are managed temporarily with the insertion of a ureteral stent or nephrostomy tube . When necessary, the ureteral dilation associated with pregnancy has been shown to facilitate passage of the ureteroscope , and several case reports of safe and effective ureteroscopy during pregnancy have been published . Indeed, with improvement in ureteroscopic instrumentation and technique, primary definitive ureteroscopic stone extraction can supplant the need for frequent stent changes during pregnancy. Care should be taken to minimize fluoroscopy time and fetal exposure during the case. For patients with ureteral stones who cannot safely stop therapeutic anticoagulation therapy, ureteroscopy also has been shown to be safe and effective. In a retrospective series of 25 patients who had significant alterations in bleeding times and international normalized ratio (INR), Watterson and colleagues successfully treated 18 of 19 (95%) ureteral stones with minimal morbidity.
Surgical management of ureteral calculi
Efficacy
The management of ureteral calculi has changed dramatically over the last 10 years because of an increased awareness and implementation of medical expulsive therapy (to facilitate ureteral stone passage) and advances in ureteroscope design and accessory instrumentation. In general, SWL remains the mainstay treatment for small (less than 1 cm) proximal stones. As stone size increases and as a stone moves distally, most authors agree that ureteroscopy is the more effective surgical approach. In early 2007, Nabi and colleagues summarized results from six published prospective, randomized controlled trials (PRCT) comparing URS head-to-head with SWL therapy for ureteral stones. Overall, stone-free rates were found to be lower in the SWL group (RR 0.84, 95% CI 0.73 to 0.96) with a trend toward lower retreatment rates in the ureteroscopy group (RR 3.34, 95% CI 0.82 to 13.62). Tables 1 and 2 summarize the results from the six PRCTs and several other recent publications in an attempt to stratify stone free rates (SWL and URS) based on stone size and ureteral stone location. If available, the stone-free rates are reported for single SWL or URS treatments. Retreatment rates and the time to complete stone clearance must be entertained when considering the value of SWL or URS.
| Therapy | <1 cm | >1 cm |
|---|---|---|
| Extracorporeal shockwave lithotripsy | 51% ; 91% ; 78% ; 85% ; 79% | 95% ; 54% |
| Ureteroscopy | 99% ; 91% ; 91% ; 93% ; 100% ; 97% ; 98% ; 88% | 100% ; 94% ; 89% ; 89% |
| Therapy | <1 cm | >1 cm |
|---|---|---|
| Extracorporeal shockwave lithotripsy | 78% ; 80% ; 60% ; 85% ; 70% | 32% ; 50% ; 45% ; 35% ; 43% |
| Ureteroscopy | 90% ; 100% ; 90% ; 91% ; 80% ; 91% ; 75% | 35% ; 93% ; 93% ; 77% ; 65% ; 71% ; 76% |
| Percutaneous nephrolithotomy | N/A (Most studies examine large stone burden) | 98% ; 86% ; 79% ; 94% ; |
Complications
Perhaps the more difficult consideration for patients and urologists is the spectrum of potential complications that may accompany a given ureteral stone treatment. The rate of reported complications in the six PRCTs was lower in the SWL group (RR 0.48, CI 0.26 to 0.91) with a significantly lower rate of hospital stay , but no specific details on the exact type of complications were given, except to say that most were minor. This review reported that pain symptoms were higher, but not significantly so, in the stented ureteroscopy group . In a recent review of over 3000 procedures for ureteral stones (predominantly retrospective), significant complications for SWL and URS were 7% for each group . Eighty-seven SWL complications were recognized ( Fig. 2 ), with the most significant difference between URS coming in rates of acute ureteral obstruction (48% [42 oif 87] versus less than 1% 1 of 151]). Notably, the lack of ureteral obstruction in URS patients was likely because of stenting, but no objective measure of stent discomfort was included in this review. Within the URS group, 151 complications were recognized, with ureteral injury (63 of 151 complications, 41%) and ureteral stricture (7 151 complications) occurring exclusively in the URS (SWL group 0%, see Fig. 2 ) . It comes as no surprise that ureteral injuries occur more frequently during ureteroscopy, and many of the previously mentioned studies were performed with older lithotripsy options (electrohydraulic, pneumatic), large semirigid ureteroscopes, and variability in evaluation for and definitions of complications. Overall, the potential for complications must be balanced with the surgeon’s experience, type of anesthesia used, available equipment, efficacy, and potential for retreatment.