Minimal Change Disease: Introduction
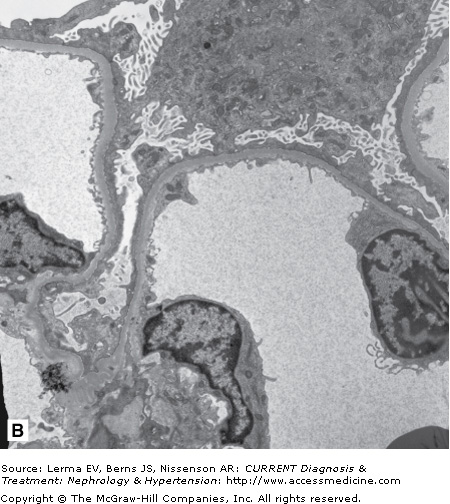
Minimal change disease (MCD) is a term used to describe the pathologic findings in a group of patients who present with heavy proteinuria, typically leading to nephrotic syndrome. On renal biopsy the findings include apparently normal glomeruli on light microscopy, negative immunofluorescence, and diffuse podocyte foot process effacement on electron microscopy. While occasionally MCD may be secondary to another condition such as lymphoma, in the majority of cases MCD is one of the idiopathic renal diseases. Because MCD is most likely to be the diagnosis in children presenting with the nephrotic syndrome, the majority of children do not undergo a kidney biopsy, but receive empiric treatment without one. Seventy percent of children with MCD present before age 5 years, and 20–30% of adolescents who present with nephrotic syndrome have MCD. Nevertheless, MCD is the third commonest finding in adults with nephrotic syndrome, after membranous nephropathy and focal, segmental glomerulosclerosis. The typical patient with MCD responds to therapy but experiences recurrent relapses.
Essentials of Diagnosis
- Heavy proteinuria, typically leading to nephrotic syndrome.
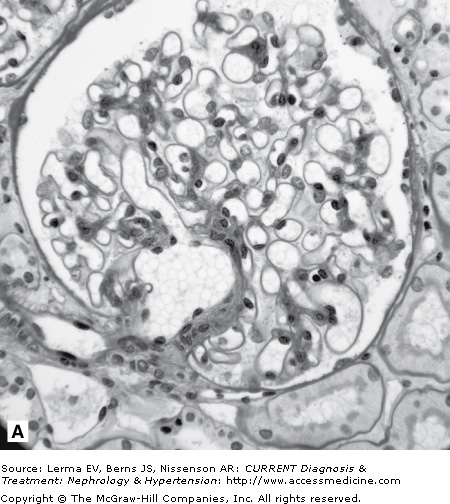
- Renal biopsy with minimal changes on light microscopy, negative immunofluorescent microscopy, and podocyte foot process effacement on electron microscopy (Figure 24–1).
- Usually there is no known etiology, although secondary MCD may be associated with neoplastic disease, toxic or allergic reactions to drugs, infections, autoimmune disorders, or other miscellaneous disorders.
General Considerations
MCD is the most common cause of nephrotic syndrome in children and the third most common cause of nephrotic syndrome in adults. In children the incidence of nephrotic syndrome is two to seven cases per 100,000 children and the prevalence is nearly 16 cases per 100,000. While most patients with MCD respond to therapy and have a good long-term prognosis, they are at risk for developing serious complications such as infection and thrombosis, and they are at risk for complications from therapy. The treatment of the MCD patient who is resistant to or dependent on corticosteroid therapy remains a challenge, despite the several therapeutic options available.
Pathogenesis
Since first postulated by Shaloub in the 1970s, the pathogenesis of MCD has been associated with the presence of a circulating factor capable of inducing proteinuria. Presumably, the circulating factor is secreted by lymphoid cells and functions as a vascular permeability factor or directly affects the function of the podocyte. The induction of remission by immunosuppressive medications further strengthens the argument that the circulating factor is secreted by immune cells whose function is inhibited by these agents. In addition, patients who develop end-stage renal disease from MCD or focal, segmental glomerulosclerosis (FSGS) are at risk for recurrent disease occurring rapidly after transplant. To date, the most promising candidate factors include hemopexin, interleukin (IL)-4, vascular endothelial growth factor (VEGF), low-molecular-weight (<100 kDa) non-Ig permeability factors, and heparanase. The isolation and identification of the pathogenic circulating factors currently remains a “Holy Grail” in nephrotic syndrome research.
Clinical Findings
The symptoms of MCD are related to the presence of nephrotic syndrome including peripheral swelling, abdominal discomfort from ascites, occasionally diarrhea from edema of the bowel wall, and, in extreme cases, pain from scrotal swelling and shortness of breath because of pleural effusions. Patients may experience oliguria, rarely leading to acute renal failure because of renal hypoperfusion. Because of an increased susceptibility to infection, especially from encapsulated bacteria, patients may present with signs of peritonitis or septic shock. They are also at an increased risk for thromboembolic phenomena, which may present with signs of deep venous thrombosis, flank pain and hematuria from renal venous thrombosis (rare), or a central nervous system catastrophe from a sagittal sinus thrombosis (also rare). An occasional patient has only minimal swelling.
Urinalysis in patients with MCD shows dipstick positive proteinuria (3+ to 4+); about 15% of patients with MCD also have microscopic hematuria. The urinary protein-to-creatinine ratio (in milligrams/milligram) is ≥3.5 and can be obtained on a random sample, alleviating the need for a 24-hour urine collection. As a consequence of the heavy proteinuria the patient develops hypoalbuminemia. The magnitude of proteinuria in MCD tends to be much greater than that seen in other glomerular diseases, leading to more profound hypoalbuminemia. Hypogammaglobulinemia may also be seen secondary to urinary losses of IgG or due to impaired immunoglobulin G (IgG) production and/or IgG catabolism in MCD. Children with MCD who have low IgG levels also have elevated IgM levels, changes in γ-globulins that may persist during periods of remission.
Renal function is typically normal, although there might be a minor increase in creatinine as a consequence of intravascular volume contraction. In severe cases, the hemoglobin and hematocrit will also be elevated from volume contraction, and platelets may also be elevated. Serum cholesterol and triglycerides are elevated and return to normal slowly after the induction of a remission. It is appropriate to draw a C3 complement level and an antinuclear antibody to rule out other causes of nephrotic syndrome; these will be normal in MCD.
Renal ultrasound is not necessarily indicated in nephrotic syndrome, but patients with MCD tend to have enlarged kidneys on ultrasound along with ascites fluid. A chest radiograph will be normal or may show pleural effusions.