Grade A
Grade B
Grade C
Serum bilirubin (μmol/L)
<34.2
34.2–51.3
>51
Serum albumin (g/L)
>35
30–35
<30
Ascites
(−)
Controllable
Refractory
Hepatic encephalopathy
(−)
Mild
Coma
Nutrition status
Good
Moderate
Poor
23.3 Indications
1.
Hepatic malignancy: Hepatoblastoma is the most common hepatic malignancy in children, and primary HCC also occurs in older children. Rhabdomyosarcoma, embryonic sarcoma, and leiomyosarcoma can also be diagnosed in pediatric patients. Most commonly originating from the retroperitoneal neuroblastoma or renal blastoma, hepatic metastases are resectable when they are confined within a single lobe with the resectable primary tumor.
2.
Hepatic benign tumor: Hemangioma and hemangioendothelioma are common, while teratomas are rare.
3.
Traumatic liver rupture: The liver is severely damaged, with over 50 % of the liver parenchyma, the intrahepatic major vessels, and the bile ducts being discontinuous with the uninjured portion. When uncontrolled bleeding after suturing, formation of intrahepatic hematoma, or complicated massive biliary hemorrhage occurs, hepatic lobectomy or hepatectomy should be considered.
4.
Chronic infectious lesions: Chronic liver abscess with thick walls, long-lasting fistula leftover from a drained liver abscess, an external fistula of bile duct, or hepatic tuberculosis.
5.
Hepatic cyst: Nonparasitic solitary hepatic cyst or follicular hepatic echinococcosis.
23.4 Contraindications
1.
Severe damage to multiple organs coexists.
2.
Widespread diseased lesions of the liver that are unresectable.
3.
Patients with primary hepatic cancer who simultaneously have jaundice, ascites, swelling, bleeding tendency, portal hypertension, or evident liver function damage.
23.5 Preoperative Preparation
1.
Whether the hepatic tumor is resectable should be determined, and hepatic metastasis should be excluded before the operation. A CT scan, which is an accurate noninvasive diagnostic method, is helpful in locating the tumor. CTA not only depicts the structure of liver vessels but also displays the features of tumor vessels. Ultrasonography is valuable in assessing the completeness of the inferior vena cava.
2.
Hepatectomy itself has a very large impact on metabolism, so careful assessment of homeostasis and electrolyte balance is necessary before the operation. The function of the heart, lungs, and kidneys also requires evaluation, except in emergent hepatectomy. Liver function evaluation is paramount in understanding liver compensation and estimating the volume of resectable liver.
3.
A high calorie and protein diet that is rich in fiber is recommended before the operation. An injection of vitamin K is also given. A transfusion of plasma or albumin or whole blood is given to patients with hypoalbuminemia.
4.
Oral antibiotics covering Gram-negative bacteria (first-generation cephalosporin) and those covering anaerobic bacteria (metronidazole) are given two days before the operation.
5.
Adequate fresh whole blood should be prepared before the operation.
23.6 Principles During Operation
A subcostal incision is sufficient to provide good visibility because children usually have a wide costal angle, a shallow abdominal cavity, and an elastic chest wall. Position: A supine position is used during left hemiliver resection. When right hemiliver resection or right triple segmentectomy is considered, the right side is elevated by 30° using a sandbag cushioned under the right shoulder and waist, with the right upper extremity resting on the headrest. Deep anesthesia is required to eliminate autonomous respiration and prevent air embolism when the liver is dissected, except in thoracotomy. A sufficient blood supply to the liver should be preserved during the operation. Hypothermic anesthesia is advocated in sophisticated hepatectomy to prolong the duration of blood supply blockage.
23.7 Surgery Type
23.7.1 Left Hepatolobectomy
1.
Incision: An incision across the right rectus abdominis or midline incision is frequently adopted. The incision is extended to the left of the xiphoid process, if necessary, which can be removed for better exposure. An oblique incision under the costal margin in the upper abdomen can be chosen due to the soft costal arch in children. If necessary, the incision can be extended to beneath the left costal margin, and the left rectus abdominis can be cut apart.
2.
Mobilization of the left lateral lobe: The left hemiliver requires mobilization before dissecting the hepatic hilum. The ligamentum teres hepatis is ligated and removed. The liver is pulled caudally using a clamp on the end of ligamentum teres hepatis. The hepatic falciform ligament has better exposure after the liver is pressed toward the vertebrae. The hepatic falciform ligament is cut apart along the anterior abdominal wall to the left coronary ligament, which is then removed. The superficial branches of the left hepatic vein and diaphragmatic vessels should be preserved. Better visualization can be obtained by pushing the stomach to the left lower side with a saline-soaked gauze pad. The left triangular ligament is occluded using two long-curved clamps, cut off and ligated close to the diaphragm.
During mobilization, over-traction of the left lateral lobe should be avoided, or the left hepatic vein might be lacerated. Finger pressure is used to stop bleeding once the left hepatic vein is lacerated where it is then clamped and sutured.
3.
Ligature of the left hepatic vein: The left hepatic vein is exposed and ligated when the liver parenchyma is cut apart left to the cranial end of the falciform ligament. The left hepatic and middle hepatic vein often meet and form a common trunk, which then joins the inferior vena cava (IVC). The posterior upper margin of the left hepatic vein, which is usually lying in the left coronary ligament, may directly join the IVC or merge with the middle hepatic vein before joining the IVC at the superficial surface of the left lateral lobe. Attention should be given so the middle hepatic vein and IVC are conserved. The left hepatic vein on the left wall of the IVC can also be separated following separation of the IVC. Then, the liver parenchyma should be bluntly dissected and separated along the left hepatic vein; the left hepatic vein is ligated inside the liver.
4.
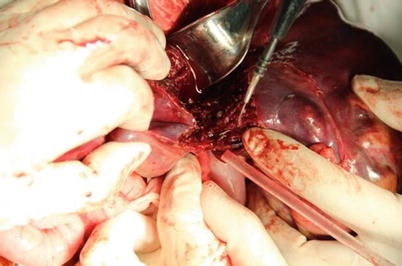
Left lateral lobectomy: The liver capsule is cut open 1–2 cm left of the falciform ligament after the blood supply to the left lateral lobe is occluded. The hepatic parenchyma is bluntly divided using a scalpel handle or forceps; vessels and bile duct are ligated if encountered (Fig. 23.1).
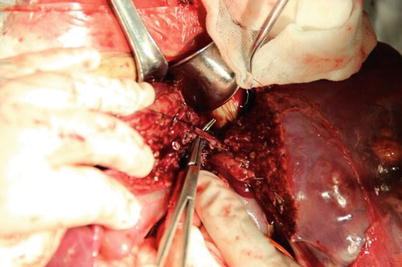
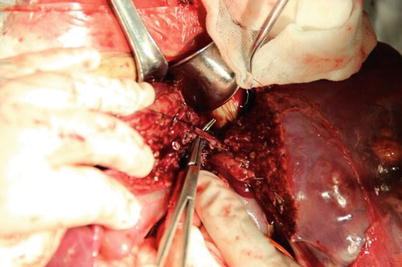
Fig. 23.1
Conduits inside the hepatic parenchyma are closed using suture or metal clips
5.
Management of hepatic cutting surface: Every vessel and bile duct termination along the cutting surface requires ligature with number 0 suture (Figs. 23.2 and 23.3). The bleeding points on the liver capsule are electrocauterized or ligated. The surgical area is rinsed and covered using normal saline. The cutting surface is covered by the remnant falciform ligament, hepatogastric ligament or even the great omentum using interrupted suture. Drainage is placed under the left diaphragm.