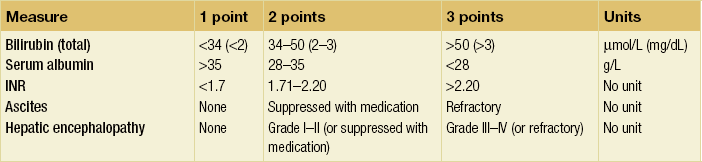
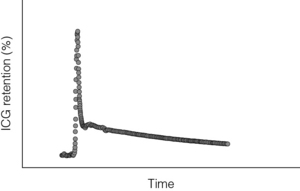
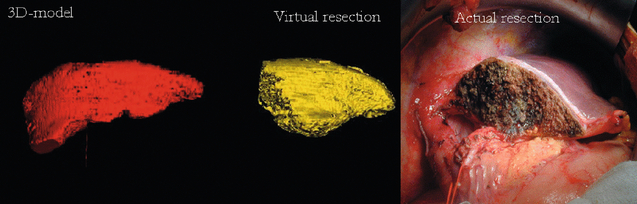
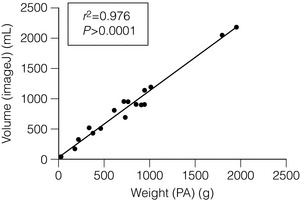
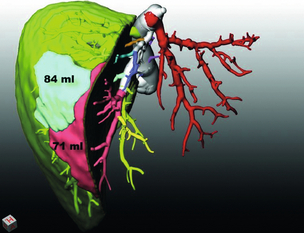
1 In the acute setting, liver failure can present with a number of symptoms, but it is important to note that not all of these may be present at the same time. Typically, a patient with acute liver failure after surgery, transplantation or in acute poisoning will be confused or mentally slow as a result of encephalopathy, which may progress to loss of consciousness and a need to protect the airway by intubation and mechanical ventilation. Patients are often not immediately jaundiced, but jaundice may develop over the course of several days. Patients may be hypoglycaemic and the requirement for intravenous infusion of dextrose is a sinister development and an indicator of severe acute liver failure. Coagulopathy may develop, with evidence of bruising or bleeding from line sites or surgical scars. Severe acute liver failure can be assessed using the King’s College Hospital criteria, which were designed to predict mortality in paracetomol- and non-paracetomol-dependent acute liver failure.1 Later, this scoring system was adopted in the UK to determine criteria indicating likely benefit from liver transplantation. In the surgical patient, the development of acute liver failure is usually more gradual and less dramatic; a useful scoring system for liver dysfunction in the acute setting has been reported by Schindl et al.2 (see Box 1.1). The second crucial problem has been that there is only a poor correlation between volume and function. However, it is still unclear why some patients with smaller hepatic remnants do not develop liver failure whilst some with greater residual volumes do. These observations suggest, however, that peri- and intraoperative events superimposed on the innate hepatic capacity to withstand injury play a role. Hepatic insufficiency in this situation may arise either if not enough liver volume is left after partial hepatectomy or if the residual volume does not function properly. A functional limitation may arise, for example, in patients that have received aggressive chemotherapy in order to reduce the number and size of metastases prior to surgical treatment by liver resection. One of the factors contributing to defective defence may be preoperative fasting,3 but equally prior chemotherapy and pre-existent steatosis may play a role. A third important aspect is that during liver surgery deliberate hypotension and temporary hepatic blood inflow occlusion (the so-called Pringle manoeuvre) are used by many surgeons to reduce blood loss during liver surgery (15 minutes ischaemia, 5 minutes reperfusion (15/5 Pringle)). Other surgeons do not use this manoeuvre, assuming that it causes oxidative stress and ischaemia/reperfusion (I/R) injury.4,5 There is little doubt that this procedure does cause oxidative stress and I/R injury; however, the consequence of this is variable. In a situation where defence mechanisms against oxidative stress are deficient it may adversely affect liver function. In this situation hepatic steatosis may constitute an additional predisposing factor to damage by ischaemia/reperfusion. In this situation it is assumed that defence mechanisms against oxidative stress are adequate and are indeed enhanced by short-term I/R injury.7 The Child–Pugh score for chronic liver disease8 has served as a useful means of categorising patients based on the severity of their liver disease. It employs five clinical measures of liver disease and each measure is scored 1–3, with 3 indicating the most severe derangement (Table 1.1). Liver failure gives rise to multiple abnormalities in nitrogen metabolism, some of which are thought to play a crucial role in the characteristic syndrome of hepatic encephalopathy that accompanies liver failure. Hepatic encephalopathy is a reversible neuropsychiatric syndrome, with a probably multifactorial cause.9 The current belief is that ammonia is one of the key components in the aetiology of hepatic encephalopathy10 because liver failure is usually associated with moderate to severe hyperammonaemia. Hyperammonaemia leads to increased brain uptake of ammonia, followed by detoxification of ammonia in the brain by coupling to glutamate to form glutamine. This process consumes glutamate (an important excitatory neurotransmitter) and leads to the formation of glutamine, which acts as an osmolite causing brain oedema. These changes in plasma levels were thought to be caused by increased BCAA catabolism in muscle and decreased AAA breakdown in the failing liver.14 A reduction in the insulin–glucagon ratio in this situation may play a key role in disturbing the balance between anabolism and catabolism. Accumulation of AAAs in the circulation in combination with the increased breakdown of BCAAs, particularly in skeletal muscle, would, according to this hypothesis, give rise to a decrease in the BCAA to AAA ratio, the so-called Fischer ratio. The increase in plasma AAAs in combination with increased blood–brain barrier permeability for neutral amino acids has been suggested to contribute to an increased influx of AAAs in the brain, since they compete for the same amino acid transporter. This, in turn, would lead to imbalances in neurotransmitter synthesis and accumulation of false neurotransmitters such as octopamine in the brain, which may contribute to hepatic encephalopathy.15 Advances in imaging have permitted the development of in vivo imaging of the liver. Three-dimensional models of the liver can be constructed from computed tomography (CT) or other cross-sectional imaging modalities, such as magnetic resonance imaging (MRI). The volume of the liver can then be calculated based on known separation of image slices combined with planar mapping of cross-sectional areas. In addition, such three-dimensional computer models can be simulated to map the effects of surgery by performing virtual hepatic resection, and studies have demonstrated that there is a good correlation between computer modelling and actual resection weight of surgical liver specimens (Fig. 1.1).2,16 Figure 1.1 Three-dimensional reconstruction of the liver preoperatively (red) showing tumours (green). Computer prediction of residual liver volume based on virtual hepatectomy of 3-D model (yellow) and actual photograph of resection showing residual liver segments. Reproduced from Schindl MJ, Redhead DN, Fearon KC et al. The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut 2005; 54:289–96. With permission from the BMJ Publishing Group Ltd. This technology is useful as a research tool because it allows liver function to be put into the direct context of the volume of functioning liver tissue. In addition, this technology is useful for predicting the need for reconstruction of venous territories of the liver in split liver transplantation. Usually, liver volumetry is performed on software directly linked to the hardware MRI or CT. In recent years, however, stand-alone software has become available, which makes it possible to perform hepatic volumetry remote from the radiological hardware. Examples of such software are the freely downloadable program ImageJ (for Windows-based PCs) and OsiriX (for Apple Macintosh). Our group has recently shown that the ImageJ software is very useful in measuring liver volumes in patients referred with a CT undertaken in the referring centre17 (Figs 1.2 and 1.3). Figure 1.2 Correlation between volume of resection calculated with ImageJ and actual measured weights of the resection specimens (n = 15, Pearson’s test).14 Reproduced with permission from World J Surg. Figure 1.3 Mapping the territory of the right hepatic lobe drained by the middle hepatic vein. The numbers represent the volumes of the territories at risk if segment 5 and 8 tributaries of the middle hepatic vein were not reconstructed in a potential right lobe living-donor liver transplant. Image reproduced with permission of MeVis imaging technologies, Bremen, Germany Kindly provided by H. Lang and A. Radtke, Plainz, Germany. Biochemical markers of true liver function vary depending on whether acute or chronic liver failure or injury is being considered (Table 1.2). Table 1.2 Blood tests useful to assess function in acute and chronic liver injury ICG is a compound that is used widely to measure liver function. It is rapidly cleared from blood by hepatocytes and is excreted into bile without enterohepatic circulation. Hepatocytes are so effective at clearing ICG from the circulation that the major limiting factor to its clearance is liver blood flow. This is thought to be reduced in cirrhosis. ICG clearance can be measured as ‘disappearance’ from the blood or can also be measured as accumulation in bile. Liver dysfunction is suggested by a slower rate of clearance from the blood and is usually expressed as percentage retention at 5 or 15 minutes after injection. Continuous measurement of ICG clearance can also be performed, which offers the potential improvement in accuracy by measurement of area under the clearance curve (Fig. 1.4). In some centres ICG clearance is routinely performed during preoperative work-up with cut-off values set for which patients are ‘safe’ to proceed to resection. However, there is no evidence to suggest that outcomes are improved in centres that use this test compared to centres that do not. In chronic liver disease, discriminative ability of ICG clearance is greatest in those with intermediate to severe liver failure. Addition of this test to the MELD score (Model for End-stage Liver Disease) can improve prognostic accuracy for patients with intermediate to severe liver dysfunction.18 However, given the relationship with hepatic blood flow, caution should be exercised when interpreting ICG clearance in the context of abnormally high cardiac output. Using a radiolabelled tracer that is eliminated exclusively by the liver, such as [99mTc]mebrofenin, blood clearance and hepatic uptake can be measured using a gamma camera to provide an indication of hepatic function. Hepatobiliary scintigraphy may improve predictive value compared to future liver remnant volume, especially in patients with uncertain quality of liver parenchyma.19 However, HBS has not been widely used preoperatively, there is no evidence that it outperforms ICG clearance and the requirement for a nuclear medicine facility on-site may limit its application.
Liver function and failure
Symptoms of liver failure: acute and chronic
Common causes of acute liver failure: hepatic insufficiency following liver resections
Chronic liver failure
Metabolic liver function
Measuring liver volume
Blood tests of liver function
Acute
Chronic
Albumin
−
+++
Prothrombin time
+++
+++
Bilirubin
+
+++
Lactate
++
−
Glucose requirement
++
−
Ammonia
+
+
Tests of liver function measuring substance clearance
Indocyanine green (ICG)
Hepatobiliary scintigraphy
Liver function and failure