Laparoscopic Transabdominal Preperitoneal Inguinal Hernia Repair
Antonio Garcia-Ruiz
Alejandro Weber-Sanchez
Anatomy
Being the site of highest incidence of abdominal hernias that require surgical management, the groin is one of the most relevant anatomical regions for the laparoscopic surgeon (Fig. 15.1). The groin is limited cephalically by the horizontal plane passing through the anterior superior iliac spine, medially by the midline, and inferolaterally by the inguinal ligament (running from the superior iliac spine to the pubic symphysis). In our judgment, the laparoscopic surgeon does not face an anatomical view more complex than the anterior approach. Instead, he or she observes the same anatomical structures from a different perspective, which may not be familiar to all. Nonetheless, detailed knowledge of this anatomical aspect is essential to safe and effective laparoscopic repair.
The anatomy of this zone has few variants; the reference points are mostly constant and can be summarized in relatively simple terms. Observed from inside the abdomen with the peritoneum intact, the lower part of the anterior abdominal wall is usually divided into three fossae, separated by the same number of folds or ligaments formed by different protruding structures. These may be more or less evident, depending on the patient’s constitution and the quantity of preperitoneal fat. On the midline we find the urachus, also called median umbilical ligament. Lateral to the urachus is the lateral umbilical ligament, usually the most prominent of the three folds. This ligament is a remnant from the obliterated umbilical artery leading from the iliac artery toward the navel. Finally, the most lateral fold, corresponding to the deep epigastric vessels, is the least prominent. The most common classification of the inguinal hernias still uses these three folds as reference points. Indirect inguinal hernias are those that protrude laterally to the epigastric vessels (Fig. 15.2), direct inguinal hernias are those that are medial to them (Fig. 15.3), and supravesical hernias are those protruding in between the median and lateral umbilical ligaments. Femoral hernias are located below this plane, in a position inferior to the iliopubic tract and through a space around the femoral sheath. On very rare occasions, we have found obturator hernias (defect of the obturate membrane of the iliac bone). Due to
their anatomical location, these hernias are not considered inguinal hernias. However, we have approached and managed them laparoscopically with almost the same principles as inguinal hernias, except that we shape the prosthetic mesh to fully cover the hernial defect, in this case considerably deeper into the pelvic space.
their anatomical location, these hernias are not considered inguinal hernias. However, we have approached and managed them laparoscopically with almost the same principles as inguinal hernias, except that we shape the prosthetic mesh to fully cover the hernial defect, in this case considerably deeper into the pelvic space.
The transabdominal preperitoneal laparoscopic hernioplasty requires elevating a very wide peritoneal flap. In order to do so, it is of outmost importance to recognize and be familiar with the extraperitoneal spaces of the pelvis. Medially, between the peritoneum and the trasversalis fascia, is the space of Retzius, which has a variable quantity of fat.
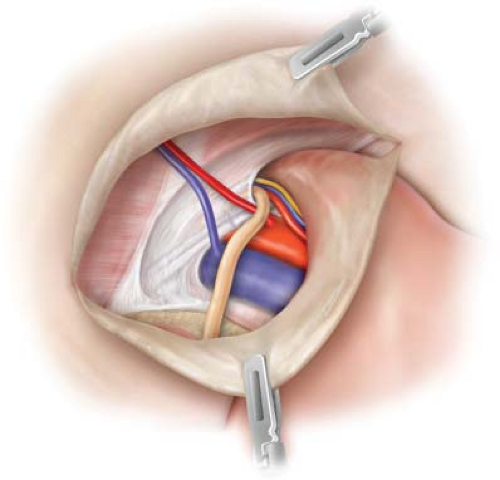
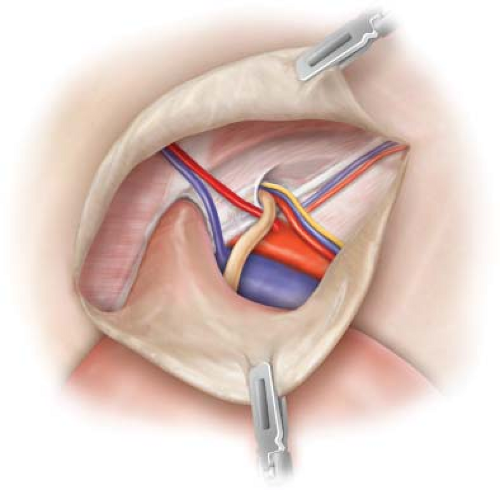
Usually it is an avascular space, except in the lower part which contains the venous anastomoses between the obturate, epigastric, and iliopubic vessels. From this perspective behind the wall it is impossible to observe the inguinal ligament which is in an anterior position concealed by the muscles of the abdominal wall. However, Cooper’s ligament is visible in this space. Even in obese subjects with large quantities of fat it can be palpated with laparoscopic instruments as a hard edge. This important reference point is located 1 cm medial and inferior to the origin of the epigastric vessels. Also visible in this space is the iliopubic tract, a band of thickened fascia running parallel to the inguinal ligament, is attached to the superomedial part of the pubic bone medially and laterally its fibers are dispersed with the trasversalis fascia and the iliac fascia, with no attachment to the iliac spine. Through the intact peritoneum, it is possible to identify the round ligament in females and the vas deferens in males. Both have a trajectory running from the deep part of the pelvis upward and from inside outward, to exit the abdomen through the internal inguinal orifice crossing the epigastric vessels. In males, the spermatic vessels, which have a downward trajectory, join at an obtuse angle with the deferent conduct, and also exit through the internal inguinal orifice, to form outside it, with the fasciae and muscular fibers enveloping it, the spermatic cord. On joining in the internal inguinal orifice, the gonadal vessels and the iliac vein form a triangle with its apex upward, area of the iliac vessels; this anatomical area, called “triangle of doom,” as well as the so-called “triangle of pain,” located between the anterior superior iliac spine and the gonadal vessels, warrants special attention. Familiarity with these two regions is crucial during laparoscopic inguinal hernioplasty because they are areas with high potential for severe complications such as transoperative vascular lesions or painful postoperative sequelae.
Usually it is an avascular space, except in the lower part which contains the venous anastomoses between the obturate, epigastric, and iliopubic vessels. From this perspective behind the wall it is impossible to observe the inguinal ligament which is in an anterior position concealed by the muscles of the abdominal wall. However, Cooper’s ligament is visible in this space. Even in obese subjects with large quantities of fat it can be palpated with laparoscopic instruments as a hard edge. This important reference point is located 1 cm medial and inferior to the origin of the epigastric vessels. Also visible in this space is the iliopubic tract, a band of thickened fascia running parallel to the inguinal ligament, is attached to the superomedial part of the pubic bone medially and laterally its fibers are dispersed with the trasversalis fascia and the iliac fascia, with no attachment to the iliac spine. Through the intact peritoneum, it is possible to identify the round ligament in females and the vas deferens in males. Both have a trajectory running from the deep part of the pelvis upward and from inside outward, to exit the abdomen through the internal inguinal orifice crossing the epigastric vessels. In males, the spermatic vessels, which have a downward trajectory, join at an obtuse angle with the deferent conduct, and also exit through the internal inguinal orifice, to form outside it, with the fasciae and muscular fibers enveloping it, the spermatic cord. On joining in the internal inguinal orifice, the gonadal vessels and the iliac vein form a triangle with its apex upward, area of the iliac vessels; this anatomical area, called “triangle of doom,” as well as the so-called “triangle of pain,” located between the anterior superior iliac spine and the gonadal vessels, warrants special attention. Familiarity with these two regions is crucial during laparoscopic inguinal hernioplasty because they are areas with high potential for severe complications such as transoperative vascular lesions or painful postoperative sequelae.
Given that in the early days of laparoscopic hernia repair nerve injuries were among the most serious complications due to the intense pain and disability they caused, knowledge of the nerve structures present in the zone is crucial. The nerves with greatest risk of injury are the lateral femoral cutaneous nerve and the femoral and genital branches of the genitofemoral nerve. Both follow almost parallel trajectories always positioned inferior to the iliopubic tract. The most medial is the genitofemoral nerve; from its origin in the lumbar region it crosses the psoas muscle and exits through the anterior face of that muscle near its inner edge. It then descends, covered by the fascia of the same muscle, and is positioned in front of the external iliac artery. At this point it divides into its two terminal branches: One genital and the other crural. The genital branch penetrates the inguinal duct, while the crural branch exits the abdominal cavity and passes below the inguinal ligament, accompanying the anterior face of the femoral
artery. The femoral cutaneous nerve descends on the anterior face of the psoas muscle, continues downward behind the fascia on the anterior face of the iliac muscle, and exits the abdomen below the iliopubic tract, very close below the anterior superior iliac spine. Usually, the voluminous femoral nerve is not observed during dissection of this region; however, it is important to bear in mind that it is between the psoas muscle and the iliac muscle—lateral to the external iliac artery and separated from it by the iliopubic tract—to avoid injuring it when dissecting more deeply in this area.
artery. The femoral cutaneous nerve descends on the anterior face of the psoas muscle, continues downward behind the fascia on the anterior face of the iliac muscle, and exits the abdomen below the iliopubic tract, very close below the anterior superior iliac spine. Usually, the voluminous femoral nerve is not observed during dissection of this region; however, it is important to bear in mind that it is between the psoas muscle and the iliac muscle—lateral to the external iliac artery and separated from it by the iliopubic tract—to avoid injuring it when dissecting more deeply in this area.
The crural region, where the iliac vessels cross, is limited above by the iliopubic tract, below by Cooper’s ligament, medially by Gimbernat’s lacunar ligament, and laterally by the psoas muscle. Finally, it is also highly advisable to recognize the importance of the spermatic fascia and dissect it carefully, to avoid injury to the genito-reproductive apparatus in male patients. The surgeon must have a very clear understanding of this region to develop the ample space that will house the prosthetic mesh and will be the support for a successful repair.
Clinical Presentation and Diagnosis
Diagnosis of an inguinal hernia is usually simple. It is based fundamentally on clinical aspects, and requires only a detailed clinical history and an adequate physical examination. Once established, there is no need for additional diagnostic or image studies. However, the evident clinical signs of a reducible, painful inguinal mass, with occasional signs of entrapment or with signs of intermittent intestinal obstruction are not always found. In such cases, a much more meticulous or sophisticated evaluation is required. Examples include the patient who seeks medical attention due to chronic or recurrent inguinal pain without an evident mass or hernial defect, in whom the Valsalva maneuver causes inguinal pain, but does not cause protrusion of tissues in the groin, or the morbidly obese patient who complains of nonspecific inguinal discomfort which can be particularly difficult to diagnose. In such patients, image studies (USG, CT, or even NMR) may help to document the presence of a hernia. Notwithstanding, even those studies may not be 100% sensitive or specific. Similarly, there may be patients with masses in the inguinal region that do not coincide with the usual sites for hernias and may be due to defects over prior surgical scars (cesarean section or prostatectomy) or uncommon true hernias such as supravesical or Spiegel’s hernias. Occasionally, a patient may present symptoms of acute intestinal obstruction because an intestinal loop has become trapped in the hernial orifice. In such cases, the surgeon will have to rely on image studies such as ultrasound, computerized axial tomography, and magnetic resonance or may even recur to laparoscopic exploration to achieve a more accurate diagnosis on the basis of which to plan the best possible surgical treatment for the patient. When laparoscopic examination confirms the presence of a hernia with peritoneal sac, there is no doubt that a laparoscopic inguinal hernioplasty should be performed. However, we have found cases where the peritoneum does not present hernial defect. In such cases, we have opted specifically to explore the corresponding inguinal region performing peritoneal dissection as described below, as in most of these cases we have found lipomas of varying size accompanying the spermatic cord or extending through the space between the femoral sheath and the corresponding blood vessels. The presence of such lipomas obliterates the hernial defect and makes the peritoneum appear intact during diagnostic laparoscopy. Another finding we have seen in rare cases is the presence of inguinal adenopathies which are distinguished laparoscopically by their greater consistency. In such rare cases, we recommend taking a tissue sample for histopathologic study without resection, as it could condition postoperative lymphedema.
Treatment
To date, the only definitive treatment for inguinal hernias is surgery. However, recently published studies have evaluated conservative medical management for reducible and relatively asymptomatic inguinal hernias. Most cases of inguinal hernia can be surgically treated on an elective basis.
In the case of an incarcerated inguinal hernia, treatment should be started immediately due to the risk of necrosis and intestinal perforation. In such cases, in the emergency ward, parenteral hydration and reclining the patient in the Trendelenburg position may allow the trapped intestinal loop to be released and management may then be semi-elective. However, some patients will require hospitalization and nasogastric decompression in an attempt, still conservative, at emergency management. If the patient’s clinical status worsens or conservative management does not produce results in a period of 48 to 72 hours, surgery will be the most indicated option. The decision to approach the case by laparoscopy or by conventional means should be based on the conditions of the patient and the experience and capabilities of the surgeon (see section on “Transoperative Complications”).
With very few exceptions, the indications for the transabdominal preperitoneal laparoscopic approach are the same as for conventional hernioplasty (by anterior approach). With considerable satisfaction, in recent years we have observed a strongly justified tendency to refer recurrent inguinal hernias for laparoscopic management. However, some cases may constitute a contraindication, relative or absolute, to the laparoscopic approach.
Patient does not tolerate capnoperitoneum (severe cardiopathies or severe neumopathies, for example).
Strangulated and perforated inguinal hernia with intercurrent sepsis.
Patient with severe ascitis.
Recurrent inguinal hernia following prior laparoscopic treatment.
Patient under age 15 years—pediatric.
Pregnancy, after the second trimester.
Patients with severe clotting disorders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree