Chapter 27 Interventional endoscopy
Technical aspects
Overview
The field of therapeutic biliary and pancreatic endoscopy has evolved rapidly since the first reports of endoscopic sphincterotomy in 1974. A spectrum of interventional procedures has gained widespread acceptance as therapeutic alternatives to operative management (Table 27.1; Brugge & Van Dam, 1999). The minimally invasive nature of endoscopic retrograde cholangiopancreatography (ERCP) coupled with its ability to be performed under conscious sedation have resulted in its rapid dissemination around the world. Refinements in procedural technique and improvements in accessory equipment have improved results and safety. This chapter focuses on these technical advances. The indications, contraindications, and complications of interventional biliary and pancreatic endoscopy are presented elsewhere (see Chapter 14, Chapter 18, Chapter 36, Chapter 37, Chapter 50D, Chapter 54, Chapter 63B ) and are not directly addressed here.
Table 27.1 Interventional Endoscopy in Biliary and Pancreatic Disease
Cannulation
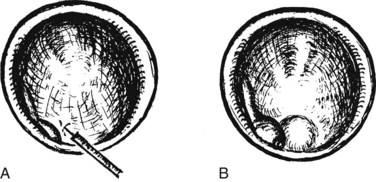
Selective cannulation of the bile and pancreatic ducts is a prerequisite for interventional procedures. Cannulation usually can be achieved with a standard cannulating catheter, using contrast injection to confirm successful cannulation. Use of a sphincterotome for cannulation has the advantage of enabling immediate sphincterotomy after cannulation. The sphincterotome also enables upward bowing in a caudocranial axis to assist in selective cannulation of the bile duct (Fig. 27.1). Wire-guided sphincterotome cannulation is associated with a lower rate of pancreatitis (Lee et al, 2009).
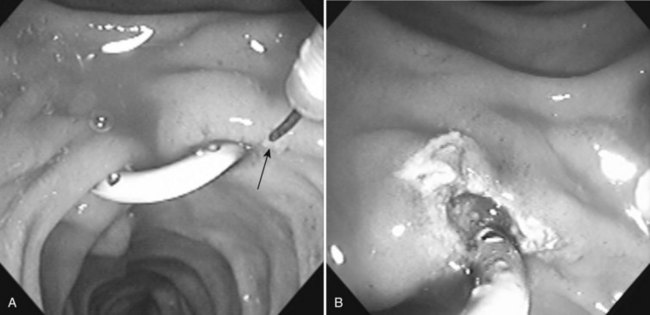
If free cannulation with a cannulating catheter fails, guidewire cannulation can be attempted. Hydrophilic guidewires with a special slippery coating are ideal for cannulation, because they minimize trauma to the papilla and more effectively seek out the path to the desired duct. The guidewire is extended several millimeters from the tip of the cannula or sphincterotome, and the papillary orifice is cautiously probed with the wire, until it slips into the duct (Fig. 27.2). When deep cannulation is achieved, the cannulating catheter can be advanced over the wire into the duct.
Precutting
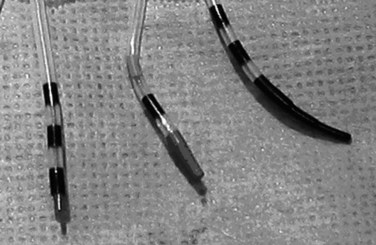
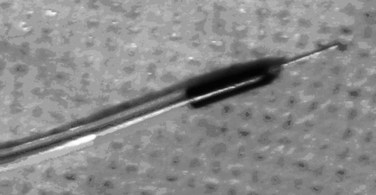
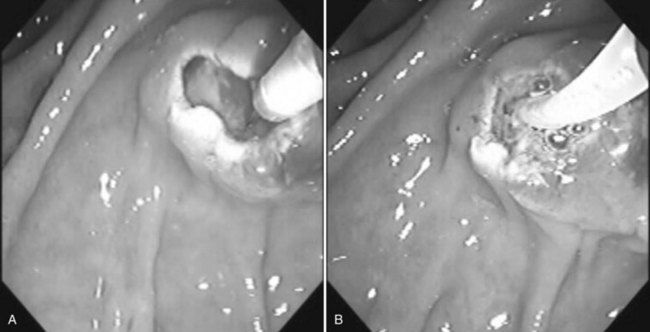
Precutting is performed with either a needle-knife catheter (Fig. 27.3, top) or Erlangen-type precut papillotome (Fig. 27.3, bottom). Most of the published experience has been with the needle-knife catheter, which consists of a retractable bare diathermy wire that extends 5 mm from the tip of the catheter; the needle is inserted at or just above the papillary orifice, and the cut is directed upward in the 11 to 12 o’clock position (Fig. 27.4). Biliary cannulation success rates exceeding 90% have been reported (Misra, 2009). The needle knife can also be used to create a supraampullary fistula in patients with biliary obstruction as a result of an ampullary malignancy. Another application is to free an impacted stone at the papilla; an incision is made directly into the most bulging portion of the papilla against the surface of the impacted stone. Higher complication rates with precut sphincterotomy for stone extraction have been reported (Pereira-Lima et al, 2001).
Precutting is not without risk, but some series suggest that in expert hands, it does not increase the risks of pancreatitis (Lawrence et al, 2009). Two large multicenter studies identified precutting as a significant risk factor for postsphincterotomy pancreatitis, and there have been isolated reports of perforation. Practice guidelines have established that precutting requires appropriate training and expertise and should be reserved for patients with a strong indication for sphincterotomy (Carr-Locke, 2004).
Rendezvous Procedure
Biliary cannulation can be aided by a combined percutaneous and endoscopic approach, known as a rendezvous procedure. A guidewire is inserted via the percutaneous transhepatic route into the duodenum and is subsequently grasped at the endoscopic end. The guidewire is pulled through the working channel of the endoscope and serves as a guide rail to enable retrograde biliary cannulation, sphincterotomy, and further endoscopic intervention (Calvo et al, 2001).
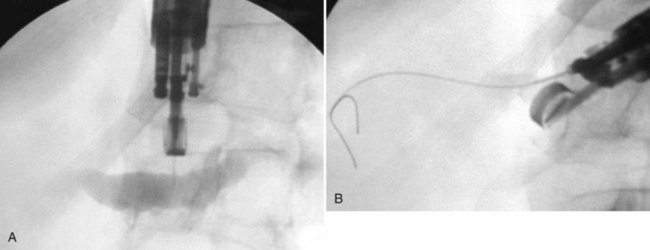
A rendezvous approach also can be used to accomplish biliary or pancreatic duct cannulation under endoscopic ultrasound guidance (Mallery et al, 2004). The bile or pancreatic duct is punctured transduodenally or transgastrically with a standard fine aspiration needle loaded with a guidewire. The wire is advanced anterogradely across the stricture into the duodenum (Fig. 27.5), and the stent is placed over the wire in the standard retrograde fashion.
A further variation of the rendezvous approach can be used to achieve cannulation of the pancreatic duct (Bataille & Deprez, 2002). The minor papilla is used to pass a wire from the duct of Santorini into the duct of Wirsung and then across the major papilla. When cannulation of the major papilla is achieved, the wire is rerouted from the minor papilla to the main pancreatic duct (Fig. 27.6).
Juxtapapillary Diverticula
Frequently found in elderly patients, juxtapapillary duodenal diverticula alter the position and anatomic boundaries of the papilla and displace the course of the bile and pancreatic ducts, making cannulation more difficult (Panteris et al, 2008). Accessing the papilla is a problem when it is located within the diverticulum, but various ancillary maneuvers may improve access. Aspirating air from the diverticulum may help “evert” the diverticulum, bringing the papilla into a more favorable position for cannulation. Altering the patient’s position and applying abdominal pressure may also be helpful. Failing these, a small depot of normal saline can be injected into the submucosal plane of the mucosa adjacent to the papilla. The injection should be made on the diverticular side of the papilla in an attempt to “tilt” it toward the endoscopist (Fig. 27.7). The use of two accessories, forceps and cannula, inserted together through the working channel to enable the endoscopist to pull the papilla out of the diverticulum and cannulate the papilla simultaneously also has been described (Fujita et al, 1998).
Deep cannulation of the bile duct adjacent to a large juxtapapillary diverticulum may be difficult, because the diverticulum distorts the course of the distal common bile duct. It is helpful to alter the direction of cannulation after entering the biliary orifice according to the anatomy of the diverticulum (Fig. 27.8). The direction of cannulation may be caudal rather than cranial; a guidewire tends to straighten the course of bile and pancreatic ducts and may facilitate deep cannulation (Draganov et al, 2005).
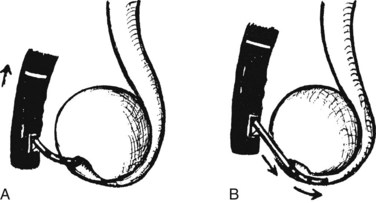
Billroth II Gastrectomy
A patient who has undergone a Billroth II gastrectomy poses a special challenge to the endoscopist. Accessing the papilla is the first obstacle. When the afferent loop is long, it can be difficult to intubate, and the papilla can be difficult to reach. Cannulation of the Billroth II papilla is the second obstacle. Because the endoscope approaches the papilla from below rather than above, the papillary anatomy in a Billroth II patient appears reversed. The bile duct is cannulated by orienting the catheter downward, toward the 5 to 6 o’clock position, rather than toward the standard 11 to 12 o’clock position. It is helpful to use a new, straight catheter or mold a downward bow into the catheter to achieve this (Fig. 27.9). A rotatable sphincterotome can also aid in the cannulation of the bile duct (Kim et al, 2008). Cannulation of the pancreatic duct is achieved by inserting the catheter at the 11 o’clock position and aiming it upward in a right-to-left orientation. The bile duct is usually easier to cannulate than the pancreatic duct, because the catheter is automatically directed in the axis of the bile duct. The placement of a guidewire into the bile duct aids in the placement and performance of the sphincterotomy (Dolay & Soylu, 2008).
Sphincterotomy
The basic technique of sphincterotomy has changed little since its initial description. The standard sphincterotome, the Erlangen “pull-type” model, consists of a catheter containing a cautery wire exposed 20 to 25 mm near the tip of the instrument. The leading tip distal to the wire, the “nose,” is 5 to 10 mm in diameter. After deep bile duct cannulation, the sphincterotome is retracted slowly, until one fourth to one half of the wire length is exposed outside the papilla. The sphincterotome is slightly bowed so that the wire is in contact with the roof, but not excessively, to avoid a “zipper” incision. The incision is made by gently lifting the sphincterotome against the papillary roof using the elevator and up–down controls while applying short bursts of current. The power settings vary according to the type of diathermy unit used. It is debated whether blended or pure-cut current should be used. Theoretically, pure-cut current would be associated with less edema of the ampulla and may decrease the risk of pancreatitis, but the risk of postsphincterotomy hemorrhage might be greater. In a prospective randomized study, the use of pure-cut current was associated with a lower incidence of pancreatitis than with blended-current sphincterotomy (Elta et al, 1998). In addition, the use of blended current after pure cutting reduced the risk of bleeding without increasing the risk of pancreatitis (Gorelick et al, 2001). Another randomized study found that pure-cut current did not reduce the frequency of pancreatitis and was associated with a significantly increased risk of minor bleeding (Macintosh et al, 2004). If blended current is used, the cut should be monitored for excessive tissue blanching and edema, because this is likely to increase the risk of pancreatitis.
The length of a bile duct sphincterotomy should be tailored to the indication. A small incision (≤1 cm) is adequate for stent insertion, whereas stone extraction usually requires a larger incision, depending on the size of the stone to be extracted (Fig. 27.10A). The extent of the sphincterotomy is limited by the length of the intraduodenal portion of the common bile duct. The length of a pancreatic duct sphincterotomy should not exceed 1 cm because of the perpendicular insertion at the ampulla (Fig. 27.10B). In rare cases, a biliary sphincterotomy can be performed with a sphincterotome placed through a percutaneously placed choledochoscope (Itoi et al, 2004). The adequacy of a sphincterotomy can be gauged by the ability to move the bowed sphincterotome across the opening. In the presence of a juxtapapillary diverticulum, the incision should be performed in millimeter increments, paying close attention to the boundaries of the incision and the course of the intraduodenal segment of the bile duct. Late stenosis has been reported to be more common after pancreatic sphincterotomy than after biliary sphincterotomy and is easily treated with repeat endoscopic sphincterotomy (Veldkamp et al, 2007).
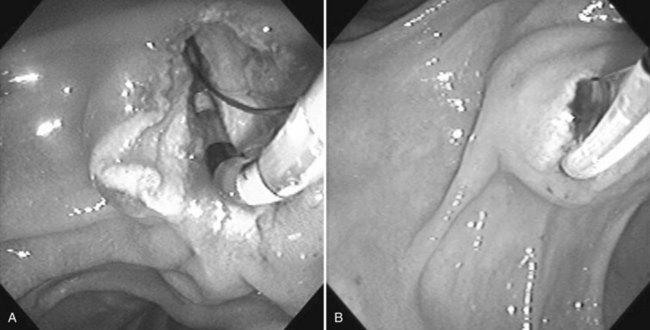
In a Billroth II patient, the standard pull-type sphincterotome is unsuited for sphincterotomy because of the difficult approach to the papilla. Special sphincterotomes and techniques have been developed to accommodate this anatomic variation (Dolay & Soylu, 2008). As an alternative to the sphincterotome, a needle knife can be used to perform the sphincterotomy over a previously inserted stent that serves as a guide rail for the incision (Nakahara et al, 2009; Fig. 27.11).
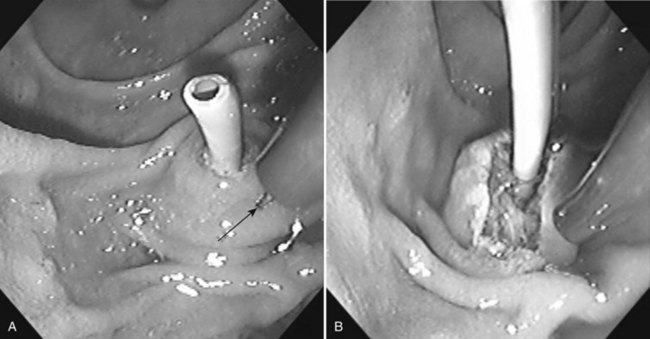
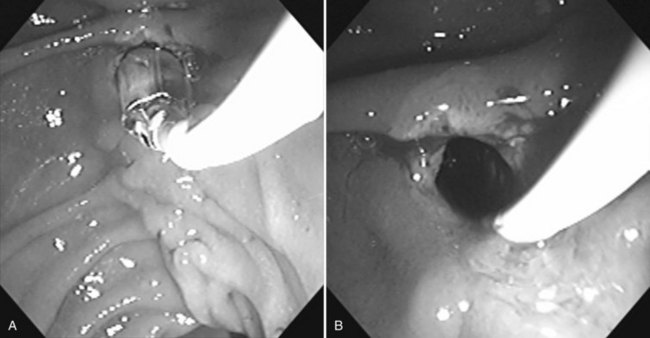
Sphincterotomy of the minor papilla in a patient with pancreas divisum requires greater caution because of the smaller size of the papilla. Wire-guided cannulation will aid in the performance of a minor ampulla sphincterotomy (Maple et al, 2009). The incision length is generally 3 to 5 mm, but it may be larger if the minor papilla is very prominent. The incision is made at the 12 o’clock position. A needle knife can also be used to perform the sphincterotomy over a 5- or 7-Fr stent (Fig. 27.12; Kwan et al, 2008), and balloon dilation sphincteroplasty can be used to aid in the extraction of pancreatic duct stones (Maydeo et al, 2009). A reduction in symptoms and episodes of pancreatitis is often reported after sphincterotomy in older patients with a history of recurrent pancreatitis and a dilated pancreatic duct (Fukumori et al, 2007; Borak et al, 2009).
Sphincteroplasty
Balloon dilation of the sphincter muscle using high-pressure hydrostatic balloons 6 or 8 mm in diameter has been employed as an alternative to sphincterotomy (Fig. 27.13; MacMathuna et al, 1994). The theoretical advantage of this approach is the preservation of the sphincter function. The drawback of balloon dilation is a more limited size of the papillary opening, which may limit the size of the stone that can be extracted using the balloon or a basket catheter. Stones measuring greater than 8 mm often require mechanical lithotripsy to enable transpapillary extraction. The risk of pancreatitis seems to be higher after a sphincteroplasty compared with a sphincterotomy, but balloon dilation after a limited sphinctertomy does not increase the risk of pancreatitis (Kowalski et al, 2009).
Stone Extraction
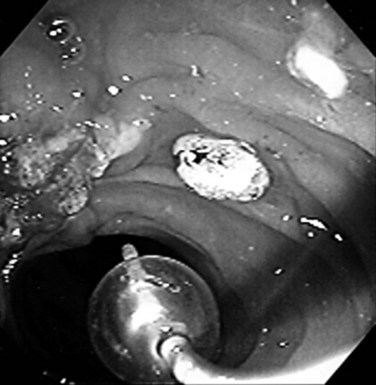
Several series have shown that 85% to 90% of bile duct stones can be removed effectively after endoscopic sphincterotomy with a basket and/or balloon catheter (see Chapters 36 and 37). The choice of basket or balloon is largely dictated by stone size: baskets are sturdier and provide better traction for removal of a larger stone (Fig. 27.14); a balloon catheter occludes the lumen and is ideal for removing small stones or sludge (Fig. 27.15).
Several technical points may increase the success rate of stone extraction. The sphincterotomy should be generous enough to enable extraction of the stone. The adequacy of the incision can be assessed by passing an inflated balloon catheter through the sphincterotomy opening. If multiple medium or large stones are present, it is important to remove stones individually, beginning with the lowermost stone, to avoid stone impaction. If a stone is mistakenly captured, it can be dislodged from the basket by pushing it upward into the hepatic duct confluence, where the basket tends to fold over or advance into the hepatic duct, thereby releasing the stone. When extracting a stone, the direction of traction should be in the axis of the bile duct, which can be verified on fluoroscopy. The success rate of stone extraction after balloon sphincteroplasty is very high (Garcia-Cano et al, 2009). Lithotripsy is indicated for the extraction of stones too large for extraction through the sphincteroplasty (Attasaranya et al, 2008).
Intrahepatic stones pose a special challenge, because they are difficult to access via the retrograde transpapillary route (see Chapters 39 and 44
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree