Inguinal Anatomy: Laparoscopic View
Maurice E. Arregui
Introduction
The intraperitoneal view of the pelvis and inguinal area is quite deceptive when looking at it through the lens of a laparoscope. It is a two-dimensional view that gives the impression that there is a peritoneal layer, a preperitoneal layer in which all structures of the inguinal area lie and the abdominal wall with a portal for exit of the cord structures.
In fact, the inguinal area is quite three-dimensional and is made up of various layers with intertwining fascial planes that serve as conduits for blood vessels, lymphatics, ureters, muscles, tendons, and nerves. To really understand the anatomy of the preperitoneal spaces of the inguinal area, one must know the embryology and migration of structures with their surrounding fascia. These fascial layers define the planes and create conduits for these structures. From the intraabdominal perspective, the laparoscopic view gives an opaque picture of the various layers of the inguinal structures with encompassed contents. A more clear view is obtained during laparoscopic inguinal hernia repair. This chapter will attempt to perform a laparoscopic dissection of the preperitoneal and inguinal spaces to identify the anatomy of the structures in their various encompassing fascial spaces.
Embryology of the Inguinal Area
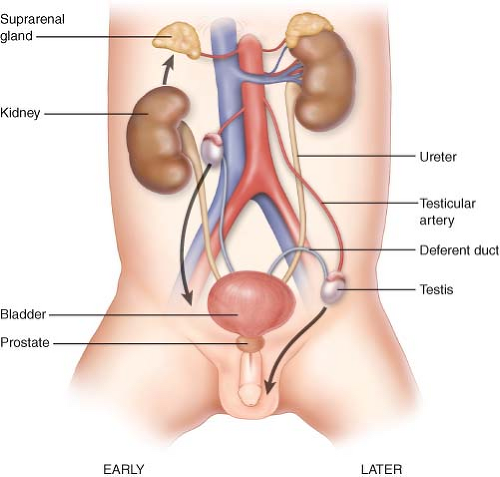
Key to understanding the fascial layers of the lower abdominal wall is understanding the embryology of the genitourinary tract with development of the bladder, ascent of the kidney, and descent of the testis. The bladder, ureters, kidneys, testicular vessels, testicles, and vas deference begin as intraperitoneal and extraperitoneal organs possibly covered by a continuous anterior and posterior fascia. During descent of the testicle between the seventhth and twelfth weeks, the gubernaculum contracts to pull the testicle and vas deference down toward the scrotum. Between the third to seventh months, the testes lie in the inguinal canal and it descends into the scrotum around the time of birth (Fig. 14.1). As this occurs, it drags the testicular structures with the peritoneum. The fascia that surrounds these structures likely includes the umbilical
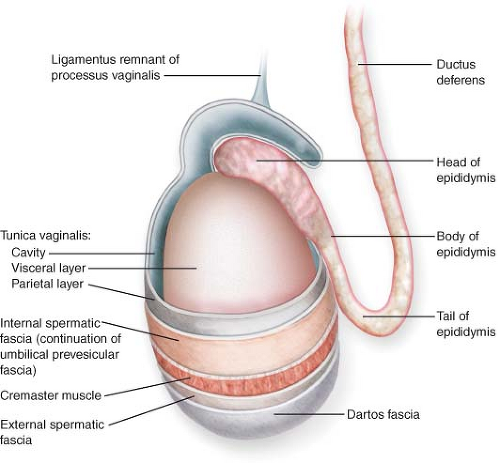
prevesicular fascia and or the transversalis fascia. After decent the tunica vaginalis obliterates proximally to form the peritoneal vaginal ligament that attaches to the tunica vaginalis testis. A serous bilaminar layer forming the parietal and visceral layers of the testis (Fig. 14.2). The internal spermatic fascia forms the layer surrounding the testis and tunica vaginalis. The internal spermatic fascia is described as being the
evagination of the transversalis fascia by some but may also have components of the umbilical prevesicular fascia (Fig. 14.3).
prevesicular fascia and or the transversalis fascia. After decent the tunica vaginalis obliterates proximally to form the peritoneal vaginal ligament that attaches to the tunica vaginalis testis. A serous bilaminar layer forming the parietal and visceral layers of the testis (Fig. 14.2). The internal spermatic fascia forms the layer surrounding the testis and tunica vaginalis. The internal spermatic fascia is described as being the
evagination of the transversalis fascia by some but may also have components of the umbilical prevesicular fascia (Fig. 14.3).
Intraperitoneal View of the Anatomy of the Inguinal Area
The structures include the bladder and umbilical ligaments in the midline and inguinal structures laterally. The bladder is at the base and at its apex is the median umbilical ligament which connects the bladder to the umbilicus. This is the median umbilical ligament which represents the obliterated urachus. On either side of the bladder are the medial umbilical ligaments which are remnants of the umbilical arteries that returned de-oxygenated blood from the fetus. This structure is connected to the internal iliac artery (Fig. 14.4A). The lateral umbilical fold is made up of the inferior epigastric vessels. This is probably a misnomer since these vessels do not have anything to do with the umbilical structures and provide blood supply to the anterior abdominal wall. The inferior epigastric vessels are enveloped by the trasversalis fascia shortly after exit from the external iliacs. Lateral to this is the internal inguinal ring. Entering this is the vas deferens and spermatic vessels in males (Fig. 14.4B, C) and round ligament in females (Fig. 14.4D). This is also the entry of an indirect hernia sac or remnant of the processus vaginalis. This is a fairly complex area that serves as portal for structures exiting the abdomen in transit to the scrotum.
Layers of the Abdominal Wall
Transperitoneal view of the lower anterior abdominal wall shows converging of the median and medial umbilical folds as it enters the umbilical ring. Lateral to the medial
umbilical fold the peritoneum is void of fat and therefore quite transparent. The posterior rectus sheath is well seen above the arcuate line and it thins out but does not disappear below (Fig. 14.5). Fibers of the layers of the posterior rectus sheath can be seen all the way to the pubis in many patients. A transverse view of the abdominal wall will show the rectus muscle, followed by the inferior epigastric vessels and deep to this is the posterior rectus sheath. Although the posterior rectus sheath is attenuated, all three fascial layers of the abdominal wall can be present to a variable degree. This includes the fascial layers of the external oblique, internal oblique, and transversus abdominus muscle which forms the transversalis fascia.
umbilical fold the peritoneum is void of fat and therefore quite transparent. The posterior rectus sheath is well seen above the arcuate line and it thins out but does not disappear below (Fig. 14.5). Fibers of the layers of the posterior rectus sheath can be seen all the way to the pubis in many patients. A transverse view of the abdominal wall will show the rectus muscle, followed by the inferior epigastric vessels and deep to this is the posterior rectus sheath. Although the posterior rectus sheath is attenuated, all three fascial layers of the abdominal wall can be present to a variable degree. This includes the fascial layers of the external oblique, internal oblique, and transversus abdominus muscle which forms the transversalis fascia.
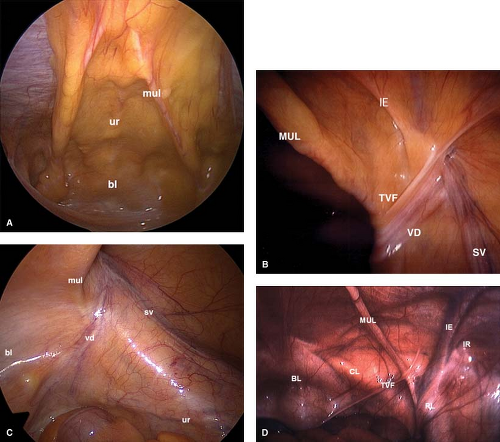 Figure 14.4 A: Laparoscopic views of the lower anterior abdominal wall. ur—obliterated urachus or median umbilical ligament, bl—bladder, and mul—medial umbilical ligament. B: View of the inguinal area in a male. MUL—medial umbilical ligament, IE—inferior epigastric arteries which form the lateral umbilical ligament, TVR—transverse vesicular fold, VD—vas deferens, and SV—spermatic vessels. With kind permission from E. Arregui. Surgical anatomy of the preperitoneal fasciae and posterior transversalis fasciae in the inguinal region. Hernia. Springer Science+Business Media; 1997;1:101–110. C:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|