Chapter 19 Ingested Foreign Objects and Food Bolus Impactions
![]() Video related to this chapter’s topics: Ingested Foreign Object
Video related to this chapter’s topics: Ingested Foreign Object
Introduction
Ingested gastrointestinal (GI) foreign bodies and food bolus impactions occur frequently and are the second most common endoscopic emergency after GI bleeding. The actual incidence of foreign bodies and food impaction is unknown, and few controlled data exist on the management of foreign body ingestions. Although most GI foreign bodies do not result in serious clinical sequelae or mortality,1 it has been estimated that 1500 to 2750 patients die annually in the United States because of the ingestion of foreign bodies.2–4 More recent studies have suggested the mortality from GI foreign bodies to be significantly lower, with no deaths reported in more than 850 adults and one death in approximately 2200 children with a GI foreign body.5–11 As a result of the frequency of this problem and the rare but possible negative consequences, it is important for the gastroenterologist and endoscopist to understand the patients at risk for ingestion of foreign bodies, the best method for a prompt diagnosis, and the correct management with avoidance of unwanted complications.
Epidemiology
True foreign bodies may be the result of either unintentional or intentional ingestion. The most common patient group that unintentionally ingests foreign bodies is children. Of foreign body ingestions, 80% occur in children, with most occurring between the ages of 6 months and 3 years.12,13 Pediatric ingestions are almost always accidental, resulting from the child’s natural oral curiosity.14 The most common items ingested by children are coins followed by small toys, crayons, buttons, pins, jewels, nails, and disc batteries.6,9,10,15,16
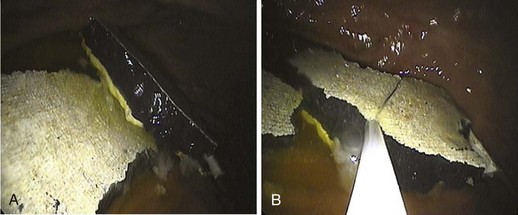
Accidental ingestion in adults occurs in various groups of patients. Dentures and the presence of dental appliances are a common risk factor for accidental foreign body ingestion secondary to impaired tactile sensation during swallowing.17,18 A common occurrence is a patient mistakenly ingesting his or her own dentures.19 The other large patient group in which accidental ingestion of foreign bodies occurs includes individuals with compromised judgment or senses, such as very elderly, demented, or intoxicated individuals. Accidental coin ingestion has been encountered in young college students secondary to an increasingly popular beer drinking game, “Quarters,” where a quarter may inadvertently be swallowed and become lodged in the esophagus.20 Roofers, tailors, carpenters, and seamstresses have increased rates of foreign body ingestion because of accidental swallowing of nails or needles placed in the mouth during work. Intentional ingestion of foreign bodies is frequent in psychiatric patients or prisoners (Fig. 19.1).21,22 These patients ingest foreign bodies for a secondary gain and often have a history of previous foreign body ingestion, ingest multiple objects, and often ingest very complex objects.
Iatrogenic foreign bodies related to GI endoscopy procedures are becoming an increasing problem. Symptoms and complications have been reported as a result of capsule endoscopy; migrated esophageal, luminal, or biliary stents; and migrated gastrostomy buttons and catheters.23,24
Esophageal food impaction is a much more common problem than true foreign body ingestion with an estimated annual incidence of 13 to 16 episodes per 100,000 people.25 Most (75% to 100%) patients who present with a food impaction have some type of predisposing esophageal pathology.5,25–28 The most commonly observed abnormalities associated with food impaction are Schatzki rings or peptic strictures and, increasingly, eosinophilic esophagitis.29 Less commonly found as a predisposing cause are webs, extrinsic compression, surgical anastomoses, fundoplication wraps, and bariatric gastroplasties.30 Esophageal cancer very rarely manifests with acute food bolus impaction.31 Motility disorders such as achalasia, diffuse esophageal spasm, and nutcracker esophagus are infrequent causes of food impactions.32
Food impaction most commonly occurs in adults in their 4th or 5th decade but is becoming more prevalent in young adults because of the increasing incidence of eosinophilic esophagitis. The type of food impacted correlates with cultural and regional dietary habits. In the United States, hot dogs, pork, beef, and chicken are the most common foods resulting in impaction, whereas fish and fish bones are the most common food to result in impaction in Asian countries and coastal areas.33–35
Pathophysiology and Pathogenesis
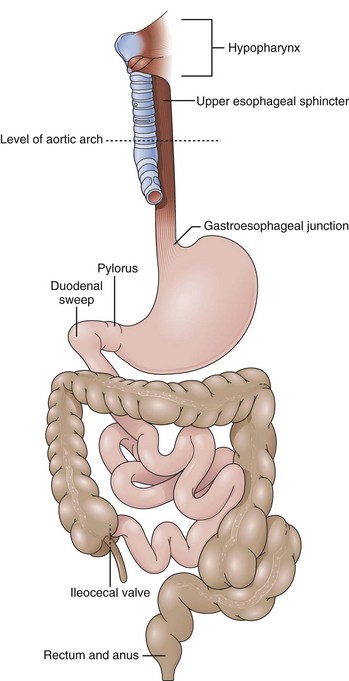
Most (80% to 90%) ingested foreign bodies and food bolus impactions pass spontaneously without clinical sequelae.1 However, 10% to 20% of GI foreign bodies require endoscopic intervention, and 1% may require surgical intervention.5,31,36 It is important to understand how ingested foreign bodies can result in significant disease, which patients are more likely to ingest complex foreign bodies, and in which parts of the GI tract foreign bodies are most likely to cause damage (Fig. 19.2). This understanding ensures appropriate use of endoscopic and surgical interventions.
The most common complications related to foreign bodies are obstruction and perforation, which can occur in any area of the GI tract where there is narrowing, angulation, anatomic sphincters, or previous surgery.37 The posterior hypopharynx is the first area of the GI tract in which a foreign body may become lodged, particularly small sharp objects such as chicken or fish bones.38,39 In the esophagus, there are four areas of physical narrowing where a food bolus or foreign body is likely to impact: the upper esophageal sphincter, the level of the aortic arch, the crossing of the main stem bronchus, and the lower esophageal sphincter (LES) and gastroesophageal junction. All of these areas have been shown to be areas of true luminal narrowing with diameters of 23 mm or less in adult patients.40
Independent of the physiologic areas of narrowing, most food boluses are associated with esophageal pathology, including rings, webs, diverticula, and peptic strictures.2 Multiple esophageal rings associated with eosinophilic esophagitis have led to esophageal food impaction at much greater incandescence in young adults.41,42 Uncommonly, esophageal motor disturbances, such as achalasia, diffuse esophageal spasm, or segmental variations in peristalsis, may contribute to food and foreign body impactions.43–46
Foreign bodies and food impactions in the esophagus generally have the highest incidence of complications with the rate of complication being directly proportional to the time the object spends in the esophagus. Esophageal foreign bodies may lead to perforation, abscess, mediastinitis, pneumothorax, fistula formation, and cardiac tamponade.47,48 Once through the esophagus, most objects, including sharp objects, pass through the intestinal tract without consequence.1,37 However, among patients presenting with symptoms related to a foreign body, the perforation rate has been estimated to be 5% overall and up to 35% for sharp and pointed objects.31,49 Esophageal perforation is the most frequent cause of significant morbidity and mortality.47 The risk of perforation of the esophagus increases dramatically when foreign bodies or food boluses are left impacted in the esophagus for more than 24 hours. Other reported complications, including complications that have been reported to lead to fatalities, include GI bleeding, aortoenteric fistulas, aspiration, abscess formation, and true rarities such as perforation of the heart and lead and zinc toxicity.50–56
Once in the stomach, most foreign bodies pass through the GI tract without complications in 1 to 2 weeks. Exceptions are objects with a diameter of greater than 2 cm and objects longer than 5 cm, such as pencils, pens, and eating utensils, which have difficulty passing through the pylorus or the duodenal bulb and sweep.37,38,57 In the small intestine, three points of impedance exist where a foreign body may become lodged and result in obstruction: In the duodenal C-loop, long objects may get “hung up” and result in perforation. The narrowing and angulation of the ligament of Treitz can result in foreign body obstruction, and even smaller objects that were able to pass through the pylorus and ligament of Treitz may cause a distal small bowel obstruction by becoming impacted at the ileocecal valve. Patients with small bowel disease, history of adhesions, or partial small bowel obstructions may have greater difficulty passing foreign bodies through the small intestine.
Most objects, once in the small intestine and colon, do not cause damage. The bowel tends to protect itself naturally against foreign bodies. A foreign body stimulates peristalsis and axial flow in the small intestine, which results in the foreign body concentrated in the center of fecal residue with the blunt end leading and the sharp end trailing.58,59 As the foreign body travels further into the large intestine, it usually becomes centered in the lumen surrounded by stool, making a complication even less likely.2 Rectal foreign bodies rarely result from ingestion and more frequently are inserted into the rectum through the anus. However, occasionally an ingested foreign body may traverse the entire GI tract to the rectum before further passage is impaired by the rectal valves of Houston or the internal and external sphincters.
Clinical Features: History and Physical Examination
For adults who are able to communicate, a history of ingestion including timing, type of foreign body ingested, and onset of symptoms is usually reliable. History is particularly reliable for food impactions because patients are almost always symptomatic and can detail the exact onset of symptoms. Small sharp objects or fish bones often manifest with a foreign body sensation or odynophagia in the posterior pharynx or cervical esophagus; this occurs even if the foreign body has passed to the stomach because of a small mucosal laceration. Partial or complete esophageal obstruction almost always results in symptoms. Esophageal obstruction may cause substernal chest pain, dysphagia, gagging, vomiting, or a sensation of choking.60 More complete obstruction can lead to drooling and the inability to handle oral secretions.
The type of symptoms may aid in determining whether an esophageal foreign body is still present and where in the esophagus it may be located. If the patient presents with dysphagia, dysphonia, or odynophagia, there is almost an 80% chance that a foreign body or food impaction is present. If the symptom is retrosternal pain or a pharyngeal discomfort only, less than 50% of patients have an identifiable foreign object.61 The patient may be able to localize the object successfully in the posterior pharynx or at the level of the cricopharyngeal muscle. However, for objects located more distally in the esophagus and in the stomach, patient localization becomes poor with an accuracy of 30% to 40% in the esophagus and almost 0% in the stomach.62,63 Once in the stomach, small intestine, or colon, the only symptoms described would be secondary to a complication resulting from the foreign body, such as obstruction, perforation, or bleeding.
The history and symptoms for true foreign bodies are often less reliable than food impaction because true foreign bodies are often ingested by children, mentally impaired adults, or adults who have ingested the foreign body for secondary gain. Even with esophageal foreign bodies, 20% to 38% of children are asymptomatic.62,64 In children and adults unable to communicate, there may be no history of a foreign body ingestion from the patient or the caregiver in up to 40% of cases,65 necessitating a high degree of suspicion. Symptoms are more subtle and include drooling, poor feeding, blood-stained saliva, or a failure to thrive.65,66 Respiratory compromise may occur with aspiration or a proximally located esophageal foreign body that compresses the trachea causing wheezing and stridor.65,67
Diagnosis
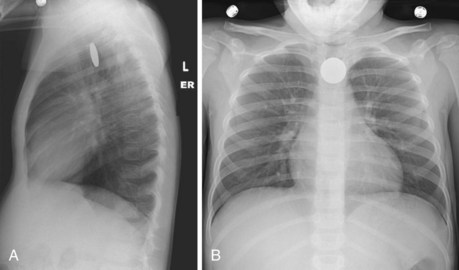
Diagnostic evaluation should begin with plain film radiographs. Patients with suspected foreign body ingestion should undergo anteroposterior and lateral radiographs of the chest and abdomen to help determine the presence, type, and location of a foreign body.49 Anteroposterior and lateral neck and chest films are suggested if there is a suspicion of a foreign body in the esophagus versus the trachea or if there is a foreign object that may be obscured by overlying spine (Fig. 19.3).65,68 Plain films also aid in detecting complications such as aspiration, abdominal free air, or subcutaneous emphysema.60,69 Radiographic studies are more controversial in children. Because history from children is often poor, mouth-to-anus screening films have been advocated in suspected foreign body ingestions.49
Other authors have suggested a more directed approach or nonradiographic methods to determine the presence and location of foreign bodies in children.70 To limit radiation, hand-held metal detectors have been used with a sensitivity of greater than 95% for the detection and localization of metallic foreign bodies.71 Plain films are satisfactory in some cases of true foreign bodies and occasionally in cases of food ingestions with larger bones. Smaller bones or thin metal objects are not readily seen, however, and many objects, including plastic, wood, and glass, are not radiopaque.6 False-negative rates with plain films can be 47% and false-positive rates are close to 20% in the investigation of foreign bodies.61,72 Of films read by a nonradiologist for the presence of foreign bodies, 35% have been found to be misread.73 Generally, it is accepted that barium studies should not be performed in the evaluation of GI foreign bodies. If aspiration occurs, the hypertonic contrast agents used can cause acute pulmonary edema.74 Barium evaluation can delay a necessary therapeutic endoscopic procedure by interfering with endoscopic visualization and complicating removal of a foreign body.75
Advanced imaging such as computed tomography (CT) or magnetic resonance (MR) imaging may be used in unusual or difficult-to-diagnose cases and may aid in detecting soft tissue inflammation or the presence of an abscess. Three-dimensional CT has been used to diagnose foreign bodies not seen with other imaging and may aid in detecting complications of foreign body ingestion such as perforation or abscess before the use of endoscopy, and MR imaging may have a role in showing soft tissue periesophageal pathology.65,76,77
Diagnostic endoscopy provides the most accurate diagnostic modality in suspected ingested foreign bodies and food impactions. Any patient with persistent symptoms and a continued clinical suspicion of a GI foreign body should undergo upper endoscopy even after negative or unrevealing radiographic evaluation.78 This approach ensures the correct diagnosis of food impactions, nonradiopaque objects, and radiopaque objects that are obscured by overlying bony structures.37 Endoscopy is the best method to detect underlying pathologic conditions, such as esophageal strictures, that contribute to a food impaction or foreign body that does not pass readily through the GI tract. Endoscopy also can closely examine the GI mucosa to assess for laceration or damage that may contribute to continuing symptoms after a foreign body has spontaneously passed. Most importantly, diagnostic endoscopy is directly linked to when endoscopy is used for therapy—treatment or extraction of a known or suspected foreign body. Diagnostic endoscopy is not indicated when small, blunt objects are known to have passed into the stomach and the patient is asymptomatic. These objects traverse the pylorus and the rest of the GI tract without complications. If a foreign body is known to have passed the ligament of Treitz, diagnostic and therapeutic endoscopy would be of little added benefit. Rare exceptions are sharp objects that can be safely extracted with an enteroscope. More recently, double-balloon enteroscopes have been used for the retrieval of ingested foreign bodies and retained endoscopy capsules in the small bowel.79,80 Finally, diagnostic endoscopy is contraindicated when there is physical examination or radiographic evidence of a bowel perforation anywhere in the GI tract or a small bowel obstruction beyond the ligament of Treitz secondary to the foreign body.
Treatment
Of GI foreign bodies, 75% to 90% pass through the GI tract spontaneously without complication.5,81 Two more recent studies have emphasized conservative management with 86% to 97% of foreign bodies passing spontaneously with minimal complications.82,83 Esophageal foreign bodies were excluded from the above-mentioned studies. Although conservative management is successful in most nonesophageal foreign bodies, a more appropriate treatment plan if immediate endoscopy is not performed is to have a policy of expectant management and then selective endoscopy based on type, size, and location of the ingested object.84,85
Numerous medical therapies for esophageal foreign bodies or food impactions have been studied as primary treatment or in conjunction with endoscopic therapy. The most frequently used medication is glucagon, a smooth muscle relaxant that significantly reduces LES pressure with doses of 0.25 mg.86 Glucagon has treated esophageal food impactions successfully in 12% to 58% of cases.87–89 However, a randomized trial found glucagon no better than placebo in treating children with coins lodged in the esophagus.90 Glucagon is generally safe but may result in nausea, abdominal distention, and, rarely, vomiting. Glucagon would not work with a fixed obstruction present, which is often found with esophageal foreign bodies and food impactions. Glucagon does not provide definitive examination and treatment of coexisting esophageal pathology as does flexible endoscopy. Finally, glucagon may help when used with endoscopy by lowering LES pressure and facilitating the endoscope pushing a food impaction into the stomach.91 Nitroglycerin and nifedipine are other smooth muscle relaxants that have been anecdotally described as promoting passage of esophageal impactions into the stomach.49
Medical methods that have been described but should be avoided are gas-forming agents, emetics, and papain meat tenderizer. Gas-forming agents combined with a smooth muscle relaxant have been reported to have success rates of almost 70% in clearing esophageal foreign bodies into the stomach.92 However, esophageal rupture and perforation have occurred with these agents, particularly if there is a fixed obstruction or the foreign body has been present more than 6 hours.93,94 Papain, a meat tenderizer, and emetics for the treatment of food impaction are two methods that should never be used because of the risk of esophageal necrosis, perforation, and aspiration.2,95,96
The radiologic literature has multiple descriptions of methods to remove esophageal foreign bodies under fluoroscopic guidance. Reported methods include extraction with Foley balloon catheters, suction catheters, wire baskets, or a magnetic catheter to extract ferromagnetic metal objects.69,97 The largest experience has been with Foley catheters where the catheter is passed either nasally or orally into the esophagus and past the foreign body. The balloon is inflated and withdrawn to deliver the foreign body to the oropharynx where it can be retrieved. Although high success rates have been reported, the major drawback is loss of control of the foreign body, particularly at the level of the upper esophageal sphincter and laryngopharynx. Complications reported include nosebleeds, dislodgment of the foreign body in the nose, laryngospasm, vomiting, and, of largest concern, aspiration with resultant airway obstruction and death.98,99 Because radiologic methods do not match the efficacy or safety of endoscopy, few indications exist for their use. Radiologic methods to remove foreign bodies or food impactions should be limited to when endoscopy is unavailable or cannot be available within 12 to 24 hours.
Flexible endoscopy has become the diagnostic and therapeutic method of choice in both true GI foreign bodies and food boluses in pediatric and adult patients. This recommendation is based on multiple large series using endoscopy for the treatment of GI foreign bodies with success rates greater than 95% and associated morbidity and mortality reported at 0% in most studies but always less than 5%.5,9,25–27,75,100–103 Although treatment failures are rare, predictors of endoscopic failure and complications include intentional ingestion, ingestion of multiple complex foreign bodies, and lack of patient cooperation.49
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree