Chapter 18 Hirsutism
INTRODUCTION
Hirsutism is a cosmetic concern from the patient’s perspective. Various studies have shown an increased prevalence of social fear and depression among hirsute women.1,2 Whether or not these psychological symptoms have a neuroendocrine basis remains to be elucidated.3 The old adage that “Even a single hair casts its own shadow” may help the clinician deal with the problem objectively. Indeed, even minor degrees of hirsutism may have major consequences on self-image in certain individuals.
Hirsutism needs to be differentiated from hypertrichosis. Hypertrichosis, referring to a diffuse increase in fine (vellus) hair that is not androgen dependent, may be congenital or associated with other medical conditions such as hypothyroidism or porphyria or may be associated with certain medications4,5 (Table 18-1).
Table 18-1 Disorders and Drugs Causing Hypertrichosis
| Disorders | Drugs |
|---|---|
| Thyroid disorders | Diphenylhydantoin |
| Anorexia nervosa | Diazoxide |
| Dermatologic disorders | Minoxidil |
| Cyclosporine | |
| Streptomycin | |
| Prolonged administration of cortisone | |
| Penicillamine | |
| Psoralens |
PREVALENCE
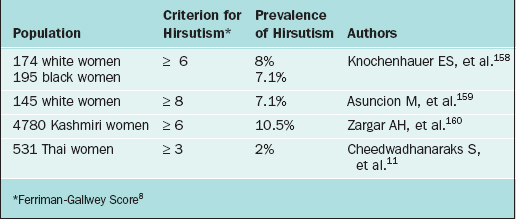
It has been estimated that between 5% and 15% of women surveyed are affected with hirsutism, although the exact prevalence remains uncertain.6,7 These estimates depend on the criteria used and the population studied. There is a wide degree of variation of what is considered normal hair growth. It is influenced heavily by the woman’s race and cultural background. It is generally accepted that women of Mediterranean origin have more body hair per unit area than Asians of the mongolian race.
Traditionally, hirsutism has been quantified according to criteria established by Ferriman and Gallwey.8 In this system, nine body areas sensitive to androgen are graded from 0 (absent), through 1 (minimal terminal hair) to 4 (frank virilization). In this scoring system, the minimum score is 0 and the maximum is 36. In their study of 161 women, Ferriman and Gallwey noted that 9.9% had a score of greater than 5, 4.3% had a score above 7, and 1.2% obtained a score above 10. In general, a score of 8 or more has been considered to represent hirsutism. Various investigators have modified this scoring system over the years.9,10
Hirsutism scores vary widely among women of different ethnic origins (Table 18-2). Consequently, a numeric cutoff point for hirsutism needs to be defined in the context of the population of interest. In clinical practice, the use of a standardized scoring system is impractical. It is limited by subjective variability as well as varying cutoff points depending on ethnicity.5,11 From a practical point of view, hirsutism may be classified simply as mild, moderate, or severe. Specifying the affected areas is helpful in following the response to therapy.
THE HAIR FOLLICLE AND HAIR GROWTH CYCLE
The hair follicle is composed of dermal and epidermal components.12 Together with the arrector pili muscles and sebaceous glands, it forms the pilosebaceous unit. In androgen-sensitive areas, each pilosebaceous unit has the capacity to differentiate into a terminal hair or into a sebaceous follicle.
There are three main types of human hair follicles. These have been classified according to the size and depth of the follicle13:
The hair follicle undergoes repetitive cycles of growth postnatally.14 In fact, the hair growth cycle has been described as a recapitulation of embryogenesis.15 The hair cycle includes three phases: telogen (resting), anagen (growth), and catagen (shortening). In humans, hair growth occurs in a mosaic pattern, where the activity of each follicle is independent of its neighbors.15 In human scalp hair, 85% to 90% of the hair follicles are in anagen, 13% are in telogen, and less than 1% are in catagen at any given time.16
Factors mediating the close relationship between the epidermal and dermal components of the hair follicle are the subject of increasing studies. Different growth factors have been implicated in the control of hair development—epidermal growth factor, fibroblast growth factor, tumor necrosis factor-β, and insulin-like growth factors.17–20 Hair growth is therefore the culmination of interactions between an organism’s genetic make-up influenced by environmental signals from the endocrine and paracrine environment. Although the morphologic changes in the hair growth cycle are well documented, the molecular mechanisms underlying the regulation of the phases of hair growth are still not well understood.
ANDROGENS AND HAIR GROWTH
Hirsutism is caused by high circulating androgen levels and/or by an increased sensitivity of the hair follicle to androgen exposure. Androgen excess has been described as the most frequent endocrine disorder in women of reproductive age.21 It is believed to occur in 75% to 85% of women with hirsutism.7 Hirsutism is only one of the clinical signs of androgen excess, which also includes androgenic alopecia, acne, and infertility.22
Androgen Production and Metabolism
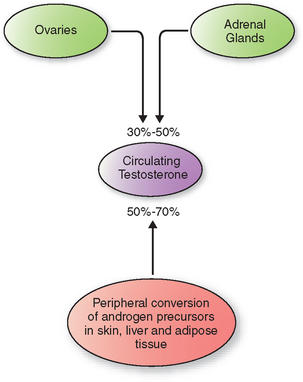
In women, direct secretion from the ovaries and the adrenal glands accounts for 30% to 50% of circulating testosterone (Fig. 18-1). The rest arises from peripheral conversion of androgen precursors to testosterone, mainly in the skin, liver, and adipose tissue.23 Androgen precursors include androstenedione, dehydroepiandrosterone (DHEA), and dehydroepiandrosterone sulfate (DHEAS).
Testosterone is the most important circulating androgen. It is present either protein-bound or free in the circulation. Approximately 98% to 99% of plasma testosterone is protein bound—with higher affinity to sex hormone-binding globulin (SHBG) and more loosely to the larger pool of albumin and other proteins. Various factors affect the hepatic production of SHBG. Androgens, insulin, and growth hormone lower SHBG levels, whereas estrogens and thyroid hormone excess result in increased SHBG levels.24
Because of the greater affinity of SHBG to testosterone compared to estradiol, changes in SHBG concentration produce a much greater alteration in the percentage of unbound testosterone than of unbound estradiol. This relationship has been characterized as a see-saw, with SHBG as the fulcrum whose position moves in response to estrogens and androgens (Table 18-3).25 In this way the balance between the levels of free estrogen and free testosterone is determined by the amount of SHBG, whose concentration is determined by these hormones. Accordingly, SHBG acts to amplify the tissue exposure and response to androgen/estrogen balance.
Table 18-3 Role of SHBG in the Regulation of Free Estrogen and Testosterone
| High estrogen state: free estrogen increases and free testosterone decreases |
| Normal estrogenic state: balance |
| High androgen state: free estrogen decreases and free testosterone increases |
The free fraction of plasma testosterone is the biologically active portion. It is believed to enter the target cell by passive diffusion and then binds to the nuclear androgen receptor. Androgen binding leads to an allosteric conformational change, which in turn leads to receptor dimerization, nuclear transport, and target DNA interaction.26–28 These events culminate in target gene transcription.
Both testosterone and dihydrotestosterone bind to the same receptor but with different affinities, that for dihydrotestosterone being much greater than that for testosterone.29 The affinity for DHEA and androstenedione is markedly less.30
Site of Androgen Action in the Skin
The skin is a major site for the peripheral conversion of weak androgen precursors to active androgens.30 DHEA and DHEAS have little androgenic activity. However, these may be converted to androstenedione and subsequently to testosterone in the adrenal glands and in the peripheral tissues.
The active androgen in the skin is dihydrotestosterone.23 Conversion from the testosterone precursor is catalyzed by the enzyme 5α-reductase. Two forms of 5α-reductase are known. Type 1 is found mainly in nongenital skin; the gene responsible is found on chromosome 5. Type 2, encoded on chromosome 2, is primarily found in androgen target tissue such as the prostate, epididymis, seminal vesicle, and genital skin.31 The two types share 50% homology.
Dermal papilla cells taken from androgen-dependent areas such as the beard have been demonstrated to express a greater number of androgen receptors as compared to nonbalding scalp cells.15 Higher levels of 5α-reductase activity have also been demonstrated in beard cells.32 The varying sites of expression of the androgen receptor in the different cell types in the skin likely account for the diverse effects of androgens in the skin. These likely account for the disparity in hair distribution and thickness observed among hirsute individuals with similar androgen levels. The increased sensitivity of the pilosebaceous unit to normal levels of androgen is believed to be due to enhanced peripheral 5α-reductase activity, polymorphisms of the androgen receptor, or altered androgen metabolism.
ETIOLOGY OF HIRSUTISM
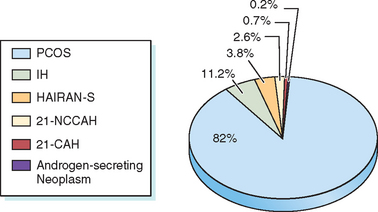
Hirsutism is a sign of increased androgen level or increased sensitivity of the hair follicles to androgen. Hyperandrogenemia is seen in 85% of patients with moderately severe hirsutism.6 Hirsutism may be idiopathic or due to androgen excess from either the ovary or the adrenal gland. Conditions associated with androgen excess from the ovaries include polycystic ovary syndrome (PCOS), hyperthecosis, and androgen-secreting ovarian tumors. Adrenal causes of androgen excess include Cushing’s syndrome, congenital adrenal hyperplasia (CAH), and androgen-secreting tumors. Most hirsute women will have PCOS33,34 (Fig. 18-2).
Idiopathic Hirsutism
The most widely accepted definition of idiopathic hirsutism includes normal androgen levels and normal ovulatory function in a hirsute patient.35 Using these criteria, the prevalence of idiopathic hirsutism has been estimated to be between 5% and 15%.36,37 Among 64 hirsute women claiming regular menses at intervals shorter than 35 days, 25 (39%) had an anovulatory cycle documented by a day 22 to 24 serum progesterone level of less than 4 ng/mL.36
Polycystic Ovary Syndrome
Although initially described in 1935 by Stein and Leventhal, a uniform definition for PCOS still does not exist.38 At the recent joint meeting of the European Society for Human Reproduction and the American Society of Reproductive Medicine, it was suggested that the diagnosis of PCOS is met when at least two of the three following elements are present: hyperandrogenism, chronic anovulation, and polycystic ovaries.39 The different diagnostic criteria for PCOS reflect the heterogeneous nature of this disorder. PCOS is still a diagnosis of exclusion. The prevalence of PCOS is estimated to be at 5% to 7% of reproductive age women.40 It is the most common cause of anovulatory infertility.
Polycystic ovary syndrome needs to be distinguished from polycystic ovaries alone. Although most women with PCOS have polycystic ovaries, a substantial population of normal women does as well. Polycystic ovarian morphology may be found in 20% or more of women of reproductive age.41,42 The significance of polycystic ovaries alone is unclear given that it seems to have no impact on fertility.43
Women with PCOS present with some or all of the following clinical features: oligomenorrhea, infertility, hirsutism, acne, alopecia, or obesity. It is important to remember that the syndrome has multiple components—reproductive, metabolic, and cardiovascular—that have health implications throughout the woman’s life.44
Insulin resistance, which refers to the diminished ability of insulin to exert its metabolic effects, is now thought to play a central role in PCOS.45,46 Beta-cell dysfunction, independent of insulin resistance, is also thought to contribute to the pathogenesis of the complications of PCOS.47 Women with PCOS have higher basal insulin concentrations and an increased prevalence of central obesity, type 2 diabetes mellitus, and hypertension.48 An estimated 50% to 70% of women with PCOS have insulin resistance.49 Not surprisingly, insulin resistance in women with PCOS is associated with obesity but may also be present in lean women with PCOS.50–52
The consequent hyperinsulinemia is believed to lead to androgen excess through several mechanisms: (1) stimulation of ovarian androgen production, (2) stimulation of adrenal androgen biosynthesis, (3) stimulation of luteinizing hormone (LH) release, and (4) decreasing hepatic SHBG production.53–56 Differentiating those women with PCOS with insulin resistance from those without insulin resistance therefore becomes important given the metabolic consequences and required surveillance for these women.57–59 Considering the paucity of data on the use of simple laboratory markers of insulin resistance in predicting risks and therapeutic response in women with PCOS, it is recommended that the best clinical approach may be the heightened surveillance in all patients for the clinical sequelae of insulin resistance, such as glucose intolerance, dyslipidemia, and hypertension.60
Congenital Adrenal Hyperplasia
CAH is a family of autosomal recessive disorders resulting from deficiency in one of the five enzymes necessary for the biosynthesis of cortisol and aldosterone.61 Clinical features depend on the degree of the enzyme defect. The classic forms of neonatal virilization result from a severe enzyme deficiency. Nonclassic forms, due to a less severe enzyme deficiency, may result in delayed signs of androgen excess. In this chapter, the three enzyme deficiencies that result in features of postnatal androgen excess are discussed (see Chapter 2 for details on steroidogenesis).
21-Hydroxylase Deficiency
This enzyme deficiency accounts for the majority (90% to 95%) of CAH cases.61,62 There is a wide variability in phenotypic expression, depending on the extent of the enzyme impairment. All the various forms of 21-hydroxylase deficiency are caused by either homozygous or compound heterozygous mutations in the CYP21A2 gene. The incidence is estimated to be 1:15,000 live births for the severe classic form of CAH.63 The prevalence is higher in certain ethnic groups, such as the Ashkenazi Jews.
Nonclassic 21-hydroxylase deficiency (21-OHD) has been reported to occur in from 1% to 10% of hyperandrogenic women.64 Affected individuals produce normal amounts of cortisol and aldosterone at the expense of elevated sex hormone precursors. Onset of symptoms is variable. Some may present with premature pubarche; others may be diagnosed after puberty when they present with symptoms resulting from androgen excess—menstrual irregularity, hirsutism, acne, or infertility. They are clinically indistinguishable from women with PCOS. Up to 50% of affected women (with nonclassic 21-OHD) have been reported to have polycystic ovaries on ultrasound examination.65 Serum androgen levels are comparable with those seen in PCOS as well.66 Measurement of 17-hydroxyprogesterone (basal or stimulated) currently is the main test used to diagnose nonclassic 21-OHD.
11β-Hydroxylase Deficiency
This is the second most common cause of CAH, seen in about 5% to 8% of cases.63 Clinical features are similar to the virilizing form of CAH. However, hypertension is a clinical feature believed to be due to the excess production of the mineralocorticoid deoxycorticosterone. Hypokalemia may be seen as well. Mild, late-onset presentations have been reported. Diagnosis is based on the response to a corticotropin stimulation test similar to 21-OHD; however, in this condition, deoxycorticosterone and 11-deoxycortisol are elevated.
Androgen-secreting Tumors
Adrenal Tumors
A purely androgen-secreting adrenal tumor is rare. More frequently, a mixed picture of Cushing’s syndrome with virilization is seen in adults.67 In a review of cases of androgen excess seen in the Mayo Clinic from 1946 to 2002, 11 female patients were identified to have pure androgen-secreting adrenal tumors. Five of these were malignant.68 Malignant tumors were bigger (9.8 cm vs. 4.2 cm) and heavier (232 g vs. 44 g). Surprisingly, mortality was reported in only one patient, a finding in marked contrast to the lower survival rates observed in other forms of adrenocortical carcinoma.69
Ovarian Tumors
Androgen-secreting ovarian tumors are also rare.70 Sertoli-Leydig cell tumors are the most common virilizing ovarian tumor and account for 0.5% of all ovarian neoplasms; however, even nonfunctional ovarian tumors may cause hyperandrogenism, probably mediated by stimulation of stromal cells adjacent to the tumor.71,72
Ovarian Hyperthecosis
Hyperthecosis refers to the nests of luteinized theca in the ovarian stroma. There is a considerable clinical overlap between patients with PCOS and those with ovarian hyperthecosis. The latter, however, often present with a more severe form of hyperandrogenism with associated virilization. Laboratory evaluation typically shows a normal serum DHEAS level with extremely elevated testosterone levels, often greater than 200 ng/dL.71
Hyperandrogenism, Insulin Resistance, and Acanthosis Nigricans (HAIRAN) Syndrome
A unique disorder of severe insulin resistance associated with hyperandrogenism, HAIRAN syndrome is becoming more widely recognized. It is characterized as follows:73 (1) early age of onset of hyperandrogenism, (2) acanthosis nigricans, (3) marked insulin resistance, (4) positive correlation of the severity of the insulin resistance with the severity of androgen excess, (5) ovarian source for the androgen overproduction, and (6) ovarian hyperthecosis. Most affected women will have normal glucose concentration at the expense of markedly elevated levels of circulating insulin (<80 μU/mL fasting insulin and/or <500 μU/mL after an oral glucose challenge).7 The molecular cause of the insulin resistance in patients with HAIRAN syndrome is still not well understood.
Cushing’s Syndrome
The reported incidence of hirsutism in patients with Cushing’s syndrome is 64% to 81%.74 However, Cushing’s syndrome is a rare cause of hirsutism. Increased adrenal androgen production may accompany the increased production of cortisol. The onset of hirsutism is often distinct from menarche. There may also be increased growth of lanugo hair as a result of the hypercortisolism.75
Hyperprolactinemia
Elevated prolactin levels have been noted in some hirsute women. In a study of 158 women with hirsutism, elevated prolactin was noted in 6% of the women.76 The exact relationship between hyperprolactinemia and hirsutism is still unclear. It is postulated that elevated prolactin level may increase androgen production via an effect on the adrenal cortex. Use of dopamine agonists in hirsute, hyperprolactinemic women has been shown not only to reduce serum androgen levels, but also to improve hirsutism scores.77 On the other hand, the use of bromocriptine in women with PCOS but without hyperprolactinemia has not been demonstrated to alter serum androgen levels.78
Drug-Induced Hirsutism
Multiple medications have been implicated in hirsutism. Anabolic steroids such as danazol, oral contraceptives containing progestins that are 19-nortestosterone derivatives, and medications that can increase serum prolactin have been implicated.4 Among 19-nortestosterone derivatives, first-generation (norethynodrel) and second-generation progestins (norethindrone and its metabolites; levonorgestrel and its derivatives) are more androgenic than the third-generation progestins (desogestrel and norgestimate).79 With the increasing use of testosterone replacement in postmenopausal women, iatrogenic hirsutism will likely occur more frequently.80
APPROACH TO THE PATIENT WITH HIRSUTISM
History
A thorough history is necessary in the evaluation of a woman with hirsutism. Recognizing the patient’s concerns and goals for the visit will allow the physician to tailor the eventual therapy to the patient’s benefit and satisfaction. Most underlying etiologies for hirsutism are benign, considering that it may take months to even years of androgen exposure to transform vellus hair to terminal hair.81
Onset of Symptoms
Increased androgen exposure of the pilosebaceous unit occurs at puberty. Hence, hirsutism often starts at around this time or a few years thereafter. On occasion, it may accompany an early adrenarche. Not infrequently, increased facial hair development in women occurs postmenopausally. It is thought to result from the altered estrogen/androgen balance.82 Rapid hair growth of recent onset should be viewed with suspicion.
Associated Symptoms
Alopecia
Androgenic alopecia, another distressing condition associated with androgen excess, needs to be differentiated from other types of alopecia. Different patterns of hair loss have been described:83
Menstrual History
Oligomenorrhea is one of the features of PCOS. In adolescents, oligomenorrhea that persists after the first few years from the menarche may be an early sign of PCOS.30 Regular menses, however, do not predict normal androgen status in hirsute women. Although 40% of hirsute women will have regular menses, on evaluation, half of these women will be found to have elevated levels of one or more androgens.84
Regular menses do not prove normal androgen status or reliably normal ovulatory/luteal function. In one study, 39% of women reporting normal menstrual cycles actually had oligo-ovulation/anovulation when basal body temperature and day 22 to 24 progesterone levels were measured.36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree