Introduction Hepatobiliary and pancreatic surgery
Historical perspective
Ancient History until the Eighteenth Century
A tablet believed to be from the time of Hammurabi (about 2000 bce), now in the British Museum, names the various parts of the liver and indicates the prognostic significance of each (Jastrow, 1908). The liver was divided into about 50 portions for individual inspection in an effort to overlook as little as possible. Such hepatoscopy was widely in vogue over the following centuries and was practiced by the Etruscans, as evidenced by a bronze tablet in a museum at Piacenza depicting the liver, this being strikingly similar to the Babylonian clay tablet in the British Museum.
The Roman Celsus in his text De Medicina, translated by W.G. Spencer in 1935, mentioned the liver and described its anatomic location: “[T]he liver, which starts from the actual partition under the praecordia on the right side, is concave within (that is on the inferior surface) and convex without; its projecting part rests lightly on the stomach and it is divided into four lobes. Outside its lower part, the gallbladder adheres to it.” Celsus lived in the first century and described symptoms attributable to liver disease. Gallstones were recognized in the embalming of mummies in ancient Egypt. In 1909, a mummy with a preserved liver and a gallbladder containing 30 gallstones was presented to the Museum of the Royal College of Surgeons in London. This mummy came from Deir-el-Bahn at Thebes and was that of a priestess of the twenty-first dynasty around 1500 bce. Elliot-Smith, an outstanding English anatomist and Egyptologist, described the gallbladder as being large and containing “many spherical calculi.” The specimen was destroyed by German bombs during World War II, but the description of it was accepted as evidence that the gallstones contained therein were the earliest specimen of such calculi to have survived from antiquity (Glenn, 1971). Gordon-Taylor, a noted surgical historian in England, had likewise called attention to the terminal illness of Alexander the Great at the age of 34 (323 bce) as an example of fatal biliary tract disease. The description of Alexander’s illness as recounted by Weigall (1933) suggests that he died of complications culminating in peritonitis.
Rhazes (850-923) and Avicenna (980-1037), two Persians, wrote on general surgical topics and the nature of disease and appreciated the gallbladder but lacked knowledge of the common bile duct. Biliary fistulae were known to have formed after the drainage of an abdominal wall abscess, and it was known that individuals with fistulae had a better prognosis than those who had an external communication with the intestines (Glenn, 1971).
Greek academic achievements surpassed that of all other civilizations until the fifth century bce. Hippocrates, widely acclaimed in medicine then and since that time, recognized the seriousness of biliary tract disease as evident in the following passage from The Genuine Works of Hippocrates (translated by Adams in 1939): “[I]n a bilious fever, jaundice coming on with rigor before the seventh day carries off the fever, but if it occurs without the fever, and not at the proper time, it is a fatal symptom.” He also noted that in the case of jaundice, “[I]f the liver hardens it is a bad sign.”
A few centuries after Aristotle recognized jaundice as an element of disease, Galen viewed biliary tract disease as a recognized clinical entity to be treated successfully in part by diet. Although Celsus had drawn attention to the gallbladder and liver in the first century ce, in the second century, Galen was the most noted author of the Greco–Roman age. Galen named three main organs that govern the body: the heart, the source of heat and the principal organ; the brain, the source of sensitivity for all parts; and the liver, as a principal part of the nutritive facility (Green, 1951). Galen considered jaundice to be due to yellow bile flowing into the skin and recognized that although jaundice could be the result of hepatic disease, it also could arise when the liver was not involved at all. Galen’s teaching persisted for centuries, and until the middle of the seventeenth century, many disorders were described as alterations in the balance of the main humors of the body brought about by hepatic dysfunction. As recorded by Rosner (1992), ancient Hebrew physicians used pigeons to treat jaundice by placing the pigeon on the patients umbilicus. “The pigeon will draw all yellowness out.”
Many subsequent advances came from Italy about the time of the Renaissance. Benivieni (1506) in Florence described a series of autopsies in his patients, which was the first record of special reference to biliary tract disease and its clinical manifestations. Two examples are cited in the translation by Singer and Long (1954) of Benivieni’s book, The Hidden Causes of Disease:
The second quotation also suggests death from gallstones:
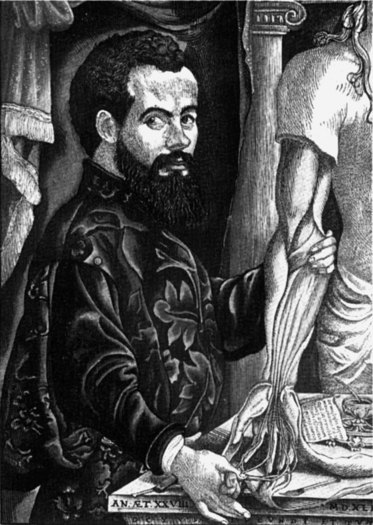
Much of the next phase of development of knowledge was centered around northeast Italy, particularly Padua, and many of the eponyms that we now use in surgery evolved from that period. The publication of Vesalius’s De Humani Corporis Fabrica in 1543 (Fig. 1) and Harvey’s De Mortu Cordis 100 years later marked the emergence of a new scientific spirit in anatomy and physiology. As was the custom of the times, Vesalius often recorded descriptions of findings of dissections on individuals who had recently died and expressed an opinion on the cause of death. Rains (1964), in his treatise Gallstones—Causes and Treatment, stated “Vesalius found [that he had] a hemoperitoneum coming from an abscess, which had eroded the portal vein. The gallbladder was yellow and contained 18 calculi. Very light, of a triangular shape with even edges and surfaces everywhere, green by color somewhat blackish. The spleen was very large.” Similarly, Rains recounted that Falloppio described stones in the gallbladder and common bile duct in 1543, and that Fernell in his De Morbis Universilibus et Particularibus (1588) proposed that the predisposing cause of gallstone formation was stasis and observed that in jaundice, the feces become white and the urine dark, and that stones may be passed per anum. Falloppio, Vesalius, and Fernell all were active in the first half of the sixteenth century and probably discussed their theories of the cause of gallstones and the changes in the liver with which they were associated.
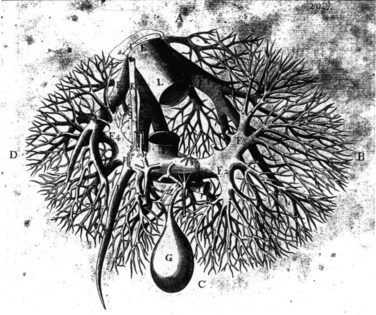
William Harvey (1578-1657), who also worked in Padua, is held by many to be the greatest of the contributors to the study of anatomy and physiology, and he established a clear understanding of the circulation. There is little doubt that Harvey also gave thought to the liver and its relation to the circulation and to the heart in particular. Harvey’s student and younger contemporary, Francis Glisson, investigated the structure and function of the liver extensively. His book Anatomia Hepatis was published in 1654 and is the first major modern work on hepatology. Glisson gave a clear description of hepatic anatomy, especially of the hepatic capsule and of the investment of the hepatic artery, portal vein, and bile duct. He described the fibrous framework of the liver and illustrated hepatic vascular and biliary anatomy on the basis of cast and injection studies (Fig. 2). Glisson was the first to mention a sphincteric mechanism around the orifice of the common bile duct (Boyden, 1936). He also deduced the flow of blood through the portal veins traversing the capillaries into the vena cava at a time when no microscopic studies of the liver had been done (Walker, 1966). Some of his illustrations are remarkably similar to those of Couinaud (1954, 1957, 1981) and to the images displayed today in three-dimensionally constructed computed tomography (CT) scans. Glisson was one of the great clinical physicians of all time, yet his name is related to an anatomic structure of limited importance.
In the century that followed the time of Harvey, great activity in publication among individuals engaged in medicine occurred. As today, senior professors often held opposing opinions and expressed their feelings based on fact or fancy with equal fervor. In an attempt to select the factual, Morgagni, senior professor of anatomy and president of the University of Padua, published in 1761 an analysis of disease (translated by Benjamin Alexander in 1960) under the title Seats and Causes of Disease, among which are those of the liver and biliary tract. In referring to gallstones, this text analyzed the distribution of stones in male and female patients, including the age, incidence, and treatment:
As outlined by Wood (1979), numerous eponyms currently used pertain to the names of these early physicians. Johann Georg Wirsung (1600-1643) also studied in Padua and was the first to dissect the human pancreatic duct and to describe it in a letter to Riola, professor of anatomy and botany at the University of Paris in 1642. Wirsung was subsequently murdered by a Dalmatian physician, the dispute probably related to who had described the duct first (Major, 1954; Morgenstern, 1965). Abraham Vater (1684-1751) was the first to describe the papilla of the duodenum. In 1720, he wrote that “those double ducts (bile and pancreatic ducts) … come together in single combination” (Boyden, 1936). He described not an ampulla but an elevation of the mucosa of the duodenum and described the first case of an ampulla with two orifices. Likewise, the duct of Santorini takes its name from the Venetian Giovanni Domenico Santorini (1681-1737), a brilliant anatomist and one of the most exact and careful dissectors of his day. While Vater was describing the tubercle at the confluence of the pancreatic and bile ducts, Santorini was relating the first detailed observation of the orifice of the two ducts (Boyden, 1936). In observations printed posthumously, Santorini noted a second pancreatic duct of normal occurrence and named the upper one the superior pancreatic duct and the lower one the main pancreatic duct. It was not until Oddi in 1864, working in Bologna, rediscovered “Glisson’s sphincter” and did studies in dogs that the holding quality of the sphincter of the outlet of the choledochus was recognized (Boyden, 1936).
Imaging in Hepatobiliary and Pancreatic Surgery
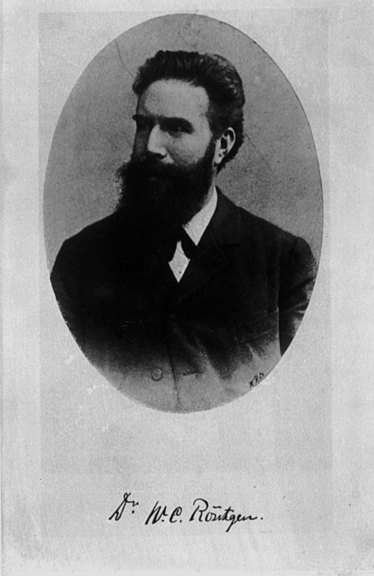
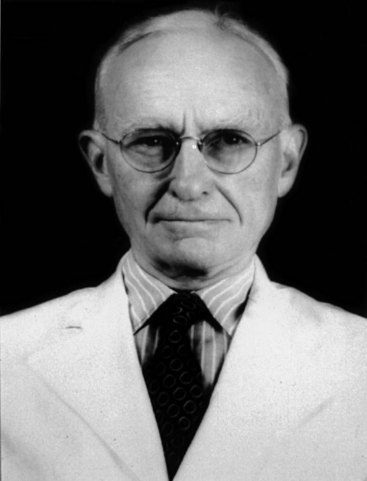
Following the discovery of x-rays by Roentgen (Fig. 3) in 1895, there have been continual important and extraordinary developments in radiology. A contemporary surgeon who examines images to determine the cause of disease, sometimes before taking a history or examining the patient, can hardly contemplate a time when precise imaging was not available. A landmark development in hepatobiliary imaging occurred when, after experimenting with various iodine compounds, Graham, a North American surgeon, developed oral cholecystography (Graham & Cole, 1924). Although biliary calculi had been observed by plain x-rays since 1898 (Buxbaum, 1898), the problem of detecting radiotransparent calculi was evident, and the development of oral cholecystography marked an important turning point. Postoperative cholangiography was soon developed by Mirizzi (1932) in Argentina. Intraoperative cholangiography (Mirizzi, 1937) and choledochoscopy (Bakes, 1923; McIver, 1941) also were developed.
In the 1970s, endoscopic cholangiopancreatography (McCune et al, 1968; Demling & Classen, 1970; Oi et al, 1970; Blumgart et al, 1972; Cotton et al, 1972a, 1972b) and endoscopic papillotomy (Classen & Demling, 1974) revolutionized biliary and pancreatic radiology and approaches to common bile duct stones. The 1970s saw not only the introduction of endoscopic approaches to the biliary tract but also the development of good methods for percutaneous transhepatic cholangiography (Ohto & Tsuchiya, 1969; Okuda et al, 1974), CT of the liver (Grossman et al, 1977), and the use of ultrasound (Bryan et al, 1977) in liver and biliary surgery. Magnetic resonance (MR) axial imaging (Damadian, 1971; Lauterbur, 1973) was conceived and has led to the development of magnetic resonance imaging cholangiopancreatography (MRCP).
Not only were endoscopic and transhepatic approaches to stones now possible, endoscopic and percutaneous transhepatic intubation of the biliary tree for the relief of jaundice and for dilation of strictures became a reality. Arteriography developed to a fine degree, so that good hepatic arteriography and portography were developed (Hemingway & Allison, 1988), which inevitably led to the development of techniques for hepatic artery embolization in the management of liver tumors and of hemobilia (Allison et al, 1977).
Surgery of the Biliary Tract and Pancreas
Biliary Tract
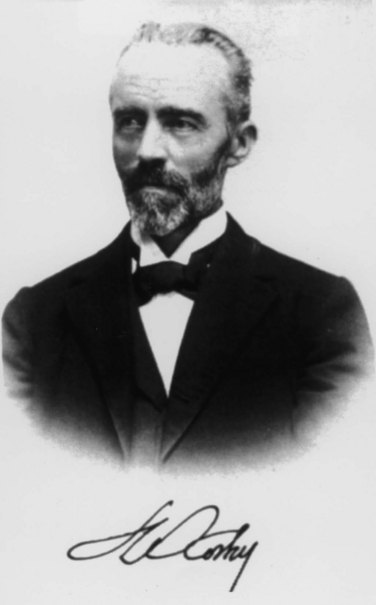
Biliary surgery began in Indiana on July 15, 1867, when John Bobbs operated on a woman who had a large tumor that he believed to be an ovarian cyst. To his amazement, when the abdomen was opened, he found an enormous gallbladder filled with stones. He opened it and extracted the calculi, sutured it carefully, and replaced it back in the abdomen (Bobbs, 1868). It was nearly a decade before a similar cholecystostomy was performed almost simultaneously by a Swiss, Theodore Kocher (Fig. 4), a North American, Sims, and an Englishman, Lawson Tait. All three surgeons planned operations in which the gallbladder was affixed to the abdominal wall to allow extraction of stones and pus and to leave it open to the exterior, so that peritonitis as a result of maneuvers within the abdomen could be avoided.
Sims worked on both sides of the Atlantic, and in Paris he operated on a patient with long-standing jaundice and a tumor in the right hypochondrium. With antiseptic technique, he opened the gallbladder and extracted 60 calculi then sutured the gallbladder to the abdominal wall; this was perhaps the first elective surgical procedure for obstructive jaundice (Sims, 1878). In the same year, in Bern, Switzerland, Kocher performed a cholecystostomy in two stages (Glenn, 1971). In the first stage, he packed the wound with gauze to the bottom of the gallbladder, and 8 days later, he emptied the residual stones from the gallbladder. Incidentally, Kocher, who won the Nobel prize in medicine in 1909 for his work on the physiology and surgery of the thyroid gland, also described sphincterotomy, or internal choledochoduodenostomy. His name is remembered by every biliary surgeon who performs mobilization of the duodenum as described by the great master (Kocher, 1903). Kocher originally described the maneuver for use in gastric surgery, but similar to so many other firsts in surgery at that time, the maneuver was first described by Jourdan (1895) and was first performed in biliary surgery by Vautrin (1896). Perhaps the maneuver should be referred to as “Vautrin’s maneuver” rather than Kocher’s. Tait, the great British surgeon, is given credit for performing the first cholecystostomy for gallbladder lithiasis in one stage. The patient, a 40-year-old woman, survived, and by 1884, he had performed the procedure in 14 cases with only 1 death (Tait, 1885).
The first elective cholecystectomy was done by Langenbuch (Fig. 5). While others were pursuing the construction of biliary fistulae and direct removal of gallstones, Langenbuch observed that because stones were known to recur, others had “busied themselves with the product of the disease, not the disease itself” (Langenbuch, 1882). As he was later to recount, two thoughts kept occurring to him: first, that in animal experiments, Zambeccari in 1630 and Teckoff in 1667 had performed cholecystostomy and cholecystectomy in dogs and had shown that the gallbladder was not essential to life (Langenbuch, 1896); second, that his medical colleagues believed that the gallbladder itself gave rise to stones. He developed the technique for cholecystectomy over several years of cadaver dissection and performed the operation at the Lazarus hospital in Berlin on July 15, 1882. The patient had had biliary colic for 16 years and was addicted to morphine. He was afebrile the day after the operation, had little pain, and was smoking a cigar; the patient was walking at 12 days and left the hospital 6 weeks later, pain free and gaining weight (Traverso, 1976). Report of this case (Langenbuch, 1882) led to a controversy over cholecystostomy as championed by Tait. Langenbuch’s operation was the new cholecystectomy.
In 1886, Gaston had tabulated 33 cholecystostomy operations with a mortality of 27% compared with 8 cholecystectomies (5 by Langenbuch) with 1 death recorded, a mortality of 12%. By 1890, 47 cholecystectomies had been done by 27 surgeons, and in 1897, the number had increased to nearly 100 operations with a mortality of less than 20% (Gaston, 1897).
The most important recent advance in surgery of the gallbladder came 100 years after Langenbuch’s first cholecystectomy. Laparoscopic cholecystectomy was conceived and first performed in Germany by Muhe in 1985. Between 1985 and 1987, he performed 94 laparoscopic cholecystectomies (Muhe, 1986, 1991). Mouret in Lyon, France, performed the first video laparoscopic cholecystectomy. He did not publish his experience, but the news spread rapidly, and Dubois in Paris published the first series of laparoscopic cholecystectomies (Dubois et al, 1989, 1990). Perissat, working in Bordeaux, further developed the laparoscopic approach and introduced it to the United States in 1989 (Perissat et al, 1990). The procedure has since been extended, so that laparoscopic exploration of the common bile duct is now possible and is routinely carried out. Today, most cholecystectomies are done using laparoscopic techniques, such that the modern surgical trainee often has little or no experience in open cholecystectomy. More recently, cholecystectomy has been done via minimally invasive techniques using robotics (Marescaux et al, 1998; Satava, 1999) to manipulate the instruments.
Not long after the performance of the first cholecystectomy, attempts were made to remove stones from the bile ducts. In 1898, Thornton performed the first removal of a stone from the common bile duct. A year later, Courvoisier operated successfully on another case of choledocholithiasis and published his well-known monograph on the pathology and surgery of the biliary ducts. He also enunciated the law that was to bear his name, which established that in cases of jaundice, if the gallbladder is not distended, the case is more likely to be one of stones. The operative procedure for exploration of the common bile duct for choledocholithiasis was not popularized, however, because of the risk of peritoneal infiltration of bile.
In 1897, Kehr (Fig. 6) performed the procedure and placed a rubber tube in the common bile duct through the cystic duct; this was the first systematic use of biliary intubation. Kehr’s name is properly associated with the development of biliary intubation; Kehr (1912) and Quenu and Duval (1908) were able to extract stones along the tunnels created by the drainage tubes. These were the precursors for techniques later developed by Mondet (1962) and Mazzariello (1966, 1974). Kehr had developed numerous combinations of drainage in patients with biliary stones, and many other surgeons rapidly developed choledochotomy without suture and using tube drainage.
Surgery of the bile ducts rapidly disseminated across Europe, England, and the United States, and in 1912, Kehr developed what came to be known as the T-tube. Not only was choledochotomy simplified, but biliary tract repair was done over these tubes. Kehr became justly famous for his introduction of biliary intubation and was probably the most outstanding biliary surgeon of his day. In 1913, he published a treatise entitled Surgery of the Biliary Tract, which for more than 40 years was the most respected text on the subject. Kehr (1908a, 1908b) described the resection of cancerous gallbladders, including hepatic resection, and he resected hepatic tumors and aneurysms of the hepatic artery. He also performed the first hepaticoenteric anastomosis.
Before the development of Kehr’s tubes, choledochotomies often became biliary fistulae, either because of residual supraampullary stones, or because the surgeon had inadvertently opened the bile duct proximal to a cancer. German and Austrian surgeons were the first to perform supraduodenal choledochoduodenostomy (Riedel, 1892; Sprengel, 1891). Sprengel’s operation described a side-to-side choledochoduodenostomy, and it subsequently became popular in Europe and the United States (Madden et al, 1965). Cholecystenterostomy also was developed initially by von Winiwarter (1882) and was used later by many surgeons, including Oddi (1888).
Transduodenal surgery was not long in developing. In 1895, Kocher wrote an article on internal choledochoduodenostomy to remove supraampullary choledochal calculi; by 1899 he had performed the operation 20 times. MacBurney (1898) published his experience with duodenostomy and papillotomy in patients with impacted periampullary calculi. These early procedures of a choledochotomy and choledochoenteric anastomosis for the treatment of jaundice and of stones in the biliary tract are still used today, with frequent application of the same principles but with the use of the endoscope.
At about the same time, surgeons began to operate on cancer of the papilla. In Baltimore in 1900, Halsted resected a portion of the duodenum that included a tumor and reimplanted the common duct, at the same time performing a cholecystostomy. He then reoperated to remove the gallbladder. Mayo (1901) reported an operation on a 49-year-old man with papillary cancer. Mayo opened the duodenum, removed the tumor, and carried out a choledochoduodenostomy. This was the first transduodenal ampullectomy. Kausch (1912) in Germany and Harmann (1923) in France gave accounts of resections of ampullary tumors. In Lausanne, Switzerland, Roux, a disciple of Kocher, had described preparation of a “jejunal loop” for use in gastric surgery, and it soon became an adjunct in biliary surgery (Roux, 1897). This Roux-en-Y procedure was soon used by Monprofit (1904) in the performance of cholecystojejunostomy, and he proposed it for hepaticojejunostomy at the French Congress of Surgery in 1908. Dahl (1909), in what he called “a new operation on the bile ducts,” was the first to advocate the Roux anastomosis in biliary surgery.
With the advent of cholecystectomy and choledochostomy came the inevitable sequelae of residual bile duct stones and iatrogenic lesions. Initially, these were treated by various forms of intubation, similar to the techniques advocated by Kehr, but many leading surgeons, such as Moynihan and Mayo, used hepaticoduodenal anastomoses (Estefan et al, 1977). Dahl (1909) used the Roux-en-Y loop, but more recently, other authors (Madden et al, 1965; Schein & Gliedman, 1981) have preferred choledochoduodenostomy as described previously.
Operative biliary drainage in upper biliary tract cancer and in patients with severe scarring in the porta hepatis is always difficult. Kehr (1913) successfully performed three operations in which he fixed a jejunal loop to a cut section of a hepatostomy wound; similar procedures were done by others, as cited by Praderi (1982). Longmire and Sanford (1948) performed a similar operation, resecting the end of the left lobe of the liver and anastomosing it to a jejunal loop. This technique, although popular for a short time, was complicated by stenosis and has fallen out of favor.
Goetze (1951) developed a procedure of transanastomotic drainage with a catheter that went through the hepatic parenchyma, the anastomosis, and the jejunal loop. Goetze’s contribution was apparently forgotten but was reinvented and popularized by others, including Praderi in 1962 (Praderi, 1982). Praderi argued strongly that Goetze’s procedure was the answer to difficult procedures in the high biliary tract but conceded that the development of transhepatic percutaneous cholangiography (Okuda et al, 1974) allowed for the development of transhepatic percutaneous methods for intubation and dilation of the biliary tract, which are now common procedures throughout the world.
The greatest advances in techniques for repair of biliary injuries came from two sources. At the Lahey clinic in the United States, three generations of famous surgeons headed by Lahey, Cattell, and Warren perfected the reconstruction of the common bile duct as an immediate or delayed procedure and splinted their anastomoses with a variety of tubes (Estefan et al, 1977). The results of these techniques were unsatisfactory, with numerous recurrent strictures. However, following the detailed study of the anatomy by Couinaud in France (1954), Hepp and Couinaud (1956) and Soupault and Couinaud (1957) developed techniques for direct biliary–enteric anastomosis, either to the left hepatic duct or to the segment III duct of the left liver. These surgical techniques have become widely accepted and are used throughout the world (Bismuth & Corlette, 1956; Bismuth et al, 1978; Voyles & Blumgart, 1982; Warren & Jefferson, 1973).
Pancreas
Like liver surgery, pancreatic surgery developed largely as a result of responding to wounds inflicted in wars. Claessen (1842), Ancelet (1866), Da Costa (1858), and Nimier (1893) documented the early development of pancreatic surgery. In 1923, Harmann wrote an extensive review of the French, German, and English literature. Early efforts at elective pancreatic surgery largely revolved around drainage of cysts (Thiersch, 1881). In 1883, Gussenbauer marsupialized a pancreatic pseudocyst, and the patient survived. Other surgeons, including Senn (1886), soon performed similar procedures.
Direct anastomosis of the pancreas to the gastrointestinal tract followed in the early part of the twentieth century, when Coffey (1909) performed an anastomosis of the tail of the pancreas to the small bowel. Ombredanne (1911) anastomosed a pancreatic cyst to the duodenum, and Jedlicka (1923) anastomosed a cyst to the posterior wall of the stomach. Chesterman (1943) performed a cystojejunostomy, and König (1946) carried out the same operation to a Roux-en-Y loop of jejunum.
Operations for pancreatic tumors were being done at about the same time. Ruggi (1890) reported a resection of a large lesion of the tail of the pancreas, and Briggs (1890) performed a similar operation. Biondi (1897) reported resection of a tumor arising from the inferior part of the head of the pancreas, and the patient was still alive 18 months later.
Whipple (Fig. 7) and associates (1935) published a technique for cephalic duodenopancreatectomy, done in two stages, for cancer of the ampulla of Vater. In the first operation, they performed a cholecystogastrostomy and gastroenterostomy. In the second and subsequent procedure, they resected the head of the pancreas with a portion of the duodenum without anastomosis to the stump of the pancreas, which they sutured. Whipple (1941) subsequently performed this operation in one stage and reported 41 cases with a mortality of 27%. Eventually, the technique of this operation was perfected. Although English-speaking surgeons throughout the world continue to call this operation “Whipple’s operation,” the procedure had been done many years before.
Sauve (1908) reviewed the literature on pancreatectomy and reported that several surgeons had resected small tumors from the head of the pancreas, and larger ones from the body of the organ, without touching the duodenum. Codivilla of Italy is reported to have resected the duodenum and head of the pancreas and performed a cholecystojejunostomy in 1898, but the patient died in the postoperative period. The first surgeon to perform cephalic pancreaticoduodenectomy successfully was Kausch, a professor of surgery in Breslau and later in Berlin. On June 15, 1909, he performed a cholecystojejunostomy on a jaundiced 49-year-old man; on August 21, 1909, Kausch reoperated, performing a posterolateral gastroenterostomy and resection of the head of the pancreas with the tumor, the pylorus, and the first and second part of the duodenum. He anastomosed the third portion of the duodenum to the pancreatic stump. Kausch (1912) published a report entitled “Cancer of the Duodenal Papilla and Its Radical Treatment.” He gathered in that publication all reports that included excisions of the papilla. Tenani (1922) reproduced this operation with success, also in two stages but with one difference: Tenani performed a choledochojejunostomy, and the patient survived 3 years. Kausch and Tenani, although cited by Whipple (1941), are generally ignored in the English and American literature.
Resection later was extended to deal with cancers of the common bile duct and of the duodenum (cancers of the proximal bile duct are described subsequently in the section on liver surgery). Recognition of endocrine tumors of the pancreas later led to operations for these conditions. Wilder and colleagues (1927) reported the first case of resection of an insulinoma arising from the islet cells of the pancreas. Mayo operated on a patient in whom he found a tumor of the pancreas with metastases to the liver, and an extract from one of the metastases produced an insulin-type reaction when injected into a rabbit. Graham and Hartman (1934) reported subtotal pancreatectomy for hypoglycemia, and total pancreatectomy was performed by Priestley and colleagues (1944) for a patient in whom there was proven hyperinsulinism, but no tumor of the pancreas was to be found. The patient was cured by the operation, and the small tumor causing the syndrome was discovered during the pathologic examination.
Later, Fallis and Szilagyi (1948) performed total pancreatectomy for cancer, and this procedure was developed further in the hope that total removal of the gland would reduce morbidity and mortality and perhaps lead to better results. ReMine and colleagues (1970) and Brooks and Culebras (1976) adopted this approach, but early suggestions regarding efficacy were not fulfilled, and total pancreatectomy for pancreatic cancer has largely been abandoned. Fortner (1973) described the even more extensive procedure of regional pancreatectomy. The operation included an extensive total pancreatectomy and resection of the pancreatic segment of the portal vein—and sometimes the hepatic and superior mesenteric arteries, if these vessels were invaded by tumor—together with subtotal gastrectomy and regional lymph node dissection. Fortner’s results have not been reproduced by others.
Surgery for pancreatitis also developed over the same period, and the severity of acute pancreatitis was recognized. Ockinczyc (1933) revealed the frustration of the times when he advocated “the use of drainage of the pancreas and hope.” Because the mortality of emergency surgery reached 78%, the conservative approach to acute pancreatitis was advocated. Nevertheless, some patients with acute pancreatitis still came to operation because of the necessity to treat gallstones and pancreatitis or to deal with complications, such as abscess and pseudocyst (Cattell & Warren, 1953).
The development of intensive care, antibiotics, and better metabolic management of patients with acute pancreatitis led to improvements in outcome, although the death rates remained unacceptably high. Ranson and colleagues (1976) and Imrie (1978)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree