5th (1997)
6th (2002)
7th (2010)
0
TisN0M0
TisN0M0
TisN0M0
Ia
T1N0M0
T1N0M0
T1N0M0
Ib
T2N0M0
IIa
T2N0M0
T3N0M0
T2N0M0
IIb
T1-3N1M0
IIIa
T3N0M0,T1-3N1M0
T4NxM0
T3N0M0
IIIb
T1-3N1M0
IVa
T4N0M0,T4N1M0
TxNxM1
T4N01M0
IVb
TxN2M0,TxNxM1
TxN2M0,TxNxM1
22.4 Hepatectomy for Gallbladder Carcinoma
22.4.1 Surgical Treatment Principles
Gallbladder cancer therapy is divided into curative and palliative treatment. Curative therapy is used to treat early cancer, whereas palliative treatment is for patients with advanced cancer. Because the gallbladder is not sensitive to radiotherapy or chemotherapy, surgical resection is the only effective curative method. Gallbladder cancer is an incurable malignancy. R0 resection margin represents a curative resection. Survival of patient with R1 or R2 resection is similar to that without surgical resection. The T stage of gallbladder cancer has a direct impact on its N and M stages. The cure rate is higher when T stage is in the earlier period [8, 9].
The surgical approach for gallbladder cancer depends on the patient’s clinical and pathological staging [10]. We used the American Joint Committee on Cancer Staging Manual, 7th edition, as a guide for the staging of gallbladder cancer [7]. For early gallbladder cancer (Tis and T1a tumors), the prognosis after cholecystectomy is very good and no further treatment is needed for these patients [11]. In recent years, considerable evidence has been published in support of the use of radical cholecystectomy to treat T1b gallbladder cancer [12], but some studies have suggested that extended resection for T1b gallbladder cancer is still debatable [13]. T2 gallbladder cancer should be treated with radical resection methods. Radical cholecystectomy includes resection of gallbladder and adjacent liver tissue + skeletonized hepatoduodenal ligament.Resection of the gallbladder surrounding liver tissue includes the followings:
2.
3.
If the left liver volume is <20 % of the total liver volume, a right portal vein thrombosis could be developed prior to right hepatectomy [22]. A case of T3 tumor should undergo liver resection + near violated organ removal (including the colon, duodenum, stomach, and pancreaticoduodenectomy) [20, 21]. Pancreaticoduodenectomy has a high complication rate and high mortality, with low 2-year survival rates, and as a result, it is not universally accepted [20, 21]. The survival rate of patients with combined portal vein or hepatic artery resection is very poor, so it is not generally carried out even in Japan [22–26]. For T4 tumors, although there are few opportunities for surgical resection, and the survival rate is very poor, a radical resection should be performed as far as possible [27]. A prior laparoscopy is beneficial to know whether a radical cholecystectomy could be carried out. Lymph node dissection remains controversial; the current consensus view is to produce a clean liver ligament, that door vein, and the hepatic artery and its branches [14, 20, 27–30]. Bile duct resection should be performed in the following cases: ① when the cystic duct is invaded by the tumor and ② when extended right hepatectomy is carried out to achieve R0 resection for gallbladder carcinoma with common bile duct invasion [31–33].
22.4.2 Preparations for Hepatectomy of Gallbladder Carcinoma
1.
Liver function assessment: Because a considerable number of gallbladder patients have jaundice or need major liver resection, preoperative assessment of liver function is critical.
2.
Protection of liver function: When the serum total bilirubin is more than 256.5 μmol/L, PTCD should be used to relieve jaundice; intravenous administration of vitamin K1 and fresh plasma is needed to correct the clotting mechanism; exogenous glutathione can maintain liver cell membrane stability; and the addition of many vitamin C, branched-chain amino acids for the preoperative liver can have a protective effect.
3.
Determine whether the tumor is resectable: In addition to considering the general condition and whether the patient’s liver function can tolerate surgery, local conditions determine whether the tumor is removable. First, whether there are violations of the liver and the extent of the violations should be clear. If there is only direct tumor invasion of liver without liver metastasis, it is possible that liver wedge resection or 4/5 segmentectomy can be used. Semi-hepatectomy can be performed if the tumor is confined to the infringement of half of the liver. Surgical resection is not an option if multiple liver metastases exist. Second, determining whether the hilum has been violated is important: whether surgery is not possible if there are hilar lymph node invasion, tumor integration into the metastatic lymph node, class I hepatic buct invasion, and the hilar can not be dissected. Third, it is necessary to evaluate the presence of abdominal lymph nodes and abdominal metastases. It is more difficult to diagnose these issues using the current commonly used imaging method. A diagnostic laparoscopic testing before laparotomy is necessary.
22.4.3 Radical Resection of Early Gallbladder Cancer: Liver Wedge Resection
Surgical procedures include en bloc resection of gallbladder, surrounding liver tissue within the range of 2–4 cm, liver ligament lymph tissue with nerves and adipose tissue, as follows:
Get Clinical Tree app for offline access

1.
Open: inverted “L” incision under the right costal margin.
2.
Exploration of the peritoneum and abdominal visceral and regional lymph node metastases.
3.
Pulling forward on the right rib cage with retractor. Pressuring stomach and small intestine to the lower left side of the abdomen with wet gauze, and then to expose the liver hilar and lower areas (Fig. 22.1).
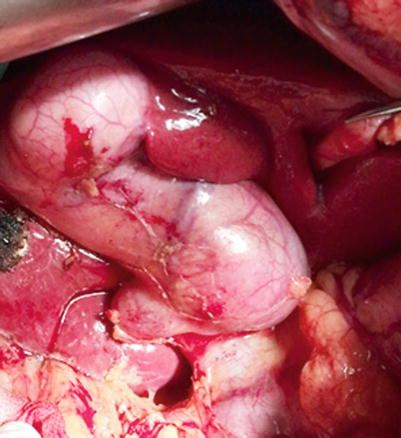
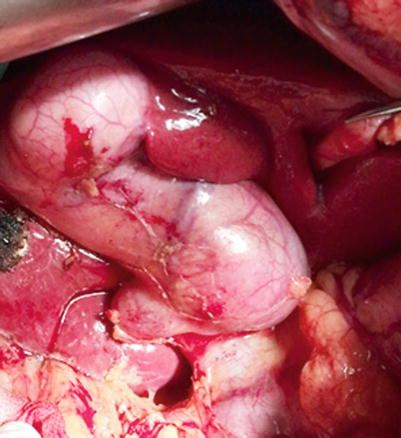
Fig. 22.1
Exposing the hepatic hilum and gallbladder
4.
Cutting the peritoneum outside of the duodenum to free descending part of the duodenum and pancreatic head to remove the surrounding lymph nodes.
5.
Skeletonization of the hepatoduodenal ligament: skeletonization of the portal vein, proper hepatic artery, hepatic artery, right and left hepatic arteries, and splenic artery should be performed. All the lymph nodes, nerve, fiber and fat tissues in the hepatoduodenal ligament and in the gallbladder triangle should be removed completely with the branch vessels ligated. All lymph nodes of the group 5, 7, 8, 9, and 12 were completely excised (Fig. 22.2).
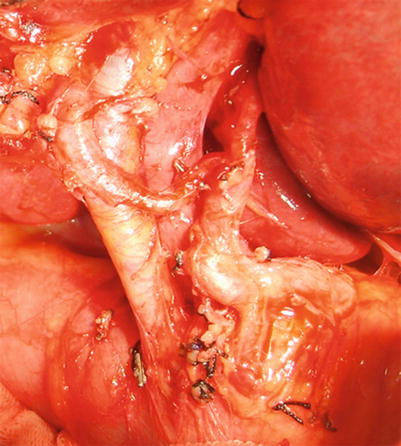
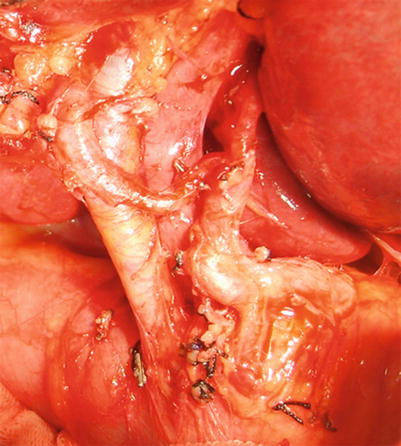
Fig. 22.2
Skeletonization of the hepatoduodenal ligament
6.
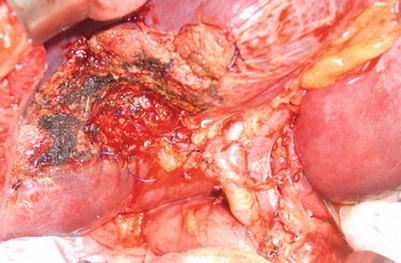
Cystic artery be ligated and cut. Cystic duct excision is performed. Cystic duct margins are routinely submitted to pathological department for evaluating margin free. If there is tumor embolus within the cystic duct, the tumor embolus should be taken out, and even the main bile duct should be opened and probed (Fig. 22.3).
Fig. 22.3
Common bile duct exploration to retract the tumor embolus (a). Radical cholecystectomy + common bile duct exploration + skeletonization of the hepatoduodenal ligament as well as the removal of the regional lymph nodes (b)
7.
Wedge resection of the liver tissue within 2cm of the gallbladder bed is performed. The gallbladder and the wedge resected hepatic tissue within 2 cm of the gallbladder bed as well as all the lymph and fat tissues in the hepatoduodenal ligament be removed by en bloc resection (Fig. 22.4).