Fig. 12.1
Blocking the inflow of the corresponding hepatic lobes or hepatic segments. A: The basis of the round ligament, right side; B: inferior margin of the quadrate lobe, near the left end of the hilar plate; C: the basis of the round ligament, left side; D: superior margin of the quadrate lobe, near the left end of the hilar plate; E: inferior margin of the quadrate lobe, near the capsule bed; F: inferior margin of Glisson’s pedicle near the portal vein branches, right side; G: fissure of Ganz. LMS left branch of Glisson’s pedicle, RMS right branches of Glisson’s pedicle, CP cystic plate, the arrows indicate the round ligament
Advantages
This technique addresses hepatic ducts without opening Glisson’s sheath, saves time, and avoids potential damage to the hepatic portal.
Disadvantage
This technique requires adept operative skills and solid hepatic anatomy, and it may cause duct injury when there is variation in the hepatic portal.
12.1.2 Techniques
Take the right costal margin incision along the midline directly up to the xiphoid. Confirm that there are no intrahepatic metastases or intra-abdominal metastases. Cut the falciform ligament and the round ligament, and reserve the stump of the round ligament for traction. Dissect the coronary ligament until the conjunctive region of the suprahepatic inferior vena cava, hepatic vein, and inferior vena cava is exposed. Cut off the left side of the deltoid ligament and completely dissociate the left liver. Locate the tumor and confirm the relationship between the cancer and the intrahepatic ducts with intraoperative ultrasound.
12.1.2.1 Hepatic Left Lateral Lobectomy
Control the Inflow of Left Lateral Lobe
Blood into the left lateral lobe (including the S2 and S3) is supported by the left Glisson’s pedicle branches along the left side of the fissure of the round ligament. A small incision on the left side is the basis for the fissure of the round ligament (Fig. 12.1); then, make an incision on the front of the left venous ligament and left Glisson’s pedicle branch confluence (Fig. 12.1). Use long curved forceps for blunt dissection from site C to site D until the curved forceps pierce site D. Then, a tourniquet can surround the left Glisson’s pedicle branches with the curved forceps traction until the branches are broken off.
Parenchymal Transection
Resect the liver at the diaphragmatic surface along the left border of the falciform ligament, at the visceral surface along the left border of the round ligament, and toward the Arantius ligament follows an order of a superior-inferior movement and then an inferior-superior movement. Because the inflow of the left lateral lobe and bile duct has been amputated, the hepatectomy can be performed more quickly. After exposing the left hepatic vein trunk, amputate it, and reinforce the stump with 5/0 polydioxanone suture (PDS) wire. Remove the entire specimen, staunch the bleeding, place the drainage tube, and close the abdomen.
12.1.2.2 Left Hemihepatectomy
Control the Inflow of the Left Liver
Dissect the left Glisson’s branches at the left side of the hilar plate, which will avoid injury to the blood vessels and bile ducts if there is anatomical variation of the hepatic portal. Using the confluence of the left Arantius ligament and left Glisson’s pedicle branches as a guide, safely and quickly dissect the left Glisson’s pedicle branches. Make a small incision at the inferior border of the fissure of the round ligament, and dissect the front confluence of the left Arantius ligament and left Glisson’s branch (Fig. 12.1) to expose the back of left Glisson’s pedicle branch. Then, use long curved forceps for blunt dissection from site B to site D, encircle the left Glisson’s branch with a tourniquet and amputate the left branch (Fig. 12.2).
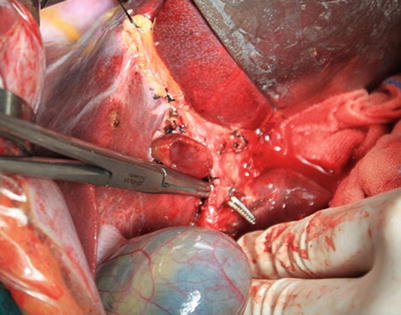
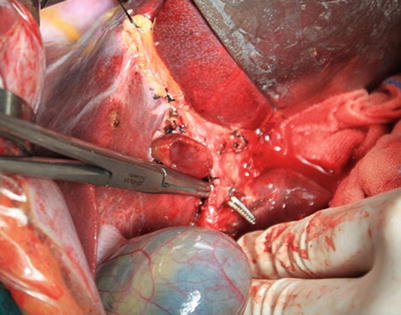
Fig. 12.2
Isolating the left Glisson’s branch at the end of left hilar plate
Parenchymal Transection
After occlusion of the left hepatic inflow, a significant ischemic line appears on the liver surface; the hepatectomy starts from this line. Make an incision along the left hepatic vein following an order of a superior-inferior movement and then an inferior-superior movement. Intraoperative ultrasound can help locate the middle hepatic vein when necessary. After exposing the left hepatic vein trunk, amputate it, and reinforce the stump with 5/0 PDS wire. When the tumor affects the caudate lobe and the caudate lobe must be resected, resect the liver along the line as described until arriving in the front of the inferior vena cava. Then, pull the caudate lobe and left liver to the left, expose the front and left side of the retrohepatic inferior vena cava, and ligate the short hepatic vein from inferior to superior. After the back of left hepatic vein is completely exposed, ligate and suture it. Remove the entire specimen, staunch the bleeding, place a drainage tube, and close the abdomen.
12.1.2.3 Right Hemihepatectomy
Control the Inflow of the Right Liver
Make a small incision on the right side of the confluence of the caudate lobe, gallbladder bed, and far right side of the hilar plate (Fig. 12.1), up to the level of the hepatoduodenal ligament. Expose the connective tissue at the inferior border of the hilar plate. Reveal the caudate branch after careful dissection. Dissect, ligate, and suture this branch; blunt dissection can occur from this branch to incision E until the entire right Glisson’s pedicle trunk is dissected. Amputate the trunk, and suture the ends (Fig. 12.3).









