Fig. 25.1
Cross-section view of a flexible ureteroscope showing the optical system and 3.6 Fr working channel (a). Figure 23.1a from Cohen JH, Grasso III, M. Ureteroscopy for Upper Ureteric and Renal Stones: Overcoming Difficulties with the Flexible Approach. In: Difficult Cases in Endourology Al-Kandari A, Desai M, Shokeir AA, Shoma AM, Smith AD, editors. New York. Springer Science + Business Media; 2013. Reprinted with permission. Modern fiberoptic flexible ureteroscopes typically have a 7.5 Fr tip diameter, a shaft diameter of 8.1–8.5 Fr (b)
One-to-one torquability (rotating the flexible ureteroscope at the handle facilitates the same degree of tip rotation) and logical active deflection (lever down leads to tip down) of up to 270° facilitate accurate placement of the flexible ureteroscope throughout the upper urinary tract (Fig. 25.2). Active tip deflection by depressing the endoscope lever is enhanced by passive distal shaft deflection, often required to access the lower pole. With the instrument hand lever maximally depressed, the instrument is advanced causing buckling at a predetermined shaft segment. This maneuver, termed passive deflection, is useful in placing endoscope accessories into a particularly dependant lower pole calyx. Accessory equipment, such as a 365-μm laser fiber and a 2.4 Fr Nitinol basket decrease tip deflectability, but their application is enhanced with this maneuver.


Fig. 25.2
270° tip deflection is demonstrated. Figure 23.1b from Cohen JH, Grasso III, M. Ureteroscopy for Upper Ureteric and Renal Stones: Overcoming Difficulties with the Flexible Approach. In: Difficult Cases in Endourology Al-Kandari A, Desai M, Shokeir AA, Shoma AM, Smith AD, editors. New York. Springer Science + Business Media; 2013. Reprinted with permission
Technique
Ureteroscopy begins with cystoscopic evaluation of the bladder to both evaluate the lower urinary tract urothelium and define the location and caliber of the ureteral orifices. A 5-Fr open-ended ureteral catheter and real-time fluoroscopy are employed for a contrast-based retrograde pyelogram, defining ureteral and calyceal anatomy. The bladder is then drained completely, and the flexible ureteroscope passed into the bladder. Sufficient irrigant (typically 50–60 cc) is instilled to lift the back wall of the bladder off of the trigone, which aids in identifying the ureteral orifice. If the bladder is over distended, the intramural tunnel is compressed, making ureteral cannulation with the endoscope challenging.
The ureteral orifice is gently cannulated with the flexible ureteroscope under direct vision and then directed proximally (Fig. 25.3). If a ureteral peristaltic wave is encountered, retrograde passage is transiently paused until the wave has passed. Once in the kidney, a complete mapping of the collecting system is routinely performed. Instillation of dilute radio-opaque contrast thru the working channel of the ureteroscope can be employed as a map for subsequent endoscopic inspection. Lower pole calyces can be challenging to visualize, particularly if associated with a narrow or angled infundibulum. The combination of maximal active tip deflection with passive proximal shaft buckling (i.e., secondary deflection) will often help facilitate endoscope placement in this setting (Fig. 25.4).
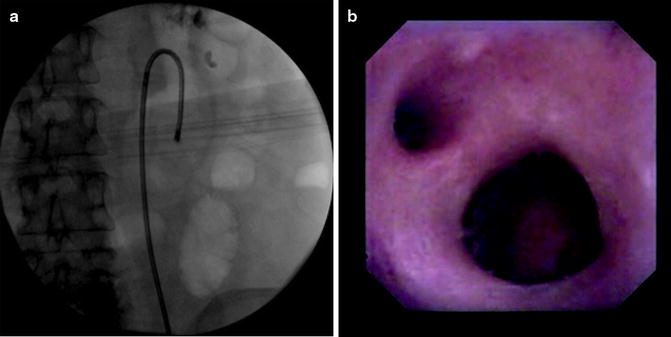
Fig. 25.3
View of the right ureteral orifice through the ureteroscope (a). A peristaltic wave is encountered in the mid-ureter (b)
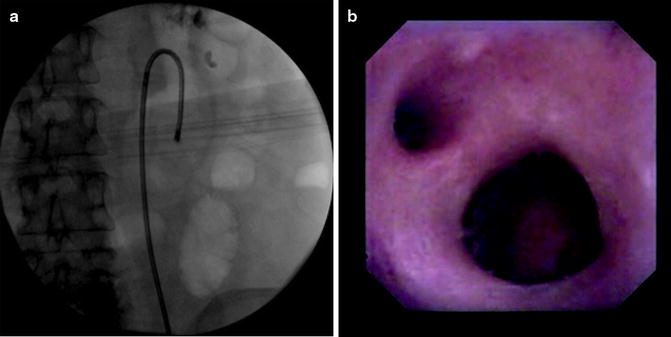
Fig. 25.4
Secondary active and passive deflection is required to achieve access to this right, lower-pole calyx (a). Endoscopic view of anterior and posterior mid-pole calyxes from the renal pelvis (b)
Irrigant is employed thru the working channel of the endoscope to clear the optical lens of debris and to distend the collecting sufficiently for inspection. A simple irrigation system commonly employed is based on two refillable 60 cc syringes joined to a 3-way stopcock attached to the endoscope with standard Luer-lock ended tubing (Fig. 25.5). The assistant instills sufficient irrigant to clear the optical field, varying the pressure and flow as needed based on the clinical presentation. Normal saline is the most common irrigant employed for diagnostic ureteroscopy and endoscopic lithotripsy. If electrocautery is to be employed for fulguration, sorbitol is the preferred irrigant. Small aliquots of sterile water can also be used in this setting and is particularly useful when encountering a bloody endoscopic field of view.
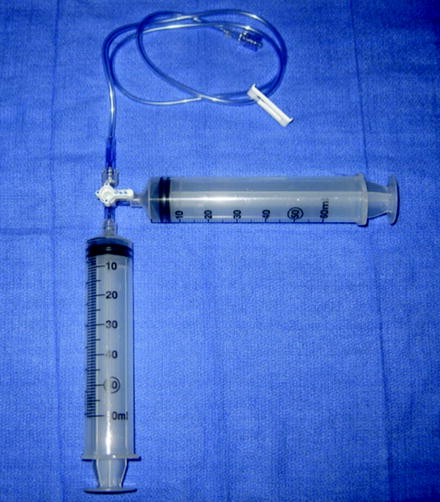
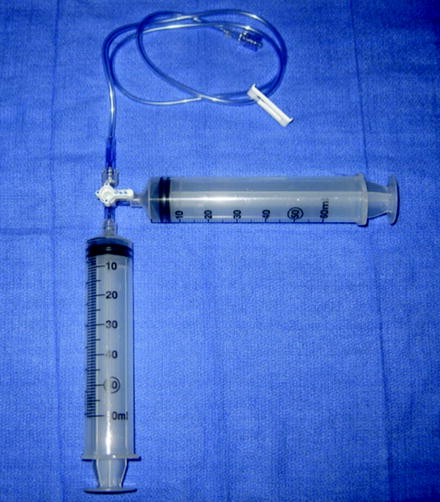
Fig. 25.5
Two 60 cc syringes connected through a 3-way stopcock to Luer-lock extension tubing allows variation in pressure and flow while irrigating
Difficult Endoscope Access: Broadening the Algorithm
No-touch flexible ureteroscopic access is employed when technically feasible for the reasons previously defined. Commonly, a tight ureteral orifice or a tortuous intramural ureter will prohibit endoscope placement. In this setting a flexible tipped guide wire is passed thru the working channel of the endoscope and the distal ureter is intubated under direct vision. This maneuver frequently facilitates endoscope passage thru a tortuous or kinked segment of the ureter, straightening the ureter while providing increased shaft rigidity. Once the narrowed or tortuous segment is traversed, the guide wire is removed and the remainder of the ureter and collecting system inspected without a wire in place.
If the intramural ureter is narrowed, a common finding in young males, and a guide wire alone will not facilitate access, intramural dilation is required (Fig. 25.6). Dilators with the smallest caliber outer diameter cause the least ureteral trauma and are preferred. The intramural ureter is actively dilated with either a 6–12 Fr graduated dilator (i.e., Nottingham dilator, Boston Scientific, Natick Mass.), or a balloon dilator (5 Fr delivery sheath, 12 Fr inflated outer diameter, 4–10 cm long balloon). Dilation is performed over a teflon sheathed kink-resistant, nickel-titanium guide wire (Zebra wire, Boston Scientific, Natick, MA). The more costly balloon dilation can be less traumatic with only circumferential dilating force, as compared to gradual dilators which have the added shearing force. After active intramural dilation, the flexible ureteroscope is then passed over the guide wire to begin the endoscopy.
Fig. 25.6
Procedural algorithm. Asterisk: Complicated defined by prolonged procedure, infection, ureteral edema/trauma, congenital obstructive anomaly, or significant residual stone burden. Figure 23.2 from Cohen JH, Grasso III, M. Ureteroscopy for Upper Ureteric and Renal Stones: Overcoming Difficulties with the Flexible Approach. In: Difficult Cases in Endourology Al-Kandari A, Desai M, Shokeir AA, Shoma AM, Smith AD, editors. New York. Springer Science + Business Media; 2013. Reprinted with permission
If the flexible ureteroscope cannot traverse the ureteral orifice after active dilation, a mucosal lip or fold may be inhibiting progress. In that setting a small caliber semirigid ureteroscope is employed to inspect this segment. The passage of the graduated semirigid endoscope will also facilitate ureteral dilation in this setting. There are certain clinical presentations where after the aforementioned maneuvers, the endoscope will not pass proximally. Patients with prior retroperitoneal surgery or radiotherapy causing marked ureteral fibrosis may prohibit diagnostic ureteroscopy. In this setting, performing a staged procedure by first placing an ureteral stent to facilitate passive dilatation of the ureter over time is a useful technique.
Management of Upper Urinary Tract Urothelial Tumors
Atraumatic ureteroscopic examination of the upper urinary tract is crucial in the setting of diagnosing and treating upper urinary tract tumors. No-touch flexible ureteroscopy, if technically feasible, facilitates a pristine inspection of the urothelium, minimizing bleeding and inadvertent urothelial trauma. In addition, the application of an access sheath in this setting may disrupt a papillary lesion or obscure distal ureteral tumors and thus are infrequently employed, particularly during diagnostic endoscopic mapping (Fig. 25.7).
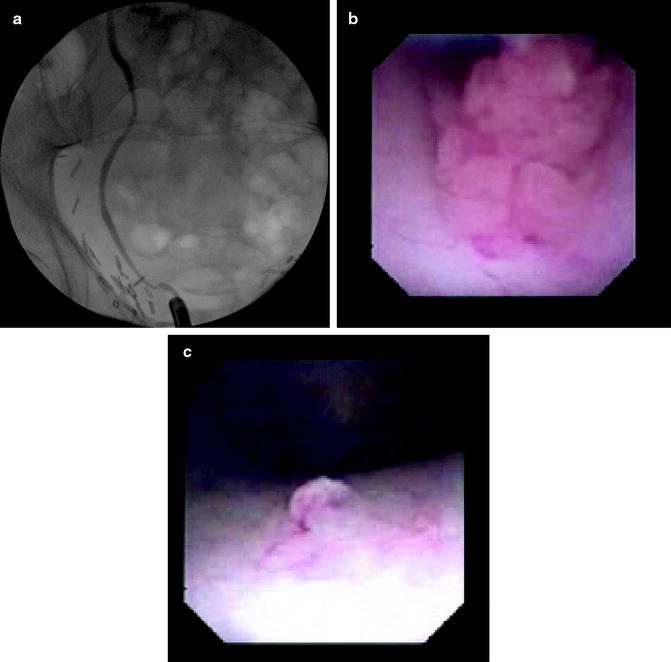
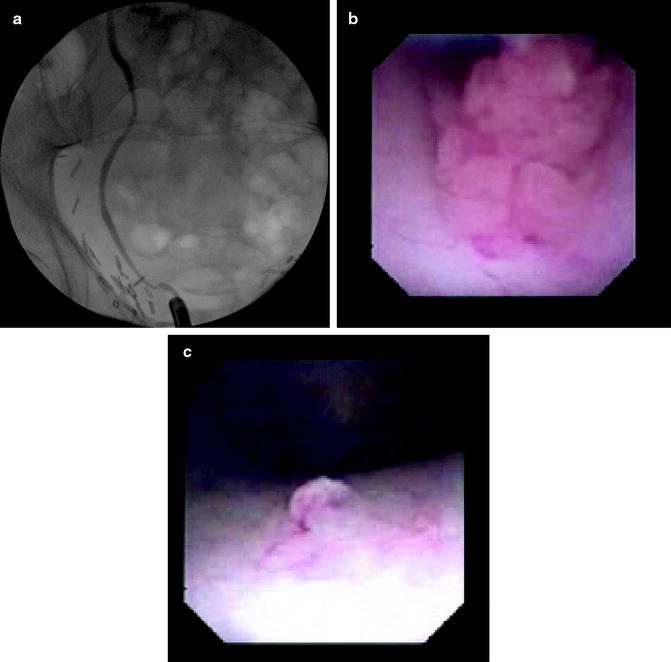
Fig. 25.7
Normal retrograde pyelogram in a patient with a history of prior pelvic surgery and upper tract urothelial cancer (a). No-touch ureteroscopy was performed, revealing a 5 mm right distal ureteral tumor that did not manifest as a filling defect on the retrograde pyelogram (b). A 1 mm tumor in the renal pelvis easily appreciated with atruamatic inspection of the upper urinary tract without prior sheath or wire placement (c)
Cystoscopic mapping of the lower urinary tract urothelium, bladder barbotage for cytological evaluation, and retrograde pyelograms are performed prior to diagnostic ureteroscopy. A small aliquot of dilute contrast is instilled thru a 5 Fr angiographic ureteral catheter under real-time fluoroscopic guidance to opacify the collecting system. Over distension of the collecting system may cause extravasation and mucosal changes, potentially obscuring small or flat lesions.
Obtaining an adequate biopsy specimen is paramount to accurately diagnosing upper urinary tract tumors and crafting a treatment plan. Papillary tumors are best biopsied with a flat-wire 2.4 Fr stainless steel Segura basket (Boston Scientific, Natick, MA). The flexible ureteroscope is withdrawn with the engaged specimen under vision, as extracting the basket through the working channel of the ureteroscope will shear off specimen (Fig. 25.8). For large and vascular lesions, it is often helpful to first coagulate the tumor base with laser energy or electrocautery to minimize hematuria associated with the biopsy. Flat lesions are biopsied with a cup biopsy forceps (Piranha biopsy forceps, Boston Scientific, Natick, MA) with the small specimens prepared and evaluated using cytologic cell block technique [4]. Obtaining a barbotage specimen of saline obtained thru the working channel of the endoscope after biopsy will increase the sensitivity of the cytologic evaluation [5].
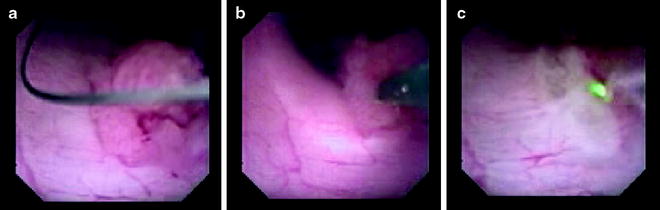
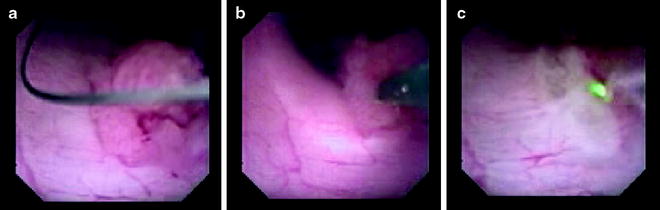
Fig. 25.8
A 2.4 Fr basket is placed around the tumor (a). The tumor is pulled free and the tumor, basket, and ureteroscope are withdrawn down the ureter as a unit (b). The tumor base is then coagulated using holmium laser energy (c)
Once an ureteroscopic biopsy has been performed, tumor therapy can proceed in the appropriate setting. The indications for ureteroscopic therapy have broadened with the best results in those with modest sized, lower grade lesions [6, 7]. Ureteroscopic resection of an upper urinary tract urothelial lesion is performed with either electrocautery or laser energy, with the intent to remove all visible tumor. Small caliber 2 Fr electrocautery electrodes are employed to both resect and coagulate lesions. Holmium laser energy is an efficient means of clearing papillary tumor fronds, employing low power setting of 0.6 J and frequency of pulsation of 5 Hz to coagulate small bleeding sites as tumor is ablated. ND:YAG (neodymium) laser energy can be employed simultaneously with holmium to obtain deeper tissue coagulation. Twenty watts of Nd:YAG power for 15–20 s will both coagulate and also cause deeper tissue necrosis as compared to holmium, and as such should be used with caution in the ureter in light of a relatively high risk of subsequent structure [8]. Staged ureteroscopic resection is employed commonly for large tumors, and to help facilitate topical therapies.
Postoperative ureteral stenting is employed after ureteroscopic tumor therapy based in part on the complexity of the procedure and the volume of tumor treated. In cases where active dilation was employed for access, or when an intrarenal chemotherapy is planned, a ureteral catheter is placed at the termination of ureteroscopic therapy.
Ureteroscopic Lithotripsy
Flexible ureteroscopic lithotripsy is a common therapy for upper urinary tract calculi, and is particularly useful for extracorporeal shock wave (ESWL) failures and in those patients who are not candidates for the more invasive percutaneous nephrostolithotomy (PCNL). Ureteroscopic lithotripsy can be employed for various stone compositions, often irrespective of size. Ureteroscopic lithotripsy is useful in treating complex presentations including the morbidly obese, those with uncorrectable bleeding diathesis or on chronic anticoagulation, or patients with other comorbidities limiting their ability to tolerate more invasive procedures. A relative contraindication to flexible ureteroscopic lithotripsy is active pyelonephritis, potentially with pyonephrosis, where primary drainage and staged endoscopic lithotripsy are the best course.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







