Chapter 90C Extended hepatic resections for biliary tumors
An alternative approach
Preoperative Diagnosis and Management of Hilar Cholangiocarcinoma
Accurate preoperative staging using extensive investigation is indispensable prior to radical resection for hilar cholangiocarcinoma (Nagino et al, 1998; Nimura, 1994, 1997; Nimura et al, 1990a, 1995b, 2000). Most cases of hilar cholangiocarcinoma are associated with jaundice as a result of obstruction of the proximal bile ducts, either within or outside of the liver. Obstruction usually involves multiple ducts as a result of proximal spread of carcinoma along the intrahepatic segmental bile ducts. Multiple applications of PTBD (Nagino et al 1992; Nimura et al 1995a; Takada et al 1976) to relieve the cholestasis and restore the functional reserve of the future remnant liver, we believe, is essential prior to operation involving extensive hepatic resection.
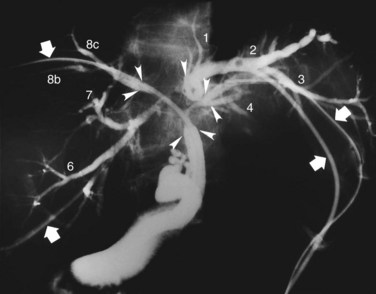
In the third edition of this text, we explained that the first step in the preoperative management of hilar cholangiocarcinoma was PTBD; however, MDCT is taken before biliary drainage to define which side of the liver should be resected, and PTBD applied by the direct anterior approach under fluoroscopic guidance (Takada et al, 1976) or ENBD for the future liver remnant (FLR) are selected to relieve cholestasis of the FLR. This offers both diagnostic and therapeutic advantage (Nagino et al, 1995a), and it minimizes PTBD sessions and the number of PTBD catheters. On the other hand, magnetic resonance cholangiopancreatography (MRCP) is occasionally insufficient to diagnose the difficult local anatomy of the separated intrahepatic segmental and/or sectoral ducts and to design an appropriate operative procedure, especially in patients with Bismuth type III or IV tumors (Bismuth & Corlette, 1975). In such cases, high-quality cholangiograms through the PTBD catheters, taken in various positions—supine, right and left anterior oblique, right and left lateral, and cephalad-anterior-oblique positions (Kamiya et al, 1994)—often clearly demonstrate the tumor location and provide the most reliable information on the proximal extension of hilar cholangiocarcinoma along the intrahepatic segmental bile ducts (Ebata et al, 2002; Sakamoto et al, 1998; Fig. 90C.1).
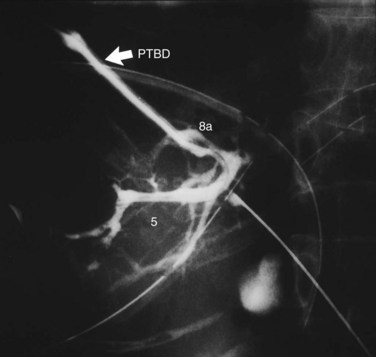
When cholangiography provides insufficient information on the tumor extent, additional PTBD is performed to the undrained bile ducts. After dilating the sinus tract of PTBD, percutaneous transhepatic cholangioscopy (PTCS) can also provide reliable information on anatomic variations of the biliary tree and mucosal extension of the cancer (Kamiya et al, 1994; Nimura, 1993; Nimura et al, 1989). Superficial mucosal extension of the carcinoma is often associated with polypoid and/or nodular tumors of a macroscopic type (Igami et al, 2009). Thus PTCS or per oral cholangioscopy with biopsy may be valuable in diagnosis of the extent of cancer (Itoi et al, 2000, 2007; Nimura et al, 1988; Sakamoto et al, 1997). On the other hand, coexistence of biliary tract infection negatively affects the functional reserve of the liver. When intrahepatic segmental cholangitis develops, even in patients with PTBD catheters during preoperative period, urgent additional selective PTBD to the affected segmental duct should be performed (Kanai et al, 1996; Fig. 90C.2).
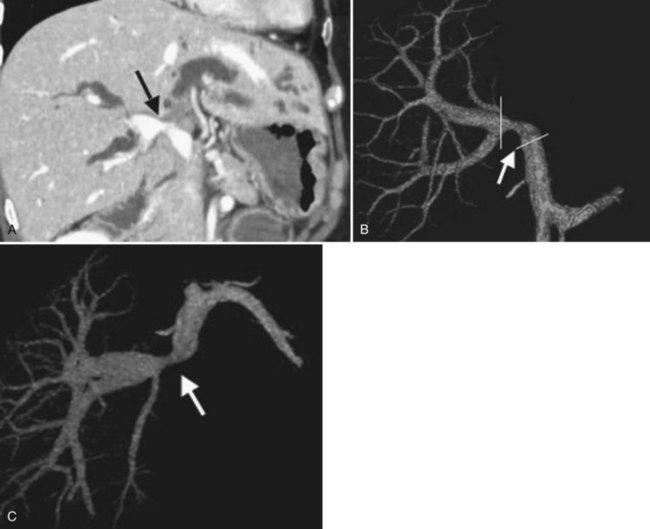
Concomitant vascular resection and reconstruction is indicated in some advanced cases of hilar cholangiocarcinoma (Nimura et al, 1991). We previously performed visceral angiography, percutaneous transhepatic portography, and selective retrograde hepatic venography to assess the vascular invasion of the tumor (Nishio et al, 1999, 2003). Recently, three-dimensional images of MDCT using techniques of volume rendering, multiplanar reformation, and maximum intensity projection have taken over because of the high-quality images and reduced invasiveness (see Fig. 90C.13). We usually estimate the relationship between a tumor and the vascular system in the liver and hepatoduodenal ligament and diagnose the vascular involvement of the tumor on the multiplanar reformatted images; we plan the methods of resection and reconstruction—wedge or segmental resection, direct end-to-end anastomosis, or segmental auto vein grafting—by volume-rendered images and maximum-intensity projection images (Senda et al, 2009; Sugiura et al, 2008).
Postoperative morbidity and mortality rates remain considerable, particularly if extensive resection is necessary (Nagino et al, 2001). Postoperative liver failure sometimes occurs and results in death. For this reason, liver resection is usually scheduled only after the liver has been decompressed and the serum total bilirubin concentration falls below 2 mg/dL. In addition, since 1989, we have routinely performed percutaneous transhepatic portal vein embolization (PVE) (Nagino et al, 1993, 1996, 2000, 2006a) as preoperative preparation for extensive liver resection. This is done to minimize the incidence of postoperative liver failure. After estimation of the resultant compensatory hypertrophy by volumetric CT scan (Nagino et al, 1995b, 1995c) and of the functional reserve of the liver as assessed by the indocyanine green clearance rate (Uesaka et al, 1996), hepatectomy is performed, usually 2 to 3 weeks after PVE. A Japanese series implemented a management strategy for patients with hilar cholangiocarcinoma that consisted of preoperative biliary drainage, PVE, and major hepatobiliary resection; it reported a 0% mortality rate in more than 100 consecutive cases (Sano et al, 2006).
Impaired intestinal barrier function does not recover with PTBD without bile replacement, which can restore the intestinal barrier function during external biliary drainage in patients with biliary obstruction, primarily as a result of repair of physical damage to the intestinal mucosa. Thus, in patients with hilar cholangiocarcinoma and external biliary drainage, we routinely replace bile prior to operation (Kamiya et al, 2004; Kanazawa et al, 2005). Also, perioperative administration of synbiotics can enhance immune responses, attenuate systemic postoperative inflammatory responses, and improve the intestinal microbial environment (Sugawara et al, 2006). These procedures may reduce postoperative infectious complications after major hepatobiliary resection in difficult patients with hilar cholangiocarcinoma.
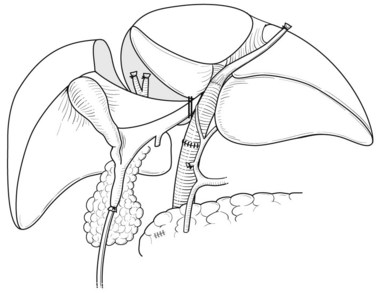
Right Hepatic Resection with Total Caudate Lobectomy, Extrahepatic Bile Duct Resection, and Portal Vein Resection and Reconstruction
Right hepatectomy with total caudate lobectomy is carried out for tumors involving the right anterior and posterior sectoral bile ducts, with sparing of the left medial segmental bile duct to segment IV, or when the right hepatic artery is also involved (see Chapters 50B and 90B). If the cancer involves the right hepatic duct and the left medial segmental duct, anatomic right hepatic trisectionectomy with caudate lobectomy is indicated (Nagino et al, 2006b).
After retropancreatic lymph node dissection, the distal bile duct is divided above the pancreas with a histologic free margin; the hepatoduodenal ligament is dissected, and the vessels are skeletonized and removed (Bhuiya et al, 1992). The middle hepatic artery usually runs ventral to the left portal vein and enters the liver below the left medial segment branch of the portal vein; this artery is carefully preserved. The left hepatic artery enters the liver to the left of the umbilical portion of the portal vein (Figs. 90C.3 to 90C.5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree