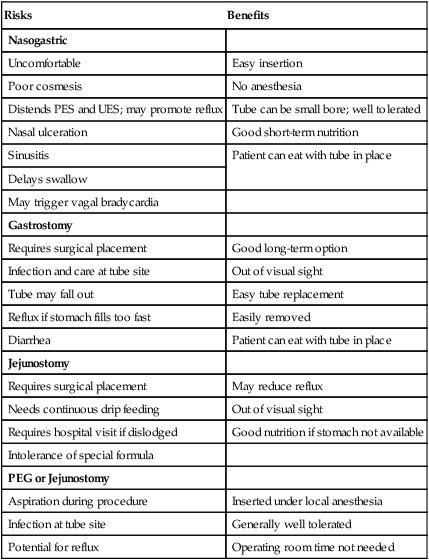
1. Present the basic principles of medical ethics as they relate to the swallowing-impaired patient. 2. Discuss the risks and benefits of alternative types of feeding. 3. Highlight the differences between factors that predict aspiration and those that predict aspiration pneumonia. 4. Present an approach for weaning from feeding tubes. 5. Present examples of ethical dilemmas resulting from the placement or retention of alternative forms of feeding. The Patient Self-Determination Act took effect on December 1, 1991. The act established guidelines to allow patients to participate fully in decisions regarding their health care, particularly decisions made in circumstances of severe or terminal illness. The act strives to establish a patient-physician interaction that allows both parties to balance individual morals and values against the known risks and benefits of proposed medical care. For example, patients might want to decide under which circumstances they would want to be resuscitated or whether they would want to be nourished by a feeding tube to sustain life. Counseling patients, families, and caregivers on the risks and benefits of tube feeding may involve the expertise of the dysphagia specialist.1 One study found that speech-language pathologists (SLPs) who manage patients with dementia are involved in the decision making in 65% of cases when the recommendation is made for some type of alternative nutrition.2 The gastrostomy tube is placed directly into the stomach with the assumption that the digestive processes of the stomach are intact. Formula is passed through a catheter that sits on the outside of the stomach. If the stomach is not functioning, the feeding tube may need to be placed into the jejunum of the small intestine. Because the stomach is bypassed, specialized, predigested formulas are required for jejunal tube feedings. Some clinicians argue that jejunal placement reduces the risk of reflux of the tube-fed material into the pharynx because the pyloric valve provides an additional barrier to retropulsion of stomach contents into the esophagus. However, the experimental evidence does not clearly support this contention.3 Table 15-1 summarizes the medical risks and benefits of enteral tube feeding. TABLE 15-1 Medical Risks and Benefits Associated with Enteral Tube Feeding PES, Pharyngoesophageal segment; UES, upper esophageal sphincter. Parenteral nutrition is indicated when the gastrointestinal tract cannot be used because of medical complications such as gastroparesis, obstruction, or bleeding. Total parenteral nutrition (TPN) is a specialized formula that most commonly is delivered into a central vein (subclavian or internal jugular). Although there are potential medical complications from this therapy, such as pneumothorax, patients can be supported nutritionally with this formula for 4 to 6 weeks if necessary.4 Peripheral parenteral nutrition (PPN) is a form of nutritional support delivered through a peripheral vein. Because of potential medical complications, this therapy can be used effectively for only 7 to 10 days.4 Intravenous feeding is a common form of parenteral nutrition, usually providing hydration and medication only rather than more complex elements such as amino acids. Hypodermal clysis is a form of parenteral nutrition that is given for hydration through the subcutaneous tissues in the chest, thigh, or abdomen. Table 15-2 summarizes parenteral and enteral alternative nutrition and hydration. TABLE 15-2 Summary of Potential Methods of Providing Nutrition
Ethical Considerations
MEDICAL ETHICS
TUBE FEEDING
Enteral Nutrition
Gastrostomy and Jejunostomy Tubes
Risks
Benefits
Nasogastric
Uncomfortable
Easy insertion
Poor cosmesis
No anesthesia
Distends PES and UES; may promote reflux
Tube can be small bore; well tolerated
Nasal ulceration
Good short-term nutrition
Sinusitis
Patient can eat with tube in place
Delays swallow
May trigger vagal bradycardia
Gastrostomy
Requires surgical placement
Good long-term option
Infection and care at tube site
Out of visual sight
Tube may fall out
Easy tube replacement
Reflux if stomach fills too fast
Easily removed
Diarrhea
Patient can eat with tube in place
Jejunostomy
Requires surgical placement
May reduce reflux
Needs continuous drip feeding
Out of visual sight
Requires hospital visit if dislodged
Good nutrition if stomach not available
Intolerance of special formula
PEG or Jejunostomy
Aspiration during procedure
Inserted under local anesthesia
Infection at tube site
Generally well tolerated
Potential for reflux
Operating room time not needed
Parenteral Nutrition
Type of Nutrition Delivery
Route of Delivery
Method of Delivery
Indications for Use
Types of Formula
Possible Complications
Simple IV/CTPN
IV (small vein; catheter inserted or surgically placed for CTPN in deep central vein)
Continuous or cyclic infusion by pump
Supplemental hydration; restoration of fluid and electrolyte balance, need for complete parenteral nutrition or long-term CTPN
Nasogastric tube
Catheter/tube placed transnasally to the stomach
Intermittent or continuous drip by pump
Short-term alternative to oral intake (approximately 2 weeks); transnasal insertion, easily removed
Commercial nutritionally complete (standard, hydrolyzed, modular) supplements; regular liquids
Misplacement into the airway; irritation to nasal, pharyngeal, esophageal mucosa; discomfort; negative cosmesis; may affect swallow function; may contribute to reflux and aspiration
G-tube/PEG
Feeding tube inserted directly into the stomach
Bolus or gravity (syringe); drip by infusion pump
Option for long-term alternative to oral intake; does not necessarily preclude oral intake in certain cases
Commercially prepared nutritionally complete enteral formulas; fiber supplements, supplemental and regular liquids, select medications; some individuals may liquefy table foods
Nausea, vomiting, diarrhea, constipation, reflux, clogged tube, skin irritation at gastrostomy site; aspiration
J-tube/PEG
Feeding tube inserted directly into the jejunum (small intestine)
Bolus or gravity syringe; drip by infusion pump
Does not require stomach for digestion; allows enteral nutrition earlier after stress or trauma; less risk of reflux and aspiration
Commercial prepared nutritionally complete enteral formulas; fiber supplements, supplemental liquids
Loss of controlled emptying of the stomach; misplacement; diarrhea, dehydration
Hypodermal clysis
Subcutaneous; common infusion sites are the chest, abdomen, thighs, and upper arms
Injection (3 L in 24 hours/two sites)
Hydration supplement for mild to moderate dehydration
Saline; half saline/glucose; potassium chloride can be added
Mild subcutaneous edema ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ethical Considerations






